Abstract
Aims: Whether or not primary percutaneous coronary intervention (P-PCI) is equally effective and safe in women and men in a real world setting is still a matter of debate. The aim of this study was to evaluate the effect of gender on in-hospital outcome after P-PCI for ST-elevation myocardial infarction (STEMI) in a prospective national registry.
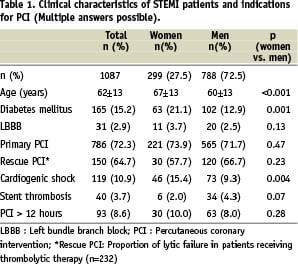
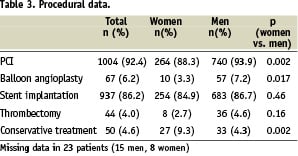
Methods and results: This registry includes in-hospital outcome data from 19 PCI-performing hospitals. During 12 months, 1087 patients with STEMI were registered (mean age 62±13 years; 27% women). Women were older than men (67±13 vs. 60±13 years; p<0.001) and more often had diabetes mellitus (21% vs. 13%; p<0.001) or cardiogenic shock (15% vs. 9%; p=0.004). PCI was performed in 1004 patients (92.4%) and more frequently in men than in women (93.9 vs 88.3%, p=0.002), whereas conservative treatment was more often decided in women (9.3% vs 4.3%; p=0.002). No differences were found between women and men in primary success rate (TIMI 2+3 flow, 92.9% vs. 93%; p=0.96). On univariate analysis, in-hospital mortality was higher in women than in men (13.7% vs. 7.2%; p=0.001). On multivariable analysis age, shock, diabetes and TIMI flow before PCI remained associated with mortality.
Conclusions: Women have higher in-hospital mortality following PCI for STEMI. On multivariate analysis age, shock, diabetes and TIMI flow, but not gender, were associated with mortality in this national register. Older age and more comorbidity are likely to explain the higher mortality in female patients undergoing P-PCI.
Introduction
Gender-related differences in outcome after acute coronary syndromes (ACS) have gained increasing attention over the past decade. Studies in the thrombolytic era have shown that women have worse outcome than men after acute myocardial infarction1-4. After adjusting for age and other risk factors at baseline, differences in mortality were no longer present in further investigations5-10. Covariables influencing outcome in women after thrombolytic therapy include older age2,5,6,11, diabetes mellitus2,4,6,11, hypertension2,4, congestive heart failure2,4, and longer delays between symptom onset and treatment12,13.
Primary PCI has become the preferred reperfusion modality for patients with ST-elevation myocardial infarction (STEMI) in recent years. Data on differences in outcome between men and women after primary PCI are conflicting and mostly derived from randomised trials10,14,15, whereas few data from registries have been reported thus far.
In the present era of primary PCI as the predominant reperfusion therapy for STEMI, more information is warranted on whether this treatment strategy is similarly useful and safe in women and men in the real world setting. One major contribution of registries to the evidence regarding new treatment modalities is the inclusion of unselected, consecutive patients.
The Austrian acute PCI registry was initiated to obtain procedural and in-hospital outcome data in patients treated with PCI within 24 hours of an acute coronary syndrome from major PCI hospitals in Austria. The aim of the present study was to evaluate the effect of gender on in-hospital outcome in patients with STEMI in uni- and multivariate analyses.
Methods
Nineteen of 29 Austrian hospitals with PCI facilities participated in the registry. Patients were enrolled if they underwent acute coronary angiography with or without subsequent PCI within 24 hours of symptom onset of a suspected acute coronary syndrome (ACS). Thus, patients were included with either STEMI or non-ST-elevation myocardial infarction (NSTEMI). The latter were included if they could not be stabilised with maximal medical therapy. Data entry was performed using a web-based case report form (CRF). The study protocol was in accordance with the Declaration of Helsinki. For this analysis, only patients with STEMI were included.
Acquired data
A three digit code was used for identification of the participating centre. Patient data was made anonymous by entering the initials, sex and age.
The CRF included the following data variables, in accordance with the definitions of the recently published Cardiology Audit and Registration Data Standards17:
1. Baseline characteristics included age, sex and known diabetes mellitus.
2. Mode of hospital admission (in-hospital, transfer from peripheral hospital by ambulance or by helicopter, direct transport to PCI hospital by ambulance or by helicopter, patient comes on his/her own).
3. Times: date and time of arrival in the cath lab, door-to-balloon time, date and time of symptom onset.
4. Pre-treatment: fibrinolysis, glycoprotein IIb/IIIa antagonist (abciximab, eptifibatide or tirofiban) or no pre-treatment before reaching the cardiac catheterisation laboratory were recorded.
5. Indications for acute PCI included primary PCI, lytic failure/ rescue PCI, PCI>12 hours after symptom onset, NSTEMI not stabilised by maximal medical therapy, stent thrombosis, and cardiogenic shock, defined as persistent systolic blood pressure < 90 mmHg, or requirement of inotropes or intra-aortic balloon pump to support circulation18.
6. Procedural parameters: target vessel, PCI device or therapy, TIMI flow and visual %-diameter stenosis before and after the intervention and the use of intra-aortic balloon pump.
7. ECG diagnosis (STEMI, anterior or posterior wall, NSTEMI, left bundle branch block), cardiac enzymes (CK, CK/MB, troponin I or T).
8. In-hospital outcome: uneventful discharge, death, reinfarction, other (e.g. transfer in peripheral hospital).
Definitions of myocardial infarction
A myocardial infarction was recorded as STEMI if the ECG revealed new or presumably new ST-elevations in two or more contiguous leads (at least 0.2 mV in V1 to V3 or at least 0.1 mV in remaining leads) or if ECG showed a new left bundle branch block.
Statistical analyses
A p-value<0.05 was considered statistically significant. Normal distribution of variables was assessed using Kolmogorov Smirnov test. Because all continuous variables included in analysis were normally distributed, Student t test was used for comparing these variables. Differences between categorical variables were compared using chi-square or Fisher-exact test, as appropriate. Stepwise logistic regression was used for analysis of the independent influence of different parameters on mortality. All analyses were performed with the use of SPSS® software.
Results
Between November 2003 and October 2004, a total of 1,087 patients were registered with STEMI according to the qualifying ECG (788 men, 72.5% and 299 women, 27.5%). Mean age was higher in women than in men (67±13 vs. 60±13 years, p<0.001). Among 165 known diabetics (15%), there were more women than men (21 vs 13%, p=0.001). A left bundle branch block was found in 31 patients (2.9%). (Table 1)
Pretreatment
Thrombolytic therapy before PCI was administered in 232 patients (21.3%). Less use of thrombolytic therapy was found in women (17.4 vs 22.8%, p=0.05). A glycoprotein IIb/IIIa antagonist was administered to 166 patients (15.3%). The use of glycoprotein IIb/IIIa antagonists prior to PCI was similar in women and men (15.7 vs. 15.1%, p=0.8).
PCI indications
Cardiogenic shock was present in 119 patients (10.9%) and more often so in women than in men (15.4 vs. 9.3%, p=0.004). Rescue PCI was the indication in 64.7% of all patients receiving thrombolytic therapy. The rate of lytic failure between gender was similar (57.7 vs. 66.7%, p=0.23). A tendency towards more stent thrombosis as indication for PCI was found in men (4.3 vs. 2.0%, p=0.07). (Table 1)
Time delays
Door-to-balloon time was below two hours in 783 patients (72%), between two and four hours in 128 patients (11.8%). Door-to-balloon time was available for analysis in 911 patients (83.8%). The mean door-to-balloon time for primary PCI was 65±42 minutes. No differences in door-to-balloon times between men and women were found (61±43 vs 68±48 minutes, p=0.11). The mean pain-to-catheter time was 355±339 minutes, with no differences between women and men (336±300 vs 361±352 minutes, p=0.89).
Target vessels
The left anterior descending artery was the target vessel in 48.5%, right coronary artery in 37.4%, circumflex artery in 10.8%, left main artery in 0.9%, diagonal branch in 0.9%, intermediate branch in 0.7% and bypass graft in 0.5% of patients. In 0.2% no target vessel was found and in 0.1% information on target vessel was not available. Target vessels were similar in men and women.
TIMI flow
The primary success rate (defined as TIMI flow 2 + 3) was 92.9%. No differences in TIMI flow before or after PCI were found between women and men. Specifically, the frequency of TIMI 3 (82.9 vs 85.3%, p=0.32) and TIMI 2+3 (93% vs 92.9%, p=0.96) was not different in women versus men (Table 2).
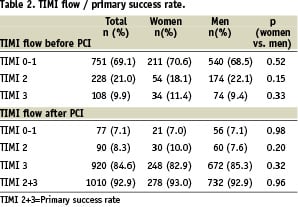
Mean percent diameter stenosis of the culprit vessel was similar in both genders before (91.4 vs 93.7%, p=0.49) and after PCI (10.3 vs 10.6%, p=0.2).
Intervention/therapy
PCI was performed in 1,004 patients (92.4%) with STEMI. Among these, balloon angioplasty (PTCA) alone was performed in 67 patients (6.2%) and stent implantation in 937 patients (86.2%). A thrombectomy was done in 39 patients with stent implantation and in five patients with PTCA alone. Conservative treatment was decided in 60 patients (5.5%). PCI was more frequently performed in men vs. women (93.9 vs. 88.3%, p=0.002). The rate of stent implantation was similar between men and women (86.7 vs. 84.9%, p=0.46). Conservative treatment was decided more often in women (9.3 vs. 4.3%, p=0.002). In 23 cases (2.1%) data was missing for intervention/therapy. (Table 3)
Outcome
Eight hundred ninety patients (81.9%) were discharged without an event. In-hospital death occurred in 98 patients (9.0%). After excluding patients with shock, mortality was 5.1% (n=49). In-hospital mortality of patients with cardiogenic shock was 41.2% (n=49). After exclusion of diabetic patients, in-hospital mortality was 5.3% (n=42), whereas the presence of diabetes was associated with a mortality of 15.8% (n=26). In 18 patients (1.7%) urgent CABG was decided after angioplasty. In 7.9% of patients (n=86), outcome was not specified.
Gender differences in outcome
Gender differences in outcome were found in mortality and uneventful discharge: women had a higher in-hospital mortality (13.7 vs 7.2%, p=0.001; Figure 1).
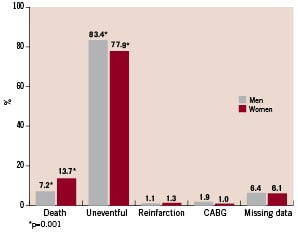
Figure 1. Difference in in-hospital outcome between women and men; a difference was found in death and uneventful discharge.
There was a higher mortality in women versus men when they were in shock (54.3 vs 32.9%, p=0.01). In diabetics a tendency towards higher mortality in women was found (22.2 vs 11.8%, p=0.09). After exclusion of either shock or diabetic patients, no gender difference in in-hospital mortality was seen.
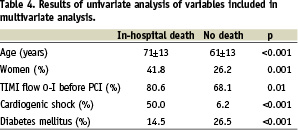
On univariate analysis, patients who died were older (71±13 vs 61±13 years, p<0.001), more often had TIMI flow O-I (80.6 vs 68.1%, p=0.01) before PCI, and after PCI TIMI III flow in a lower percentage (57.1 vs 87.1%, p<0.001). No differences in cardiac enzyme levels were found in patients who died compared to survivors. By analysing mortality according to door-to-balloon times, a door-to-balloon-time <2 hours (n=783) was associated with a mortality of 8.7%, 2 to 4 hours (n=128) with a mortality of 8.6%. Differences in mortality between men and women were found in the groups with a door-to-balloon time <2 hours (7.3% vs 12.2%, respectively, p=0.03); in patients with a door-to-balloon time between two and four hours no significant difference in mortality was found (6.9% vs 14.8%, respectively, p=0.2).
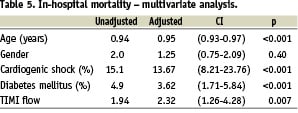
Predictors of mortality
Using stepwise logistic regression analysis including age, gender, cardiogenic shock, diabetes mellitus, TIMI flow, the strongest predictor of mortality was the presence of cardiogenic shock, followed by diabetes mellitus and TIMI flow. Gender was not independently associated with mortality (Table 5).
Discussion
In this registry of PCI performed within 24 hours of symptom onset of a STEMI, women had a higher in-hospital mortality on univariate analysis. After correcting for age, the presence of diabetes mellitus and cardiogenic shock, gender was no longer associated with mortality. Therefore, our data suggest that mechanical reperfusion therapy in STEMI is similarly effective in women and men in the real-world practice of primary PCI, but that age and comorbidity may be higher in women presenting with these syndromes.
Gender and outcome
Many studies have suggested that women have a worse prognosis after acute coronary syndromes in general and after reperfusion therapy for STEMI in particular6,11,20. In the present study, the question of potentially different outcomes in men and women receiving interventional reperfusion/early invasive therapy was reassessed in a non-selected patient cohort undergoing PCI within 24 hours of acute STEMI. The outcome was not influenced by non-accessibility to or eligibility for reperfusion but rather the invasive/interventional approach itself.
Previous studies in the era of primary PCI for STEMI showed controversial results: A retrospective analysis of patients undergoing primary PCI for AMI in the New York State Coronary Angioplasty Registry demonstrated a higher in-hospital mortality rate in women in univariate as well as multivariate analyses19. In contrast, Mehilli et al found a similar outcome for women compared to men after reperfusion therapy based in large part on PCI20. Antoniucci et al7 showed that the 6-month mortality rate was higher in women vs men (12% vs 7%) after primary PCI. In multivariate analysis, however, gender did not emerge as a significant variable. Similar findings were reported by Azar et al8. Discrepancies in the results of these studies may partially relate to rapidly changing techniques including drug eluting stents, adjunctive medical therapy and to a change in the characteristics of patients included. Furthermore, randomised trials comparing mechanical reperfusion with thrombolytic therapy10,15,21 excluded high-risk patients and may not adequately reflect outcomes that can be expected for patients treated in daily practice. Therefore, the important incremental information from registries is whether a given therapy is as effective and safe in unselected consecutive patients as in randomised cohorts.
Gender and therapeutic strategies
Our data suggest a lower rate of interventional therapeutic strategy used in women, which is in accordance with previous data16. The reason for this more conservative treatment strategy used in women cannot be fully explained, but may relate to more extensive and/or diffuse disease in women as well as to smaller vessels in general, making PCI less of an option. Furthermore, the conservative treatment decision in women may be influenced by the higher age in this group.
Time delays
Some studies showed that women have longer in-hospital delays than men, which may contribute to worse prognosis22,23. In our study, no difference in the mean door-to-balloon times between gender was found, which is in accordance with data from the AMI-Florence registry16. When dividing patients into two subgroups according to door-to-balloon times <2 hours and 2-4 hours, in-hospital mortality was lower in men versus women in the group (n=783) with a door-to-balloon time <2 hours (7.3 vs 12.2%, respectively, p=0.03). In the second group (n=128) with door-to-balloon times between two and four hours, no gender difference in mortality remained. The higher mortality in women with door-to-balloon times <2 hours may relate to the higher comorbidity in women, which may have more impact in the “early” versus the “late” population. This possible selection bias towards less sick patients among late-comers is an effect not infrequently seen in registries, which may mask true disadvantages of longer treatment delays.
Mortality
Total in-hospital mortality was 9%. This seemingly high overall mortality may be partially explained by the high proportion of patients with cardiogenic shock (10.9%), but is in accordance with other registries16,24. After exclusion of patients with cardiogenic shock, mortality was 5.1%.
Limitations
There are some important limitations in our study: first, the patients´ baseline characteristics do not include complete risk factor profiles. This is due to the restriction of a limited number of data in this countrywide registry involving 19 hospitals. Second, for the same reason, recording of pre-hospital times was restricted to the onset of pain from which the pain-to-catheter time was calculated. In-hospital delay was recorded as door-to-balloon times. Therefore, we cannot exclude that women, as reported in previous studies, presented later than men. Third, as in most registries, no external monitoring was performed for data validation. Finally, this is an observational study that reflects the practice of PCI patients undergoing PCI for STEMI and does not address the general population receiving any reperfusion therapy.
Conclusion
Women had a higher in-hospital mortality after PCI for STEMI. After adjustment for age, shock, diabetes and TIMI flow, this difference was no longer present. We conclude that higher comorbidity and age, but not worse acute procedural success rates, are likely to explain the higher mortality in women after PCI within 24 hours of STEMI. While the reason for higher comorbidity in women presenting with acute myocardial infarction is not readily explained, more prospective studies are needed to further evaluate specific outcome predictors in men versus women after PCI in STEMI.
Acknowledgements
Participants in the Austrian Acute PCI Registry: Wolfgang Tkalec, MD, Christian Ebner, MD, Josef Aichinger, MD, Elisabethinen Hospital, Linz; Johann Altenberger, MD, Matthias Heigert, MD, Maximilian Pichler, MD, Paracelsus University Salzburg; Werner Benzer, MD, Wolfgang Schöbel, MD, Tomas Banerjee, MD, Academic Hospital Feldkirch; Thomas Brunner, MD, General Hospital Wiener Neustadt; Guenter Christ, MD, Stefan Ingerle, MD, Dietmar Glogar, MD, Medical University Vienna; Edwin Maurer, MD, Johann Auer, MD, Thomas Weber, MD, General Hospital Wels; Georg Gaul, MD, Hanusch Hospital Vienna; Lukas Ameri, MD, Sebastian Globits, MD, Harald Mayr, MD, General Hospital St. Poelten; Georg Grimm, MD, Kornelia Laubreiter, MD, Hospital Klagenfurt; Herwig W. Schuchlenz, MD, Stefan Harb, MD, Dieter Botegal, MD, General Hospital Graz-West; Maximilian Juhasz, MD, Gerald Ohrenberger, MD, Josef Rieschl, MD, Hospital Barmherzige Brueder Eisenstadt; Ronald Karnik, MD, Gerhard Bonner, MD, Jörg Slany, MD, Rudolfsstiftung, Vienna; Klaus Kerschner, MD, Clemens Steinwender, MD, Franz Leisch, MD, General Hospital Linz; Heinz Koller, MD, Hospital Villach; Horst Kratzer, MD, Peter Siostrzonek, MD, Hospital Barmherzige Schwestern Linz; Franz Gremmel, MD, L. Mayerhofer, MD, Heinrich Weber, MD, Donau Hospital Vienna; Gerhard Unger, MD, Ilyas Kozanli, MD, Karim Kalla, MD, Wihelminen Hospital Vienna; Franz Gratze, MD, Robert Tischler, MD, Klaus Kaspar, MD, Hospital Bruck; Nico Moes, MD, Guy Friedrich, MD, Florian Hintringer, MD, University Hospital Innsbruck.
We thank Prof. Hanno Ulmer, PhD, and Verena Barbieri for their help in the statistical analyses and Prof. Volker Mühlberger for his comments and suggestions. We are indebted to all nurses and radiology technicians for their help in the data collection.

