Abstract
Aims: To evaluate in-hospital and long-term outcome of women undergoing percutaneous coronary intervention (PCI) with paclitaxel-eluting stents (PES) as compared to men and historic controls treated with bare metal stents.
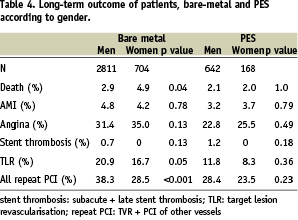
Methods and results: Eight-hundred and ten (810) consecutive patients (642 men and 168 women) with PES were analysed and also compared with 3,515 patients (2,811 men and 704 women) with at least one bare metal stent in the three years previous. In the PES group, women were significantly older than men (mean age of 68±10 vs. 63±10 years, p<0.001), with more diabetes (39.9 vs. 29.7%, p<0.05), smaller treated vessels (<2.5 mm in 34.9 vs. 24.8%, p=0.003), more left-anterior descending lesions (56.6 vs. 43.2%, p<0.001). More men had multivessel disease (78.8 vs. 62.5%, p<0,001), dyslipidaemia (73.2 versus 65.4%, p<0.05), smoking habit (74.3 versus 34.5%, p<0.001) or prior revascularisation (49.7 versus 36.1%, p<0.05). Compared to bare metal stents, similar higher risk features were recorded in women over time. No gender specific differences in in-hospital outcome were observed. At 12 months the rates of cardiac death, acute myocardial infarction (AMI) and late thrombosis were respectively 2.0%, 3.7% and 0% in women and 2.1%, 3.2%, and 1.2% in men (all p=NS).
Conclusions: Albeit with worse baseline clinical and angiographic characteristics in women, very high immediate success rates and a positive outcome can be achieved in both sexes after PES.
Introduction
Women undergoing percutaneous coronary intervention (PCI) are generally at higher risk than men, because of worse baseline clinical and angiographic characteristics1. Atherosclerosis affects older women more than men, with a high prevalence of diabetes and smaller, more diseased coronary vessels2. Different combinations of such risk factors are associated with higher rates of restenosis and target lesion revascularisation (TLR) after PCI3. Paradoxically, several studies have reported a higher periprocedural hazard in women4,5, but similar, long-term clinical outcomes (the so-called “gender paradox” of restenosis)6-8. Drug eluting stents (DES) are very effective in reducing restenosis rates, especially in high-risk lesions. Very few studies have specifically addressed their relative efficacy and safety in women9,10. We describe in-hospital and long term outcomes in a consecutive series of women treated with the paclitaxel-eluting stent (PES), as compared to men. To explore temporal trends, outcome according to gender was also evaluated in historic controls treated with bare-metal stents.
Materials and methods
Patient population
Clinical and procedural data of patients undergoing PCI at the Istituto Clinico Humanitas (ICH) are entered in the Invasive Cardiology Database, which includes clinical, laboratory and procedural characteristics together with clinical or angiographic follow-up information as it becomes available. Data were collected on all patients who received a paclitaxel-eluting stent (Taxus™, Boston Scientific, Inc., Natick, MA, USA) between June 1st, 2003 and December 31th, 2005. Records were identified for analysis of procedural data, in-hospital complications and clinical and angiographic outcome. Our policy to implant a PES has generally been to select patients at higher risk of restenosis (such as diabetics, small vessel disease, total occlusions, or left anterior descending (LAD) lesions), but the decision is ultimately left at the operator’s discretion and judgement. Gender-specific outcome data of patients who received at least one bare metal stent in the three years before the introduction of PES were also collected for analysis.
PCI and adjunct pharmacologic therapy
PCI was performed according to standard clinical practice. All patients received 100 mg of aspirin, to be continued indefinitely, and either 500 mg of ticlopidine or 75 mg of clopidogrel started at least 48 hours before the procedure. Ticlopidine or clopidogrel were maintained for four weeks after bare metal stents and six to 12 months after PES. Intravenous (iv) heparin 100 IU/Kg (maximum 10.000 IU) was given with supplemental doses to achieve an activated clotting time (ACT) > 250-300 sec. Glycoprotein IIb/IIIa inhibitors (with a lower concomitant dose of heparin of 70 U/Kg and the ACT maintained at 200-250 seconds) were administered periprocedurally, either because of unstable symptoms or angiographic evidence of thrombus. Sheath removal in the bare metal-stent group occurred 2-6 hours after the procedure, when the ACT was < 180 sec. In the most recent series of patients sheath removal was usually obtained immediately after the procedure, after reversal of heparin with iv protamine. The procedure was considered successful in the presence of residual < 30% stenosis and Thrombolysis in Miocardical Infarction (TIMI) flow grade 2 or 3. Angiographic restenosis was defined as > 50% diameter stenosis (DS) at the lesion site.
Angiographic complications included: sub-occlusive or occlusive dissection, thrombosis, distal embolisation and vessel perforation or rupture. Peripheral complications included: large haematoma (requiring transfusion), pseudoaneurysm and arteriovenous fistula requiring vascular surgical repair. The diagnosis of myocardial infarction was based on a compatible clinical picture together with either an increase in creatine kinase (CK)-MB serum level > 3 times the upper limits of normal, and/or a ratio of CK-MB/CK > 0.1, and/or new Q waves on the ECG.
Angiographic evaluation
Type B2 and C lesions were considered complex lesions, according to the modified classification of the American Heart Association/ American College of Cardiology. All procedural and follow-up angiograms were analysed off-line with an automated edge-detection system (Philips, Quantitative Cardiac System, Eindhoven,The Netherlands). Multiple matched projections were obtained in each patient after intracoronary injection of 200 mcg of nitroglycerin. Matching “worst views” were analysed with the contrast-filled guiding catheter used as reference for calibration.
Long-term follow-up
Clinical outcome data at follow-up is upgraded every six months via information on new hospital admissions, scheduled office visits or telephone calls. Repeat coronary angiography was performed only because of recurrence of symptoms, silent ischaemia or as part of research protocols. Stent thrombosis was defined as early (0 to 30 days), late (31 to 360 days) or very late (> 360 days) and required angiographic confirmation of thrombotic stent occlusion.
Statistical analysis
Data were described as number and percentage, or mean and standard deviation, as appropriate. Descriptive statistics were calculated using means and standard deviations for continuous variables and percentages for categorical variables. Comparisons between means were performed with Student’s t-test, while percentages were compared with chi-square or non-parametric tests as appropriate. Survival curves were generated with the Kaplan-Meier method. Survival was calculated starting from the day of examination. Possible prognostic factors were subjected to univariate analysis using the Cox proportional hazard model. All variables found to have a p < 0.1 in the univariate evaluation were considered to be candidates for stepwise Cox regression analysis.
All analysis were done using Stata 9 (StataCorp LP, College Station, Texas, USA).
Results
Baseline and procedural characteristics
During the study period, a total of 810 patients (169 women and 642 men) were treated with a PES. For comparison, we also show the tabulated data on 3,515 patients (2,811 men, 704 women) treated with bare metal stents in the three years before. Females represent about one quarter of patients in both series (Table 1).
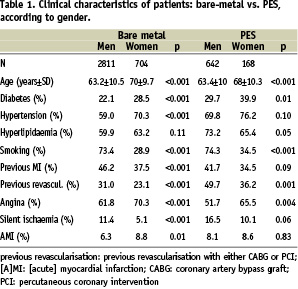
When examining the PES-treated group according to gender, women were significantly older than men (mean age 68±10 vs. 63±10 years, p<0.001). Diabetes was present in up to 39.9% of women but only in 29.7% of men (p<0.05). More men had dyslipidaemia (73.2 versus 65.4%, respectively, p<0.05), were active smokers (74.3 versus 34.5%, p<0.001) and had had prior revascularisation with either PCI or CABG (49.7 versus 36.1%, p<0.05). Table 2 shows some of the angiographic characteristics.
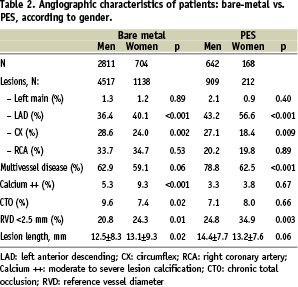
Even though the left anterior descending (LAD) was the most commonly treated artery with PES in both sexes, an imbalance in the prevalence of LAD (56.6 vs. 43.2%, women vs. men, p<0.001) or left circumflex (LCX) treatment (18.4 vs. 27.1%, women vs. men, p< 0.05) was noted. Treatment of an unprotected left main trunk was performed rarely (0.9%) in women and in only 2.1 % in men. Significantly more women (62.5%) than men (78.8%, p< 0,001) treated with PES had multivessel disease. PCI of chronic total occlusions was similar in both groups. The treated vessels were significantly smaller in women than men (mean reference vessel diameter, RVD, of 2.6±0.5 vs. 2.8±0.5 mm, respectively, p=0.02). An RVD < 2.5 mm was present in 34.9% of women as compared to 24.8% of men (p<0.05). Lesions length was similar (13.2±7.6 vs. 14.3±7.7 mm, women vs men respectively)
Procedural and late outcomes
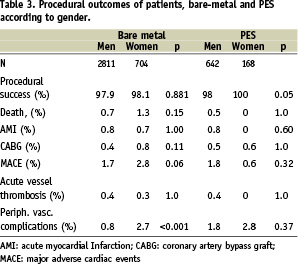
The total number of lesions treated with a PES was 212 in women and 909 in men. Procedural success was above 98% in both groups. Major in-hospital adverse cardiac events (MACE, combined incidence of AMI, CABG or repeat PCI) after PES occurred in 0.6% of women and 1.8% of men (p=0.3). Acute vessel thrombosis was rare, occurring in only three men (0.5%). Peripheral vascular complications were infrequent in both groups (2.8 % in women vs. 1.8 % in men) (Table 3).
Follow-up visits were performed in 80% of patients in the bare metal stent group and in 95% of patients in the PES group. Follow-up ranged between nine to 24 months. At the median follow-up of 11 months (25th-75th percentile seven to 14 months) after PES implantation the rates of cardiac death, acute myocardial infarction and late thrombosis were respectively 2.0%, 3.7% and 0% in women and 2.1%, 3.2% and 1.2% in men (differences not statistically significant). TLR was lower, but not statistically different in women (8.3%) than men (11.8 %, p=0.36, NS) (Table 4).
Angiographic follow-up was limited to only 43% of women and 52% of men (p=0.01). Late loss was similar among the sexes (p=0.48), but again in absolute terms it was lower in women (0.42±0.86 mm) than men (0.52±0.97 mm). The observed restenosis rates after angiography were 13.6% in women and 17.1% in men (p=0.49).
Predictors of target lesion revascularisation
In order to assess predictors of TLR, univariate analysis was performed including clinical and procedural factors known to affect restenosis rates (Table 5A). At multivariate analysis (Table 5B), only small size of the reference vessel (< 2,5 mm) remained as an independent predictor of TLR in women treated with a PES (RR 13.1, CI 2.8 to 61.2, p=0.001).
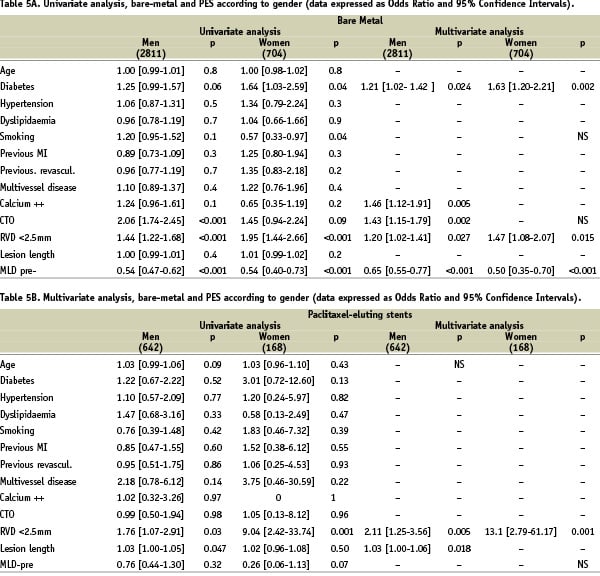
In men, a weaker association was also demonstrated for small vessel size (RR 2.1, CI 1.25 to 3.56, p=0.005) and lesion length (RR 1.03, CI 1.0 to 1.06, p=0.018).
Historic comparison with bare-metal stents
The gap in the incidence of peripheral complications (historically significantly higher in women at 2.7%, vs. 0.8% in men, p< 0.001, after bare-metal stents) narrowed considerably (2.8 % vs 1.8% in women vs. men in the more recent PES population, P=0.4) (Table 3). A reversed trend in the absolute combined incidence of in-hospital MACE (women vs. men: from 2.8 to 1.7%, p=0.006, with bare-metal stent to the current 0.6 vs. 1.8%, p=0.3 in the PES population) was also observed. Angiographic follow-up was available in 50.4% of men and 48% of women after bare-metal stenting. Late loss was similar (0,93±1.1 mm in women and 1.07±1.2 mm in men, p=0.5).
In the larger data set of patients with bare-metal stents, multivariate analysis identified presence of diabetes and small vessel size as independent predictors of TLR in both sexes. However, the relative risk ratios were similar (1.20 in men and 1.47 in women). Presence of severely calcified lesions and treatment of a total occlusion were also independent predictors of TLR in men but not in women (Tables 5A and 5B, right panels).
Discussion
Analysis of a current data set of consecutive women and men treated with a PES lends several noteworthy observations. In general, women undergoing PCI remain at a disadvantage when compared to men in terms of baseline clinical characteristics: they are older, with more comorbidities, smaller coronary vessels and a very high prevalence of diabetes. With modern interventional techniques, however, including careful selection of patients and management strategies to lower periprocedural and in-hospital complications, very high immediate success rates and a positive outcome can be achieved in both sexes. At follow-up, our data supports the efficacy of PES also in women. Notwithstanding the adverse predictors at baseline, we actually observed a “paradoxic” more benign long-term clinical outcome in women compared to men,, with a lower absolute need for repeat TLR and no difference in hard clinical endpoints after PES. Several studies have previously reported a similar discrepancy between adverse clinical and anatomic features in women undergoing balloon angioplasty or PCI with bare-metal stents, with a higher periprocedural hazard4,5,11, but a paradoxically very favourable longer term outcome when compared to men7,12-17. In a recent analysis according to gender of the randomised TAXUS-IV trial, Lansky et al9 found that women assigned to the PES did in fact have higher absolute revascularisation rates compared to men. Multivariate analysis, however, showed that the increased incidence of other risk factors for restenosis in women, particularly diabetes and small vessel diameter, were the driving factors, not gender per se9. In our current series, with the use of PES a significantly higher prevalence of diabetes in women (up to almost 40%, as compared with almost 30% in men) did not translate into worse overall clinical outcome long-term. Controversial data exist on the relative impact of diabetes on outcome according to sex. Mehilli et al18, in a large retrospective analysis of 3,349 men and 1,025 women after PCI, found a significantly higher mortality in diabetic women than men at one year (p=0.009), but similar restenosis rates (37 vs. 36%, women vs. men, p=0.9). No significant difference in mortality among the sexes was found in non diabetic patients. In other studies, however, the presence of diabetes was not independently associated with gender-specific differences in outcomes7,19,20.
Peripheral vascular complications
With extremely careful attention to patient management and sheath removal, derived from previous experience7, we were able to decrease the incidence of peripheral vascular complications in women, even though it remained slightly higher than in men (3 vs 2%). Specifically, our current approach is to avoid sending patients to the ward with a sheath in place and instead to remove it immediately after the procedure after reversal of heparin with protamine. We did not observe any complications or stent thrombosis related to protamine administration in this series. Several previous studies have reported a significantly higher peripheral complication rate in women than men21-24.
Angiographic late loss
Although in a limited number of patients, with clinically-driven and incomplete angiographic follow up, the observed in-stent late loss was not higher, as expected in light of adverse baseline predictors, but actually paradoxically slightly lower in absolute terms in women than men. In view of the non-randomised nature and the limitations of the comparison, the significance of this finding is uncertain. In the randomised TAXUS IV study, within a selected population with single de novo lesions, no difference was found in late loss according to gender9.
Limitations
The major limitations of our study stem from the non-randomised nature of the comparisons and as already mentioned in the limited angiographic follow-up. However, we aimed to describe immediate and long-term results in a real-world population on unselected consecutive patients.
Conclusions
Women treated with PES in current practice remain at baseline higher risk than men. However, with careful patient selection and technique, excellent immediate and long-term results can be achieved, not significantly different when compared to men.

