Abstract
Aims: The following manuscript summarizes results from studies regarding flow dynamics and geometrical designs of aortic valves especially focusing on haemodynamics and coronary perfusion.
Methods and results: In an animal set-up optimal orientation of tilting disc and bileaflet mechanical valves with respect to downstream turbulence was defined. Following impact of valve orientation on coronary artery perfusion was investigated again in animals and in a prospective, randomized patient study also including stented and stentless biological valves.
Optimal orientation for tilting disc valves was achieved with the major orifice facing the noncoronary leaflet, whereas the bileaflet valve offered its best haemodynamic performance with one orifice orientated towards the right coronary ostium. No valve substitute reached physiological coronary perfusion. Valve design and orientation had an impact on flow rates. In the patient study biological valves and especially the stentless valve demonstrated the most physiological coronary perfusion.
Conclusion: Haemodynamic performance and coronary perfusion is influenced by valve design and orientation. The haemodynamically best orientations also demonstrated the best coronary flow rates. The most physiological results were achieved for a stentless valve. These findings will have an impact on the design of percutaneous aortic valves.
Introduction
Aortic valve replacement has been considered to be the treatment of choice for aortic stenosis for a long time1. However, the results of aortic valve replacement are not always satisfying right now. Tirone David’s group at the Toronto General Hospital published long term follow up data from different biological valves. He reported a 36 % survival rate at 12 years with the pericardial valve2 and a 47 % survival rate for the Hancock II biological valve at 15 years3. These were not randomized studies, so comparison of the results is limited. However, there is a clear difference in survival between different valve designs in the same patient population. For both valves long term mortality was increased compared to the normal patient population. This observation has been made for mechanical valves as well. The data for the St. Jude Medical valve demonstrated that the survival rates are below the background population4. The 20 years results for the Medtronic Hall tilting disc valve revealed that, at up to 10 years, results are comparable to the background population, but there is a higher mortality after that time period5.
So in summary it has to be admitted that aortic valve replacement leads to increased mortality compared to the normal patient population. These findings could not be explained by what has been defined as valve related complications, because these did not determine outcome, therefore other factors must be taken into consideration. A possible explanation is that current prosthetic valves do not take over all physiological functions of a normal human aortic valve.
To define these physiological functions, functional anatomy of the proximal high pressure system in humans has to be considered. Starting from the left atrium and ending in the descending thoracic aorta, the arterial system forms an almost complete circle with different radii in different segments of the circle. Flow dynamics are different in a straight compared to a bent system. Flow profile in a straight tube demonstrates the highest flow velocities in the centre of the tube, whereas in a bent system the streamline, which represents the line of highest flow velocities, deviates toward the convexity of the bend. This is also true for human anatomy. Nygaard et al. showed that flow separation through a normal aortic valve leads to an eccentric profile with the highest blood flow velocities at the posterior aortic wall6. Even in a stenotic aortic valve with a central orifice eccentric flow was still present of course then with a much higher level of turbulence.
As a consequence of these considerations the proximal high pressure system in humans is a very complex asymmetrical system with respect to anatomy and haemodynamics and this means that orientation of aortic valve prosthesis has to be important for haemodynamics, especially in asymmetrical valves. Secondly, coronary perfusion must be influenced by valve design and orientation. So preservation of the kinetic energy of blood components and optimization of coronary perfusion have to be defined as additional aortic valve functions, which have not been studied in detail yet. An optimal mechanical, biological, and percutaneous valve would recognize these functions and its design should follow flow requirements.
The following studies focused on the impact of mechanical and biological valve design and orientation on haemodynamics and coronary artery flow.
Methods
Animal work haemodynamics7
Two different mechanical aortic valves (Figure 1), the Medtronic Hall tilting disk valve (Medtronic Inc., Minneapolis, MN, USA) and the St. Jude Medical bileaflet valve (St. Jude Medical Inc., St. Paul, MN, USA), were implanted into pigs.
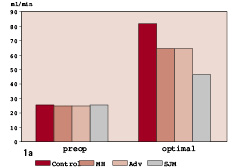
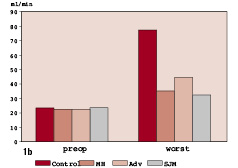
Figure 1a. Comparison of coronary artery flow of the control animals (90 minutes of extracorporeal circulation, 60 minutes aortic cross-clamping, but no valve replacement) to results obtained following aortic valve replacement with the Medtronic Hall (MH), ADVANTAGE (Adv) and St. Jude Medical (SJM) valves in their haemodynamically best orientation. None of the mechanical valves reached the LAD flow of the control animals at normal cardiac output with the highest flow rates for MH and Adv valve substitutes. 1b. In the haemodynamically worst orientation the difference between control and valve animals now is highly significant for all mechanical aortic valves.
The valves were constructed as “Rotation Devices”, which allowed change of valve orientation without reopening of the aorta. Downstream turbulence as key parameter for haemodynamic performance of mechanical valves was measured using a specially constructed perivascular ultrasound device at constant cardiac output of 4 l/min. The tilting disc valve was rotated into a total of 8 different orientations, the symmetrical bileaflet valve into four different orientations.
Animal work coronary perfusion8,9
As a first step impact of extracorporeal circulation, myocardial ischaemia and reperfusion on coronary artery flow was studied. These so called “control animals” (n=4) underwent a 90 minutes period of extracorporeal circulation and 60 minutes of aortic cross-clamping with administration of blood cardioplegia, but no aortic valve replacement.
The obtained results were then compared to animals receiving either a Medtronic Hall tilting disk valve, a Medtronic ADVANTAGE bileaflet valve or a St. Jude Medical bileaflet valve, again mounted on rotation devices.
Prospective, randomized patient study10,11
In 40 patients undergoing aortic valve replacement for severe aortic stenosis and left ventricular hypertrophy coronary flow was measured using Cardiovascular Magnetic Resonance (MRI). Patients scheduled for mechanical valve replacement (n=20) received either a Medtronic Hall or Medtronic ADVANTAGE valve, in the biological group (n=20) either a stented Medtronic Mosaic or stentless Freestyle valve were implanted. Coronary flow was again measured prior to discharge (mean of 5±1 d). At a follow up visit six months postoperatively, transthoracis echocardiography was performed with measurement of transvalvular gradients and left ventricular mass.
Results
Animal work haemodynamics
The mechanical Medtronic Hall tilting disk valve demonstrated a superior, almost physiological flow pattern in the aortic root in its optimal orientation. This was achieved with the major orifice orientated towards the noncoronary cusp. In the other orientations downstream turbulence rose up to values comparable to mild and moderate aortic stenosis. In the St. Jude Medical bileaflet valve the totally physiologic flow separation was not achieved, but the differences between the investigated orientations was not as distinctive. However, still an optimum orientation was found for the bileaflet design, which was defined with one orifice towards the right coronary ostium.
Animal work coronary perfusion
The “control group” demonstrated reactive hyperaemia in the myocardium after the ischaemic period of 60 minutes with LAD perfusion rates increasing from the rest status of 25±4 ml/min to 74±8 ml/min, which probably represents the coronary flow reserve due to maximum vasodilatation. None of the implanted mechanical valves showed such an increase even in the haemodynamically optimum orientation (Figure 1a). In the worst orientation an even more pronounced difference between the control animals and the three mechanical valves was demonstrated (Figure 1b).
Prospective, randomized patient study
Coronary perfusion was inadequate pre-operatively in all 40 patients suffering from aortic stenosis with even partially reversed flow during systole. After aortic valve replacement coronary flow increased in each individual patient and for all valve groups (Figure 2).
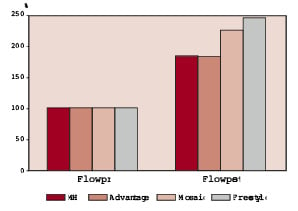
Figure 2. Comparison of pre- to postoperative coronary artery flow rates for mechanical (Medtronic Hall (MH) and ADVANTAGE); stented (Mosaic) and stentless (Freestyle) valves: in the left Preoperative flow rates were set as 100 %, a significant rise was observed for all valves postoperatively. Flow rates were significantly higher for biological valves, especially for the stentless prosthesis (p<0.01).
Furthermore flow profile was now normal with a diastolic perfusion pattern and no longer reversed flow. In the two mechanical patient groups increase in coronary flow was comparable. Both biological valves demonstrated higher rise in flow rates compared to the mechanical groups. A significantly higher increase was shown for the stentless Freestyle prosthesis. This valve design also demonstrated the lowest pressure gradients at discharge and follow up. No differences were observed between the four groups with respect to left ventricular mass regression.
Discussion
Due to the anatomical and physiological asymmetry flow distribution within the aortic root is eccentric with the area of major flow located at the noncoronary cusp. Our studies demonstrated the importance of optimal mechanical valve orientation with respect to haemodynamic performance and coronary perfusion. Biological valves seemed to match the anatomical prerequisites better, as physiological orientation could be achieved and opening and closing characteristics of biological material is closer to the native valve compared to any metallic material.
The experimental study on the impact of valve orientation on coronary perfusion clearly demonstrated the importance also of diastolic performance of valve substitutes. The haemodynamically best valve, Medtronic Freestyle, also provided the highest coronary flow rates. This might be explained by low turbulence levels in the Sinuses of Valsalva, by its flexible sewing ring and the physiological opening and closing characteristics of the zero-pressure fixed leaflets.
The unique chance of designing percutaneous valves is knowledge of the important physiological circumstances that have been published in the last decade. As these valves avoid huge and rigid stent material compared to conventional stented valves, they should already match the important prerequisite of retained flexibility, although with some restriction due to the semi-rigid metal stent itself. This will allow Left Ventricular Outflow Tract (LVOT) motion which Duran demonstrated as physiological and important for valve opening before the pressure in the left ventricle is higher than in the ascending aorta12. However, annulus flexibility will be limited in percutaneous valve implantation as long as the calcified annulus is not resected or dissolved, so some rigidity is added to the otherwise flexible valve design. Another limitation of transvalvular valve implantation is the difficulty to ensure physiological orientation of the trileaflet valve. Special attention should be directed towards the opening and closing mechanism of artificial valves, as pressure gradients and effective orifice area alone do not characterize valve function sufficiently. Other factors like coronary flow reserve have to be taken into consideration to improve especially long term outcome after aortic valve replacement.