Abbreviations
DES = Drug-eluting-stents
MACE = Major adverse coronary events
TVF = Target vessel failure
PCI = Percutaneous coronary intervention
PTCA = Percutaneous transluminal coronary angioplasty
TLR = Target lesions revascularization
BMS = Bare metal stent
TVR = Target vessel revascularization
EuroPCR 2005: the highlights
The EuroPCR 2005 meeting, attracting more than 10.000 attendees, was a highly informative meeting where leading authorities expressed their opinions and pioneering researchers demonstrated new approaches to remaining and vexing problems concerning prevention of in-stent restenosis, percutaneous treatment of complex lesions, structural heart disease and dysfunctioning heart valves, and new approaches to the management (including percutaneous treatment) of stable and unstable coronary artery disease.
Again the EuroPCR 2005 meeting fulfilled its mission which is, clearly voiced by the chairman J. Marco, to improve the Quality of Patient Care.
In this article we reviewed the highlights of this meeting which we selected from a multitude of scientific presentations.
1. Drug-eluting stents: background information
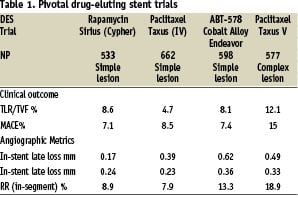
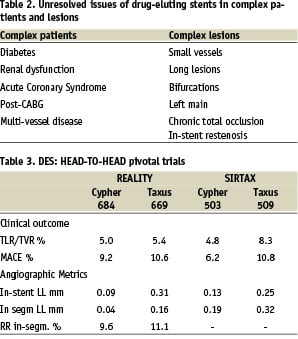
The impressive results achieved with drug-eluting stents concerning reduction of in-stent restenosis have not only been obtained in simple straightforward lesions (Table 1) but preliminary data suggest that these favourable results may also be achieved in acknowledged less favourable lesions and clinical situations (Table 2). And in particular during the Euro PCR 2005 meeting many detailed sub analyses provided further useful clinical information. In addition the two pivotal head-to-head studies comparing the effectiveness of Cypher Stent versus Taxus-Stent have not convincingly shown that there is a clinically significant difference between the 2 drug-eluting stents (Table 3).
1.1 Drug-eluting stents: EuroPCR 2005
Given the fact that DES reduce the in-stent-restenosis rate and MACE (predominantly driven by a reduction in TVF) in simple lesions and that there is no clinical difference between Sirolimus-eluting stent and the Paclitaxel-eluting stent the question is now: do DES also reduce in-stent restenosis and MACE in subgroups of complex patients and lesions? (Table 2). The EuroPCR 2005 meeting provided significant new information in the following sessions: the latest on primary PCI, late breaking trials and update of mulicenter studies and registries.
The latest on primary PCI
Primary PCI of ST-elevation MI has been shown to be efficacious, but delays in onset of symptoms to actual PCI have reduced its efficacy. The PCAT-2, a large meta-analysis of the individual date of 6763 patients obtained from 22 randomised trials of primary PCI versus fibrinolysis provided detailed information about the significance of the delays associated with both approaches with respect to the primary endpoint: 30 day all-cause mortality. The PCAT-2 investigators distinguished between two delays. First: presentation-delay defined as the time between onset of symptoms and time of randomization. Second: PCI related delay defined as the time between start of fibrinolysis and start to primary PCI, because preparations for primary PCI require more time. The 30-day mortality rate was compared between primary PCI and fibrinolysis. The duration of the presentation delay was directly related to the magnitude of the 30-day mortality, both in PCI and fibrinolysis but overall there was a 37% reduction of mortality in favour of primary PCI group (odds ratio 0.63) compared to fibrinolysis. The PCI related delay data demonstrated that longer delays were associated with higher 30-day mortality but nevertheless the 30-day mortality rate in PCI patients was always lower than the 30-day mortality rate in the fibrinolysis patients with an overall reduction of 37% in favour of primary PCI.
These data support the primary PCI approach showing that PCI for acute MI is always superior to fibrinolysis but both presentation and PCI-related delays modulated the superiority of PCI.
Simple thrombo-aspiration devices in acute myocardial infarction
Two small randomized single-center trials assessed the effectiveness of initial thrombus-aspiration in patients undergoing primary PCI for an acute myocardial infarction. The REMEDIA-TRIAL (randomized 50 patients to thrombus aspiration and PCI and 50 conventional PCI) showed better ECG and angiographic myocardial reperfusion rates but no improvement in enzyme release nor early clinical outcome. The EXPORT-TRIAL randomized a total of 50 patients and demonstrated that thrombus-aspiration was associated with better ST-segment resolution and magnetic resonance determined smaller infarct size.
Although thrombus-aspiration is feasible and safe, definitive clinical data are lacking concerning its efficacy.
Late breaking trials
Two interesting studies were presented. The Easy-study investigated whether the PCI radialis approach is safe and cost-effective. The Easy-study was a large-sized randomized non-inferiority trial to compare outpatient PCI (with radialis approach) with a bolus of Reopro (N=504) versus PCI (with radialis approach) and overnight hospitalization and bolus + perfusion of Reopro (N=501) in uncomplicated PCI’s. The primary endpoint defined as MACCE, and bleeds or radialis access complications was achieved in 13.9% of the outpatients and in 11.8% of hospitalized patients, thus showing that outpatient PCI via the radial artery is safe and cost-effective in terms of bed-occupancy.
Recurrence of in-stent restenosis after balloon angioplasty of in-stent restenosis is high with rates reported from 40% to 50%. The Paccocath-ISR-Trial was a randomized double-blind multicenter trial investigating the efficacy of the Paclitaxel coated PTCA catheter (N=27) on the prevention of the recurrence of in-stent-restenosis compared to conventional treatment with a conventional PTCA catheter (N=25). The primary endpoint of the trial was the late lumen loss after 6 months. The late lumen loss was 0.82±86 mm and binary restenosis 40.9% in the control group (conventional PTCA) versus the late lumen loss of 0.13±0.51 mm (P=0.002) and binary restenosis rate of 8.7% (P=0.017) in the PACCO-Cath patients. The MACE rate was 24% (conventional PTCA) vs 3.7% (PACCO-CATH) which was mainly caused by the need of revascularization with a TLR of 24.0% vs 0.0% (P=0.009). Even in this small-sized study the efficacy of the PACCO-cath to prevent recurrence of in-stent restenosis is remarkable.
Update on randomized trials
- The TAXUS-V is one of the pivotal randomized trials demonstrating the efficacy of Paclitaxel eluting stent to prevent in-stent restenosis in patients with long lesions, multiple and overlapping stents and diabetes in 30% of the cases (Table 1). A sub analysis of the TAXUS V using ultrasound provided deeper insights into the neo-intimal process in long lesions and multiple stents. A total of 509 patients underwent intra-stent IVUS at 9 months and the parameters measured were neo-intimal volume and% net volume obstruction of the stent. The neo-intimal volume was 68±52 mm3 in the BMS group versus 30.46±34 mm3 in the Taxus Stent (p<0.0001) a reduction of 56%; the % net volume obstruction was 32±15% in the control versus 13±12% in the TAXUS STENT group (p<0.0001) a reduction of 59%. The IVUS data showed a consistent neo-intimal suppression across the length of stent, across high-risk groups and also in single and double strut regions of overlapping stents.
- The TAXUS-VI is a double-blinded randomized trial comparing TAXUS-MR stent with BMS in patients with: long lesions with use of long or overlapping stents, 56% Type C lesions and 20% diabetics. Two hundred seventeen patients were randomized to BMS and 216 to TAXUS-MR stent implantation. At 2 years TVR in the TAXUS-MR was significantly reduced to 13.9% vs control stent 21.9% (P=0.034), however the MACE rate at 2 years was not different between the groups: 21.3% vs 25.1%; P=0.37). The benefit on the TLR rate was preserved in high-risk subsets such as those with small (<2.5mm) vessels, long (26mm) lesions and overlapping stents.
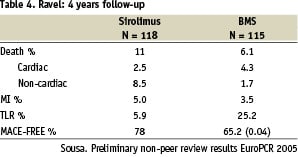
- The RAVEL-study was the first randomized study on a drug-eluting stent, the Cypher stent; the patients were recruited between 1999 and 2001. The TLR at 1 year was 0% in the Cypher stent group. At 4 years there still was a significant difference in the Cypher TLR rate 5.9% compared to control BMS 25.2% (Table 4). It may be concluded that the beneficial results of the Cypher stent are durable, and it is of note that there was no-late in-stent thrombosis. Remarkable and unexplained was the relatively high non-cardiac death rate in the Cypher-patients
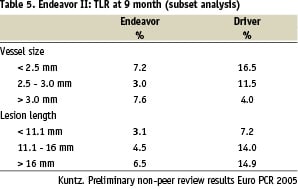
- The Endeavor II was a pivotal randomized study comparing the ABT-578 Cobalt-Alloy Stent (N=598) versus the Driver-stent (N=699) (Table 1). In a subset analysis of vessel size, lesion length and diabetics it appeared that the efficacy of this drug-eluting stent was also maintained in these various subsets (Table 5).
- The STEALTH-Trial was a randomized trial (2:1 DES: BMS) investigating the safety and efficacy of a new rapamycin derivative, Biolimus A-9 eluted from a bio absorbable PLA-coated stent (Biomatrix) in the novo coronary lesions. The STEALTH-Trial was a first in man study (N=120) and the primary endpoint was the Late Loss at 6 months. However the Late Loss data was not available The MACE rate at 12 months was 12% in DES and 6.3% in BIOMATRIX patients. Time will tell whether this stent-design will have similar or improved results compared to conventional drug-eluting stents.
- The RIBS-II Trial was a multicenter, prospective randomized study comparing the efficacy of Sirolimus-eluting stents (SES) (N=76) versus balloon angioplasty (BA) (N=74) for the treatment of in-stent restenosis. The primary endpoint was recurrent in-stent-restenosis which occurred in SES in 11% and in balloon angioplasty in 39% (P<0.001). The Late Loss was 0.28±0.6 (SES) vs 0.77±0.7 mm (BA) respectively and freedom of death, MI and TVR was 88% (SES) versus 69% (BA). Thus SES implantation is highly effective in the treatment of patients with in-stent-restenosis.
- The DEFER-study was a multicenter randomized study to compare deferral (N=91) versus performance (N=90) of PCI of non-ischemia producing stenoses in patients with stable angina pectoris. These patients were followed for 5 years. The combined death/mi rate occurred in 3.3% in the deferral patients and in 7.9% of the performance patients. The total number of adverse events occurred in 23% (deferral patients) versus 32% (performance patients). The prognosis of a non-stented non-ischemia producing stenosis (FFR≥0.75) is excellent and the risk of progression to death or myocardial infarction is <1% per year. Thus stenting a non-significant lesion does not result in clinical benefit in patients with stable pagina.
Important studies and registries
The Da Vinci Registry was a “real world” postmarketing study demonstrating the efficacy of the Multi-Link Vision Stent. The Stent is made of cobalt-chrome, has very thin struts (0.08mm) is highly radiopaque and has a low allergic potential. Between July 2003 and June 2004 1344 patients were recruited from 32 German Centers and these patients were followed for 9 months (N 1264: 98.0% complete follow-up). The baseline characteristics of these patients were: 88% B, C lesions, 60% multivessel disease and 25% diabetics. At 9 months the rates of death 0.8%, myocardial infarction 1.5%, revascularization 10.2% and MACE 12.4% demonstrated that this new design bare-metal stent is safe and effective in the treatment of “real world” patients. The EUROSTAR Trial was a registry of 145 patients who received a Co-star Cobalt Chromium Paclitaxel-Eluting Stent with controlled targeted drug delivery. The primary endpoint was the 6 month in-stent late loss, which was 0.26±0.39 mm; the in-stent restenosis rate was 3.4% and stent thrombosis 0.7%. The Costar Cobalt Chromium Stent system is highly deliverable, radiopaque and is associated with excellent angiographic 6 month-results.
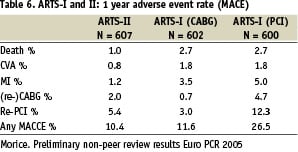
The ARTS-II Study was a single arm multicenter registry to demonstrate non-inferiority in clinical and cost-effectiveness with the Cypher-stent compared to previous results of the ARTS-I trial (CABG versus bare metal stent) for the treatment of multivessel disease of de novo coronary lesions. The relevant data of the ARTS-I and II studies are presented in Table 6. Despite the higher risk profile of the patients in the ARTS-II compared to ARTS-I patients the MACCE rate at 1 year is lower in ARTS-II (DES) than ARTS-I (PCI) and almost similar to ARTS-I CABG. Therefore in selected patients with multi-vessel disease CABG may not be the preferred option.
The PORTO-Trial was a registry investigating the safety and efficacy of the Cypher-stent in the novo native lesions in small vessels (<2.5 mm) in diabetics (n=121) and non-diabetic (N=141) patients. The primary endpoint was the in-stent-late loss at 6 months which was 0.10±0.38 mm in diabetics and 0.05±0.38 mm in non-diabetics. The restenosis and MACE rates were 6.6% vs 4.3% and 5.0% vs 1.3% respectively for diabetic and non-diabetic patients. The data suggest that the Cypher-stent is safe and efficacious in patients with small vessels and opposite to other studies there appears to be no difference in outcome in diabetics and non-diabetics.
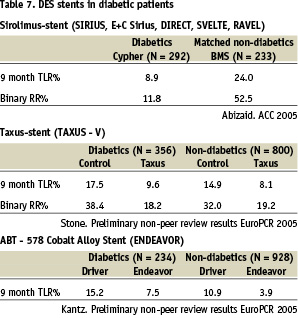
1.2 Drug-eluting stent in diabetics
Diabetic patients are notorious for the high adverse event rate after balloon angioplasty or bare metal stent implantation caused by the high frequency of in-stent restenosis and progression of disease in the non-stented coronary segments. However, preliminary data indicated that DES-implantation appeared to reduce the in-stent restenosis. Data, presented at the EuroPCR 2005 extended these findings. Subanalysis from the TAXUS V and ENDEAVOR Trials demonstrated a significant reduction in the TLR rates and binary restenosis rates (Table 7). The DAVINCI-Trial data showed that the TVF and MACE-rate in diabetic patients was 13.8% and 15.6% respectively. It may be concluded that drug-eluting stents appear to reduce the in-stent restenosis rate in patients with diabetes either those on oral diabetic treatment or requiring insulin treatment. Optimal therapy for diabetic patients should be directed toward metabolic normalization in addition to local-stent based therapy.
1.3 Bifurcation lesions
Several stent techniques, are currently available and used for the treatment of bifurcation lesions. Basically, they can be divided in two strategies: simple vs. complex, where simple is stenting of the main branch and only balloon angioplasty of the side branch while complex means stenting of both branches.
During the bare metal stent era, six month total MACE were in the range of 40% for the simple strategy and as high as 50% for the complex one. With drug eluting stents, the results in terms of restenosis and TLR rate have improved. However, in the current DES era, the results using the simple approach are at least similar or even better than using the complex technique. Preliminary data suggested that using the complex approach SES may be more efficacious that DES in reducing in-stent restenosis, however the MACE rate was not different between the two drug-eluting-stents.
To prevent restenosis, final kissing balloon is recommended following the crush technique. Whether the “final kiss” should be mandatory also in cases where the simple technique or a non-crush complex approach is carried out remains unclear.
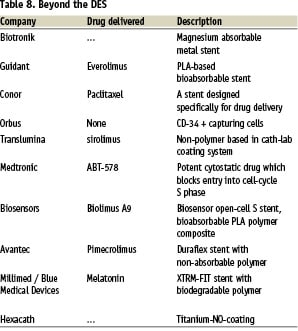
1.4 Future stent designs
The development of safer, and more efficacious stents, which are easier to deliver continues. Stents with new platforms and novel therapeutic principles such as the “Limus” family, paclitaxel, NO, melatonin, and VEGF or agents that enhance endothelial healing are new being tested and the first, very preliminary results were presented during the meeting (Table 8).
2. New small type and in hold ie new challenges in percutaneous non-coronary cardiac intervention
New treatments for percutaneous non-coronary cardiac intervention include patent foramen ovale and hypertrophic obstructive cardiomyopathy.
2.1 Current status of patent foramen ovale
Patent foramen ovale (PFO) is a common disorder, with an estimated prevalence of 19-36% in healthy individuals, which increases to 40-60% among young (<55 years old) patients presenting with cryptogenic stroke, and up to 70% in subjects affected by obstructive sleep apnea. Several closure devices have been reported, with different success (>80%) and complication rates 2-3% including thrombosis, device migration, perfusion, tamponade and fistulae formation.
The indications to perform a catheter-based PFO closure are currently debated and long-term follow-up studies still on going. Young patients with cryptogenic strokes are potential candidates for such a treatment, especially in cases of high-risk features such as long tunnel PFO, PFO causing haemodynamic consequences and/or PFO associated with atrial septal aneurysm (ASA). The role of echocardiography is crucial for monitoring the procedure and -there is an emerging role of intracardiac echocardiography in this setting.
A second potential indication to treatment, which is also investigated by ongoing randomized clinical trials, is migraine. Unfortunately the great majority of these studies for instance MIST-Trial will not be completed before 2008.
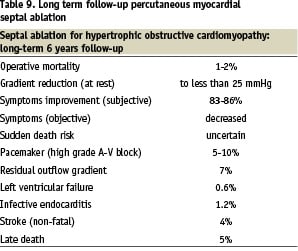
2.2 Current status of septal ablation for hypertrophic obstructive cardiomyopathy
Percutaneous myocardial septal ablation (PTSMA) is an alternative treatment to surgery (myectomy) in hypertrophic obstructive cardiomyopathy.
The indications to perform this catheter-based intervention are the same as for surgery, with the ideal candidate affected by the classical subaortic septal hypertrophy, septum thickness in the range 18-30 mm, SAM-dependent LV outflow tract opening (LVOTO) and mitral regurgitation (MR). The patients presenting with severe MR with central-anterior jet are usually excluded. The technique consists of contrast echo guided slow ethanol injection in fractions of 0.5/1 ml in the septal target vessel, through an over the wire positioned inflated balloon. The major complications include risk of transient total AV block in 50-60% of the cases with permanent pacemaker dependency in 5-10% of the patients. The short-term outcome has shown good result, with a LVOT gradient reduction in 90% of the treated patients and an improvement in exercise capacity. The results seem to be maintained during the long-term 6 years follow up. The data in Table 9 represents best estimates based on available published data. However, it should be noted that longer follow-ups are clearly needed before this less invasive percutaneous approach may become an established alternative to surgery.
There is a special concern that the PTSMA - induced damage together with spontaneous degeneration of the AV conduction system may lead to pacemaker dependency over time. Moreover, whether PTSMA is able to favourably affect the natural history of the disease is currently unknown.
2.3 Percutaneous aortic valve replacement
Traditional percutaneous treatment of acquired valvular heart diseases is mostly made up of percutaneous mitral commissurotomy and percutaneous aortic valvuloplasty. However, the field of catether-based interventions for valve disease is a new and growing area of research and future clinical challenges. Alain Cribier performed the first aortic valve replacement in 2002 using a valve composed of equine pericardial leaflets mounted on a balloon expandable stent. He used a transseptal antegrade approach, while a retrograde technique was also later developed and successfully employed in humans. Since then, 41 patients have been overall recruited on a compassionate basis. The mean age is 80 years old, with 35 patients affected by NYHA class IV heart failure and 6 presenting with cardiogenic shock. Twenty-nine patients underwent successful valve implantation, with one patient dying immediately afterwards due to haemodynamic compromise, one episode of stroke and two cases of pericardial tamponade due to pacemaker lead in one and as complication of the trans septal approach in the other. One technical issue is the need to perform balloon predilatation before valve placement. This is usually carried out during rapid (>200 beats/min) pacing to simulate cardiac arrest. This might be performed 2-5 days before the procedure, in order to properly size the aortic anulus for subsequent valve positioning and to obtain a transient haemodynamic improvement before the actual treatment. The paravalvular leak and acute dislocation of the valve prosthesis are currently being addressed to improve short- and long-term durability of the treatment.
2.4 Percutaneous mitral valve repair
For mitral valve insufficiency two main techniques can be used: the edge-to-edge technique and prosthetic ring annuloplasty. The edge-to-edge technique mimics the Alfieri surgical procedure, which consists of creating a double mitral orifice by means of a few stitches securing the two leaflets together in their midpart and thus creating ‘a tissue bridge’. In the EVEREST trial, 27 patients with severe mitral regurgitation have been treated with percutaneous edge-to-edge technique. Successfully implantation has been obtained in 24 (89%) patients, with a 67% event free survival at a median of 6 months. Prosthetic ring annuloplasty is at an even earlier stage of evaluation than the edge-to-edge technique. The only data available at the moment are experimental.
3. Imaging
3.1 Prime time for MSCT?
The diagnostic accuracy of 16-slice MSCT to detect a significant coronary lesion (> 50% luminal diameter) was evaluated in (pooled-data) 605 patients for vessels greater than 1.5 to 2 mm in diameter. Overall the sensitivity was 86% and the specificity was 96%; however, about 10% of the coronary segments were of non-diagnostic image quality and were excluded from the analysis. The preliminary results from the newest generation 64-slice MSCT scanner have shown improved image quality, due to the increased temporal and spatial resolution with sensitivity and specificity of more than 90% and now including all coronary segments for analysis. Significant remaining problems with CT scanning are severe calcification, absence of stable sinus rhythm, and the rather high radiation exposure.
Currently MSCT cannot be regarded as a viable alternative to invasive diagnostic coronary angiography. However, future developments in this avant-garde technology are expected to overcome many of its current shortcomings.
3.2 MRT whole-body vascular imaging
Atherosclerosis in one territory often means atherosclerosis in other areas. Peripheral artery disease (PAD) patients suffer up to 30% and 60% of cases of stroke and myocardial infarction respectively. In addition, more than 70% of three vessels disease patients are affected by PAD. The “angio-body surf” is a new system for whole-body 3D MR angiogram which can be performed in 72 seconds. MRT sensitivity to detect vessel stenosis and occlusions is estimated about 94%. Erbel et al. applied this new technology in a population of 163 participants with know coronary artery disease able to detect concomitant peripheral vascular disease. Only 25% of the patients had no abnormal MRI findings. Of those 75% with atherosclerotic stenoses in other territories, 45% had a significant artery stenosis, occurring in 12.5% in carotid, 17.5% in renal and 34.5% in peripheral arteries. Several “incidental findings” were also reported, such as 20 patients with cerebral atrophy, 13 patients with pulmonary nodules, 1 patient with renal cell carcinoma.
These preliminary findings have shown the potential preventive diagnostic capacity of whole-body 3D angio MR.

