Abstract
Aims: To compare reperfusion times and in-hospital outcome of patients with STEMI treated with primary percutaneous coronary intervention (PCI) in a teaching hospital (TH) with or without inter-hospital transfer and in community hospitals.
Methods and results: We performed a retrospective analysis of 536 patients with STEMI treated between January 2005 and December 2006 with primary PCI. Three groups were identified. A: 207 patients presented to the TH. B: 121 patients transferred to TH from metropolitan area hospitals (MAH). C: 208 patients presented in two rural area hospitals (RAH) with primary PCI capability.
Baseline characteristics were similar. Door-to-balloon (DtB) times were significantly (p<0.001) higher in group B (median 120, range 90-180 min) both compared to group A (median 60, range 45-90 min) and C (median 73, range 55-99 min). In group B 79,5% of patients present a DtB > 90 min. In-hospital mortality was 4.9%, 3.3% and 4.3% respectively in group A, B and C without significant differences.
Conclusions: The expansion of primary PCI to RAH achieves reperfusion delays similar to that of patients admitted to TH. Transferred patients present very higher DtB when compared to patients treated on-site. In-hospital outcome are similar but further studies are warranted.
Introduction
Primary percutaneous coronary intervention (PCI) has been largely accepted as the more effective reperfusion therapy in ST elevation myocardial infarction (STEMI). Compared to systemic thrombolysis, primary PCI leads to a reduction in mortality, reinfarction, intracranial bleeding, re-occlusion of the infarct related artery and recurrent ischaemia.1,2 Reduction in mortality is more evident in patients with haemodynamic instability and cardiogenic shock.3 These advantages are maintained when primary PCI is performed by experienced operators in high volume centres with a maximum door-to-balloon (DtB) time of 90 minutes.4,5 Observational studies, however, have showed that only a minority of STEMI patients are treated with primary PCI6,7 and that the main determinant of the reperfusion strategy is primary PCI capability at the site of first presentation.8
A high percentage of patients admitted in a hospital without PCI facilities did not receive any reperfusion therapy8. Recent randomised controlled trials9-11 and one metanalysis12 have demonstrated that early and rapid transfer for primary PCI from non-PCI-capable hospitals to a tertiary (PCI-capable) centre is still superior compared to local fibrinolysis. Alternatively, when the expected delay is clearly >90-120 min a pharmaco-invasive strategy of reduced dose thrombolysis followed by transfer for angioplasty is preferable to continuous local medical treatment13-16. The applicability of primary angioplasty is limited mostly to metropolitan areas and is extremely challenging in rural areas due to the distance from tertiary centres. Rapid transfers are not always available and moreover not all STEMI patients are stable enough to be transferred.17
In 2005, the Italian Scientific Cardiology Societies and Associations elaborated a consensus document18 to implement the creation of networks extending PCI treatment also to patients presenting at community hospitals. We present novel data on an integrated network developed in Florence with an innovative approach integrating transfer for primary PCI for patients admitted in metropolitan area hospitals (MAH) as well as supervised on-site training of local cardiologists to expand primary PCI capability in rural area hospitals (RAH). The aim of this retrospective study was to analyse the initial results of this network in terms of treatment delays and in-hospital outcomes.
Methods
Setting
The province of Florence can be divided into metropolitan and rural areas depending on geographical features and distance from the teaching hospital (TH). Median transfer time by car to TH are 25 minutes from MAH and 51 minutes from RAH. Since 200019,20 the STEMI network in our region is based on a “hub-and-spoke” model in the metropolitan area and on developing a primary PCI program in two peripheral hospitals without on-site cardiac surgery located in a remote rural area.
The metropolitan area covers an area of 2,779 Km2 with 801,060 inhabitants. There are six hospitals: one tertiary centre and TH two hospitals with intensive coronary care units (ICCU) without PCI capability and two hospitals with only emergency departments (ED). The TH is an high volume centre with catheterisation laboratories (CL) working 24 hours per day, seven days per week performing a mean of 3,000 PCIs/year.21,22
The rural area extends for 933 Km2 with 228,961 inhabitants. In this area, there are four hospitals: two hospitals with ICCU and PCI capability and two hospitals with only ED (Figure 1).
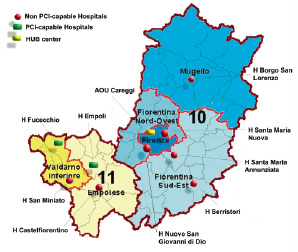
Figure 1. Map of Florence area with the spoke centres without PCI capability in red, the spoke centres with PCI capability in green and the Hub centre (teaching hospital) in yellow.
The metropolitan area has been organised according to an hub-and-spoke model, where TH is the hub centre and other MAH are the spoke centres (Figure 2).
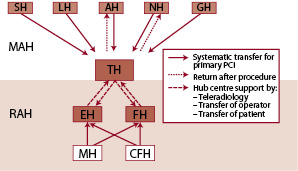
Figure 2. STEMI network organisation in Florence area. All MAH systematically transfer patients for primary PCI to TH. RAH perform on-site primary PCI and maintain support from TH by tele-radiology consultancy, transfer of expert operator or transfer of patient. SH: Serristori Hospital, LH: Borgo San Lorenzo Hospital, AH: Santa Maria Annunziata Hospital, NH: Santa Maria Nuova Hospital, GH: Nuovo San Giovanni di Dio Hospital, EH: Empoli Hospital, FH: Fucecchio Hospital, MH: San Miniato Hospital, CFH: Castel Fiorentino Hospital.
Patients with STEMI, initially presenting in MAH are transferred for primary PCI to TH. After percutaneous revascularisation, patients are early transferred back or admitted in TH ICCU according to the MAH capability and the patient’s risk profile.
The RAH are far from TH; the transferring time is longer due to greater distances and traffic congestion. In order to avoid unacceptable delays, since 2000, a training PCI program has been established between TH and the two RAH with PCI capability. During these years interventional cardiologists of the RAH have been trained in performing primary PCI by the experienced high-volume interventionalists of TH. The rural area interventional cardiologists routinely performed elective angioplasty either at the TH or at the RAH. In addition, when a STEMI patient arrives to a RAH the on call TH interventional cardiologist systematically moves them to the RAH using an emergency car to perform PCI with the rural area cardiologist. By 2005, at the end of the training program (Figure 3), the staff of the RAH had acquired the capability of performing primary PCI.
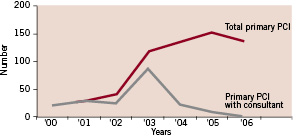
Figure 3. Accreditation of peripheral operators from 2000 to 2006 with progressive decrease of the need for consultants for primary PCI.
From 2005, STEMI patients presenting in one of the RAH are treated at the arrival hospital by rural area staff. The rural area cath labs have 24 hour primary PCI capability and perform a total of 515 PTCA/year (including elective cases).21,22
RAH have been also linked with the TH by a tele-radiology system (RADIN, Mercury Computer Systems Inc. Chelmsford, MA, USA) for consulting about procedural issues or in order to evaluate opportunities to transfer the patient to TH or of the interventional cardiologist to the RAH (Figure 2).
Patients selection
From January 2005 to December 2006, 536 consecutive patients presenting with STEMI at the ED, treated with primary PCI and admitted in our TH referral ICCU and in ICCUs of the RAH, were retrospectively evaluated.
Three groups of patients were identified:
– Group A: 207 patients presented at TH and treated directly with primary PCI.
– Group B: 121 patients presented at MAH and transferred for primary PCI in to TH.
– Group C: 208 patients presented at RAH with PCI facilities and treated in the on-site CL.
Diagnosis of STEMI was made, according to standard criteria.
Procedure
Primary PCI was performed in all patients. Patients were treated with standard antiplatelet therapy. Administration of platelet glycoprotein IIb/IIIa inhibitors was left to the operator’s discretion. Percutaneous coronary stenting, use of additional devices (e.g., thrombectomy catheters) and other treatment options (e.g., intra-aortic balloon pump) were at the physician’s discretion.
Clinical endpoints
The intervals considered were the time-to-hospital (TtH), the door-to-balloon (DtB) and the time-to-treatment (TtT). TtH was defined as the interval between symptom onset and arrival in the ED. DtB was defined as the time interval from arrival in ED to first inflation of balloon in the infarct related artery. TtT was the sum of TtH and DtB. The primary endpoint of the study was DtB.
As secondary endpoints we adjudicated the occurrence of in-hospital adverse events, i.e., death, emergency CABG for PCI failure, non-fatal recurrent myocardial infarction, major bleeding and vascular complications. Non-fatal re-infarction was defined as new clinical symptoms or electrocardiographic changes associated with an increase in the creatine kinase level more than twice the upper normal limit with an increased creatine kinase-MB. In cases in which the creatine kinase level had not returned to normal values after the index event, a second peak was defined as repeat MI. Vascular complications were defined as the occurrence of haematoma with a main diameter >5 cm, pseudoaneurysm, arteriovenous fistula or the need for vascular surgery. Major bleeding was defined as haemorrhages that required transfusions or cause a fall in haemoglobin levels of at least 5 g/dL.
Statistical analysis
SPSS 12 (SPSS Inc., Chicago, Illinois, USA) was used for computations. Continuous data were expressed as mean±standard deviation and were compared using the Student t-test. Categorical variables were expressed as a percentage (%) and were compared using chi-squared test. For all tests, a two-tailed p <0.05 was considered significant.
Results
Characteristics of the study population
General characteristics of patients are listed in Table 1.
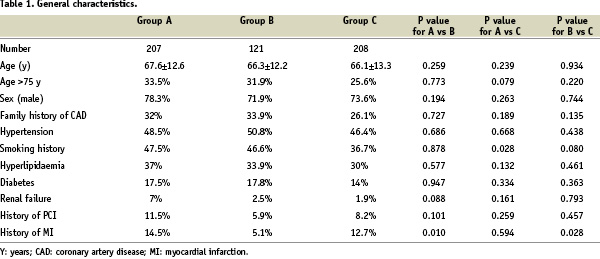
As regards clinical and angiographic characteristics (Table 2), mean ejection fraction (EF) of patients in group C was significantly higher (p<0.001) both in respect to group A and B. Moreover, group C had a lower rate of patients with three-vessel disease (p=0.034 when compared with group B).
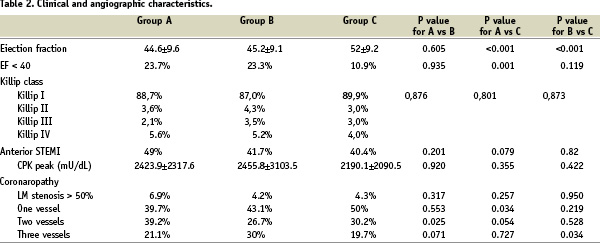
There were no significant differences between groups concerning infarct location, infarct size (represented by CPK peak) and Killip class at presentation.
Procedural characteristics are listed in Table 3.
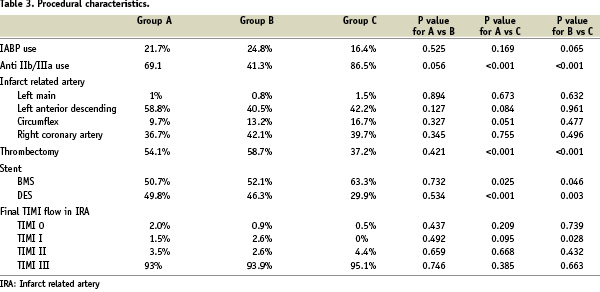
Thrombectomy use and drug eluting stent (DES) implantation were significantly (p<0.001) lower in group C compared to the other two. Procedural success was high with more than 90% of patients achieving a final TIMI III flow in the three groups. Administration of IIb/IIIaGP inhibitors (abciximab, tirofiban or eptifibatide) in group C was significantly (p<0.0001) higher respect to both group A and B.
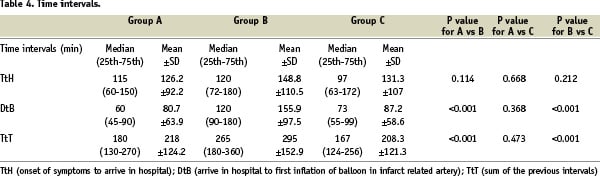
Treatment delays
TtH times were similar without significant differences between patients living in metropolitan and rural areas. DtB times were significantly (p<0.001) lower in patients with direct access to hospitals with CL (group A: median 60 min, mean 80.7±63.9 min; group C: median 73 min, mean 87.2±58.6) compared to patients requiring an inter-hospital transfer for primary PCI (group B: median 120 min, mean 155.9±97.5 min). TtT times were likewise significantly (p<0.001) higher in group B in respect to the other two groups with no significant differences between groups A and C (Table 4).
In group B, only 20% of patients were revascularised with a DtB < 90 minutes while these rates for group A and C were higher (respectively 67.8% and 66.7%). Most of the patients in group B (64.8%) presented a DtB > 120 minutes (Figure 4).
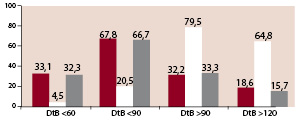
Figure 4. Percentage of patients with DtB < 60, < 90, > 90 and > 120 minutes in the three groups. All p values < 0,001 for A vs B and C vs B. No significant differences between groups A and C.
In-hospital outcome
In-hospital adverse events are listed in Table 5.

No patient required an emergency aortocoronary bypass surgery (CABG) for PCI failure or complication. Only one patient in group C had an in-hospital
non fatal reinfarction due to subacute stent thrombosis treated by re-PCI.
Mortality, both considering patients with or without cardiogenic shock, was not different in the three groups. There were no significant differences in terms of major bleeding and vascular complications.
Discussion
Quality improvement efforts concerning the treatment of patients with STEMI undergoing primary PCI have focused on strategies to improve the timeliness of reperfusion therapy in patients who present to hospitals without PCI capability. In our province two strategies to optimise reperfusion time for rural area patients were available: improvement of transferring systems or the development of a PCI program in a RAH. Due to poor viability of conditions for a emergency medical system (EMS) program, the second strategy was applied.
Our observational study, reporting the results of our integrated network, has two main findings: firstly, expanding primary PCI capability to a medium-volume CL is safe and can assure revascularisation with short DtB times also in patients living in rural area; secondly, the hub-and-spoke model with inter-hospital transfer even in a metropolitan setting results in very high treatment delays. The expanded primary PCI capability model, supported by TH operators, avoids the secondary transfer of patients and permits to achieve operators technical competence in community hospitals.
The first important reason for developing this model was to improve access to primary PCI for patients with STEMI. Recent reports8,19 showed that the strongest independent positive predictor of the reperfusion therapy in STEMI patients was PCI capability at first-admission hospital. Twenty-eight to thirty-five percent of STEMI patients admitted to a hospital without PCI facilities were treated with a conservative approach while this occurred in only 9.7% of patient admitted to a PCI-capable hospital. Thus, the transfer for primary PCI may carry a different revascularisation rate for patients living in rural area especially in high risk patients with clinical instability that could limit transfer possibilities.
The second reason is that interhospital transfer for the treatment of STEMI patients in hospital located in remote rural area often means long reperfusion delays. The median interval from randomisation in the community hospital to primary PCI in the tertiary centre was 94 minutes in the PRAGUE-210 trial and 108 minutes in the DANAMI-29 trial. Data from recent reports show that, in the real world, transfer time is unfortunately even longer than in randomised trials. In the United States the patients with STEMI treated with a DtB time < 90 minutes are only 40%23, and only 4.2% (with a median DtB time of 180 min) between those transferred for primary PCI from a community hospital.24 In a Canadian report median DtB time in patients with interhospital transfer was 142 minutes with only 8% of the patients receiving primary PCI with a DtB < 90 minutes.25,26 The Mayo Clinic STEMI protocol permitted to achieve median door-to-balloon times of ≈2 hours for patients who required transfer to a PCI center.27 Our data showed that the majority (64.8%) of patients requiring an interhospital transfer had DtB times > 120 min although driving times from MAH to TH should not take more than 30 minutes. The reason of delay is not only due to the transfer itself but to the time required for an available ambulance. Therefore, the centralisation of STEMI patients from spoke to hub center according to our data need an improvement with a dedicated STEMI network, especially regarding EMS organisation. We are developing a model promoting on-site diagnosis and direct transfer from the patient’s home to the CL.
Several observational studies28-37 and one randomised controlled trial23 demonstrated the safety and effectiveness of PTCA with off-site surgery backup. In our model, in case of high risk patients or very complex lesions, there is still the possibility to obtain the TH operators support. During the study period only 4 (1,9%) patients were transferred from RAH to TH after initial reperfusion.
Despite that DtB time has been shown to be correlated with mortality,17,38 in our study we did not find any significant differences in clinical outcome among the 3 groups although DtB time was significantly longer in metropolitan area patients. Albeit not statistical significant a trend towards a higher mortality in group A was observed, probably due to the higher incidence of cardiogenic shock. However the limited number of patients and the heterogeneity of risk profiles do not allow us to draw any definite conclusion.
A very important issue is whether mortality was reduced at the RAH by introducing on-site primary PCI. Since 1995 to 2006 the introduction of primary PCI at the RAH led to a significant rise of reperfusion rate and to a reduction of in-hospital mortality (Table 6).
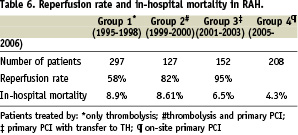
These data are only descriptive because risk profile was not known in all patients and it was not possible to perform a case-control analysis.
In conclusion primary PCI facilities in RAH with a dedicated proctoring program is safe and permits a timely fashion reperfusion even in rural area patients. At the same time the strategy of a systematic transfer from MAH to TH resulted in very higher DtB times when compared to the delays at a PCI-capable hospital as first admission site. In-hospital outcome was similar even if our data need to be confirmed by larger cohort.
Limitations
This retrospective outcome research study suffers from the limitations inherent in this type of clinical research. Small sample size (risk of a type 2 error) and differences in baseline risk profile might have affected outcome data. However, data abstraction and event adjudication were carefully performed to minimise information bias. In addition, the proposed model hereby described cannot be envisaged in all settings and resources needed to implement it were not measured so that no cost-benefit analysis may be performed.

