Abstract
Aims: Cardiovascular magnetic resonance imaging (CMR) perfusion studies performed early after successful angioplasty in AMI nearly always shows incomplete tissue reperfusion despite normal coronary blood flow by TIMI score. In contrast, when performed a few weeks or months after AMI, CMR first-pass perfusion (FP) is usually normal. This study was conducted to determine the kinetics of tissue reperfusion after reperfused AMI in humans.
Methods and results: We prospectively analyzed patients who presented with ST-segment elevation myocardial infarction between July 2002 and January 2005. Included patients had TIMI 3 flow after acute PCI and CMR FP imaging within four months post-MI. CMR FP was performed after injection of 20 cc of gadolinium chelate and imaging was performed with a Siemens Symphony 1.5 T. For FP analysis, each slice was divided into 8 segments which were subdivided into subepicardial and subendocardial layers. Normal perfusion was defined as less than 5% of segments involved by hypoperfusion. Patients were divided into groups according to the delay between MI/reperfusion and CMR. The reperfusion curve was established by plotting the percentage of patients with normal perfusion in each subgroup.
A total of 184 CMR were analysed out of 146 patients included in the study. Probability of normal perfusion was 24%, 31%, 35%, 33% and 43% at respectively day 1, day 2, day 4, day 6 and day 8. This probability increased to 67% at week 2, and at week 3 reached a 100% probability (Spearman’s rho -0.471, p = 0.001).
Conclusions: Despite complete restoration of epicardial flow, early myocardial reperfusion as assessed by CMR is very uncommon. Myocardial perfusion is progressively restored and capillary blood volume recovered normal values between weeks 2 and 4 after MI.
Introduction
Achievement of normal coronary epicardial vessel perfusion, as assessed by TIMI3 flow after percutaneous coronary angioplasty, has so far been considered as the main objective of the treatment of acute myocardial infarction1. Although immediate and prolonged restoration of normal coronary blood flow in the infarct artery is always required , the restoration of TIMI 3 flow does not always ensure myocardial tissue reperfusion which is associated with improved clinical outcomes2-5.
The phenomenon of microvascular obstruction occurs frequently in the first few days after acute myocardial infarction6. The pathological basis of this phenomenon was investigated by experimental studies which showed that micro vascular obstruction may result from endothelial swelling, myocyte oedema, and of capillary obstruction by neutrophils, erythrocytes, plaque debris and thrombus7. Echocardiographic and cardiac magnetic resonance (CMR) data demonstrated that microvascular obstruction was associated with higher myocardial damage8,9 and subsequent clinical studies pointed out the deleterious role of microvascular obstruction on left ventricular remodelling and increased mortality4,5.
Cardiovascular magnetic resonance imaging (CMR) gadolinium first-pass perfusion allows an accurate determination of microvascular obstruction10,11. When performed early after reperfused AMI, CMR near always shows incomplete tissue reperfusion12,13. In contrast, when performed a few weeks or months after acute myocardial infarction onset, CMR gadolinium first-pass perfusion is usually normal confirming the data obtained from animal studies that have demonstrated that micro vascular obstruction is a reversible phenomenon14.
This study was conducted to determine the kinetics of tissue reperfusion after reperfusion in AMI in humans.
Methods
Patient population
From July 2002 to November 2004, patients were prospectively referred for CMR after successful primary coronary intervention (final TIMI 3 flow and residual lesion <50% within 12 hours of chest pain onset).
CMR
CMR was performed on a Siemens Symphony 1.5 Tesla scanner (Siemens Medical Systems, Erlangen, Germany) with a six-element cardiac phased array body radiofrequency coil to realize both cine and perfusion images. The cine images were obtained with ECG gating and during repeated breath holds averaging 10 seconds. CMR procedures were standardised to obtain in each patient after a scouting sequence, the two-chamber, three-chamber and four-chamber long axis views with cine images. The left ventricle was then scanned with 5 to 8 contiguous slices in short axis views (thickness of 8 mm), covering the left ventricle from base to apex, using retrogated True Fast Imaging with Steady Precession (TrueFISP) sequences designed for regional contractility study and wall thickening analysis. Usual scan parameters included a temporal resolution of 34 ms, a TR of 3.0 ms, a TE of 1.5 ms, and typical voxel size 1.4 * 1.8 * 8 mm3. Functional assessment of the myocardium was performed before the injection of gadolinium.
The first pass perfusion was performed using a TrueFISP six short axis slice sequence. Acquisition was made immediately after injection of a 20 cc (average dose of 0.125 mmol/kg) bolus of gadolinium diethyltriaminepentaacetic acid (Gd-DTPA). The six slices were acquired every other heart beat in the minute following the injection of gadolinium. The perfusion images were performed with a field of view averaging 300 to 350 mm, an image matrix of 160 * 128 and a slice thickness of 6 mm.
Gadolinium delayed enhancement assessment was performed between ten to fifteen minutes after gadolinium bolus. After adjusting the inversion time to ensure a maximal contrast between heart muscle and gadolinium, the acquisitions were performed using TrueFISP sequences in the short axis and slices were correlated with those of the short axis cine CMR. Precise parameters were TE 4.4 ms, TR 9.8 ms, inversion time comprised between 240 and 320 ms and typical voxel size 1.3 * 1.6 * 5 mm3.
Study parameters
The following parameters were measured : diastolic and systolic volumes, ejection fraction, myocardial mass and wall motion using the MASS 5.0 software (Medis, Leiden, The Netherlands).
First pass perfusion analysis
First-pass perfusion sequence analysis was performed according to a sixteen segment per slice model. Each short axis slice was divided into eight segments, and each of these segments was subdivided into subendocardial and subepicardial layers. The analysis consisted in numbering the segments showing hypoperfusion at equilibrium as witness of tissular no-reflow. The determination of hypoenhancement was made by visual assessment assisted by gray scale and image contrast adjustment. Analysis of the first 40 cases showed a good interobserver correlation for percentage of hypoperfused segment determination (correlation coefficient = 0.97) as well as for normal perfusion definition (correlation coefficient = 1.0). The perfusion of each segment was classified as either normal or hypointense. Global normal perfusion was defined as less than 5% of segments showing hypoenhancement.
The reperfusion curve was established by plotting the percentage of patients with normal perfusion at day 1, day 2, day -3 and -4, day -5 and -6,day -7 and -8, day -9 to -15, day -16 to -30, day -60 to -120 and more than 120 days.
Infarct size
The gadolinium delayed enhancement analysis was performed using a thirty-two segment model consisting in dividing each short axis slice in eight segments each of them were also divided into four different layers and scored according to the transmural extent of gadolinium delayed enhancement ( nothing = 0, 0 to 25% = 1, 26 to 50% = 2, 51 to 75% = 3 and 76 to 100% = 4). The infarct size was determined in terms of percentage of the left ventricle involved by delayed enhancement. Again a good interobserver correlation was achieved (correlation coefficient = 0.96).
Statistical analysis
The reperfusion curve was established according to the percentage of patients with normal perfusion in each group. The statistical significance of the reperfusion curve was assessed by a nonparametric Spearman rank correlation. Differences between groups were assessed with χ2 tests and non-parametric ANOVA (Kruskal Wallis) for continuous data.
Results
One hundred forty-six (N= 146) consecutive patients were enrolled in the study and underwent at least one CMR perfusion examination between the achievement of TIMI- 3 flow by emergency PCI and the fourth month post-MI. A total of 184 CMRs were analysed and thirty-eight patients had CRM after day-60.Patients characteristics are presented in Table 1 and 2. Eighty-six percent were male and their mean age was 59.5±12.9 years. Their risk factors were typical of the coronary artery disease population and their mean ejection fraction, measured at the initial CMR, was 48.8±10.7%. The mean time elapsed between MI onset to TIMI 3 was 5.2±2.6 hours and 42% of the patients had thrombolytic therapy prior to emergency PCI. Statistical analysis showed no significant differences between subgroups in terms of age, gender, risk factors, MI location.
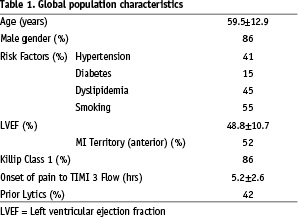
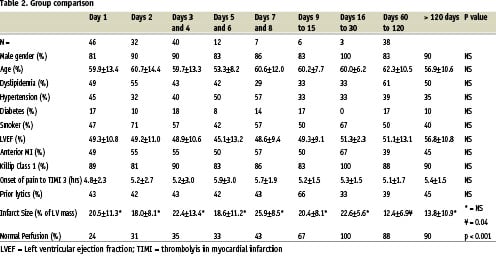
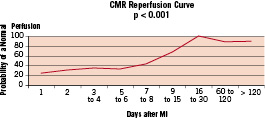
Figure 1.
The reperfusion curve (Figure 1) showed a relatively low probability of normal first-pass perfusion in the first group of early imaged patients, with only 24% of them achieving normal perfusion. This probability increased progressively over time with respectively 31%, 35%, 33% and 43% of normal perfusion in the second, third, fourth and fifth group. This probability increased to 67% beyond week-2 after MI, and reached a 100% probability beyond at week-3. after MI. The statistical analysis was strongly significant according to a non parametric Spearman rank correlation (Spearman’s rho (-0.471), p <0.001). The non parametric ANOVA (Kruskal Wallis) analysis was also strongly significant (p<0.001).
The reperfusion normalisation sequence in a patient imaged on day 2, and 60 is depicted in Figure 2a, 2b respectively.

Figure 2a.

Figure 2b.
Discussion
This study clearly demonstrates that despite restoration of TIMI-3 flow in the infarct-related artery, early recovery of myocardial perfusion assessed by CMR remain very uncommon (26% at day 2, 35% at day 4). Additionally, the present study shows that myocardial perfusion progressively increases over time to recover normal values at week 3 after successful PCI.
These data showing impaired flow early after successful PCI are in accordance with recently published data by Taylor et al. which showed an even higher rate of gadolinium first-pass anomaly (in more than 90% of patients) partly explained by an earlier imaging (within the first 24 hours after MI onset)10.
Microvascular obstruction may also be accurately evaluated by contrast echocardiography15. Some studies have shown its potential to evaluate the extent of myocardial no-reflow immediately after PCI along with its inherent role in predicting functional recovery16,17.
Contrast echocardiography, beside confirming a high rate of microvascular obstruction early after reperfused MI, also showed that when performed at a distance from acute event, microvascular obstruction tends to disappear18. However, the timing of microvascular reperfusion was not so far accurately described.
The present study confirms the transient nature of micro vascular obstruction observed after reperfused acute MI. Our data demonstrate that even in the presence of a normal TIMI- 3 flow, myocardial perfusion is slowly and progressively restored, and that achievement of complete reperfusion requires up to 3 weeks. Micro vascular reperfusion analysis have been studied in animals using CMR , but these studies were performed in small sample size population of animals, with short follow-up and reperfusion kinetics were not specifically established3,12,14. To our knowledge, this is the first study that accurately describes the kinetics of reperfusion in humans.
Interestingly, we observed a decrease in average infarct size over time in patients having had both early and late CMR. This finding is consistent with recently published literature who showed a decrease in infarct size in the months following MI15-17.
This study has important inherent limitations in its design. Achievement of normal perfusion cannot be predicted at a given time in a given patient. In contrast, the probability of perfusion restoration may be adequately assessed in a population of reperfused AMI- patients. Indeed, the high number of patients in this study allowed enough power to produce a reliable predictive value.
Nevertheless, it appears clear that the optimal design for such a study would have been a longitudinal follow-up of a cohort of patients scheduled for CMR at regular intervals until reaching a normal myocardial perfusion state. Such longitudinal studies are easily performed in animal models14 and would be possible though difficult to carry out in humans.
Conclusion
Despite the restoration of TIMI 3 flow after emergency percutaneous coronary intervention in humans, microvascular perfusion as assessed by CMR first-pass perfusion is very frequently abnormal within the first days after AMI. Perfusion is then progressively restored over the time in the days and weeks after achievement of TIMI-3 flow and the probability of a restored perfusion reaches its paroxysm up to 3 weeks after reperfused MI. This slope of myocardial reperfusion may be used as a reference to evaluate the effect of mechanical or pharmacological interventions.

