Abstract
Aims: This study was designed to compare the clinical and angiographic outcomes of paclitaxel-eluting stent (PES) and bare metal stent (BMS) implantation for unprotected left main coronary artery (LMCA) bifurcation narrowing.
Methods and results: From November 2003 to December 2004, the technique of kissing balloon followed by T provisional stenting was applied for distal left main coronary lesion in 49 consecutive patients with PES stents. Data from this group were compared to those from 57 patients treated with BMS during the previous year.
The procedural success rate was 100% for both groups. There were no incidents of death, stent thrombosis, Q-wave myocardial infarction (MI), or emergent bypass surgery during hospitalization in either group. Despite less acute gain (2.18±0.53 mm vs. 2.45±0.47 mm p= 0.078) in the PES group, PES patients showed a lower late lumen loss and a lower 8-month angiographic restenosis rate (6.1% vs. 35.1% p<0.0001) versus the BMS group. At 10 months, the rate of freedom from death,MI, and target lesion revascularization was 95.9±2.8% in the PES group and 66.1±6.3% in the BMS group (p<0.0001).
Conclusion: Paclitaxel-eluting stent implantation for unprotected LMCA bifurcation narrowing appears safe with regard to acute and midterm complications and is more effective in preventing restenosis compared to BMS implantation.
Introduction
Advances in techniques and equipment have made it possible to expand the use of angioplasty to unprotected left main coronary artery (LMCA) bifurcation lesions. Several techniques have been described for treatment of coronary lesions located in a major bifurcation with acceptable clinical outcomes. Recently1-4, there has been an increasing interest in stenting for LMCA bifurcation lesions, but little data are available about this therapy. However, in-stent restenosis is the main limiting factor to the long-term efficacy of coronary stenting and may be associated with increased long-term mortality of unprotected LMCA intervention5,6. The use of the recently developed drug-eluting stents, coated with substances that actively inhibit smooth muscle cell proliferation and possess anti-inflammatory properties, has led to a reduction in the incidence of coronary restenosis in studies in which they have been compared with bare metal control stents7-10. Recent reports from the T-SEARCH registry suggest that PES (Taxus, Boston, Minneapolis, USA) implantation for LMCA stenosis may lead to favorable clinical outcomes by decreasing restenosis11. However, these studies were limited by their small numbers of patients, heterogeneity of inclusion criteria, and low rates of angiographic follow-up. This report is a prospective study focused on the feasibility and the effectiveness of stenting for treatment of unprotected LMCA bifurcation lesions, and the acute and long-term results of this therapy in selected patients.
Methods
Study population
From November 2003 to December 2004, 49 consecutive patients with de novo unprotected LMCA bifurcation lesions underwent elective PES stenting (PES group). The control group consisted of 57 consecutive patients treated with BMS implantation for unprotected LMCA bifurcation lesions during the preceding one year (BMS group).
The inclusion criteria were symptomatic LMCA bifurcation lesion or documented myocardial ischemia and angiographic evidence of > 50% diameter stenosis of the LMCA distal lesion suitable for stent placement. The LMCA was considered unprotected if there were no patent coronary artery bypass grafts to the left anterior descending artery or left circumflex artery (LCX). Patients with a contraindication for antiplatelet or anticoagulation therapy were excluded. According to the principles of the declaration of Helsinski, the Study was performed in compliance with local regulations and was approved by a national ethical committee. All patients were requested to sign informed consent prior to their participation in this trial.
Stenting procedure
All the procedures were performed with the same slotted-tube Express stent (Boston Scientific Corporation). The only difference was the polymer-based elution of paclitaxel in the PES group compared to BMS group. All patients received aspirin (160 mg/day) indefinitely and a loading dose of 300 mg clopidogrel 12 hours before the procedure unless patients had already been pre-treated followed by 75 mg daily in a single dose for six months in the PES group and for one month in the BMS group. Patients received a 55 U/kg bolus of heparin with a repeat bolus of 5,000 U every 30 minutes to maintain an activated clotting time of > 250 seconds during the procedure. Administration of glycoprotein IIb/IIIa inhibitors was left to the operator’s discretion. Bifurcation lesions were treated for all patients using only the T-provisional stenting. Slotted-tube stents were deployed from the LMCA to the proximal portion of the most severe lesion (left anterior descending [LAD] or left circumflex arteries [LCx]). Then the other artery was dilated through the first implanted stent strut. Final kissing balloon dilatation was performed systematically at the end of the procedure.
Quantitative coronary angiography (QCA) analysis
Coronary angiography was performed after administering 1 mg intracoronary nitroglycerin (molsidomine). Coronary angiographic results were analyzed by two experienced angiographers not involved in the stenting procedures. Angiographic measurements were performed using the guiding catheter for magnification calibration and on line QCA system with an automated computer based system (Medis Medical Imaging System, the Netherland). We used the modified bifurcation classification from Duke and ICPS classifications systems used in the SYNTAX trial12. Quantitative analysis before and after stenting, and at 8-month follow-up was measured from diastolic frames in single, matched views showing the smallest lumen diameter and included minimal lumen diameter (MLD), reference vessel diameter (RVD), diameter stenosis (DS), and lesion length. The diameters of normal segments proximal and distal to the treated area were averaged to determine the reference diameter and adjacent normal segments were used as a reference. The acute gain was calculated as the difference between the minimal lumen diameter before and after the procedure. The late loss was defined as the difference in minimal lumen diameter after the procedure and at follow-up.
Follow-up
All patients were evaluated clinically by office visits or telephone interviews at one, three, six and twelve months. Repeat coronary angiography was routinely performed eight months after stenting or earlier if clinically indicated by symptoms or documentation of myocardial ischemia.
Definition
Procedural success was defined as a Thrombolysis In Myocardial Infarction (TIMI) grade 3, < 20% residual diameter stenosis by QCA measurements and the absence of major adverse cardiac events.In-hospital events including death, non-fatal myocardial infarction, and repeat revascularization were evaluated. Angiographic restenosis was defined in a dichotomic manner as >50% diameter stenosis in a parent vessel or side branch at 8-month follow-up angiography. The cumulative rates of event-free survival (death, non fatal myocardial infarction, target vessel revascularization) were analyzed during the follow-up period.
Statistical analysis
Data are expressed as mean±1 SD for continuous variables, and as frequencies for categorical variables. For continuous variables with non-normal distribution like late loss, data are presented a median and interquartile range (IQR). Continuous variables were compared by unpaired Student t test or Mann and Whitney non parametric test and categorical variables by chi-square test. Major adverse cardiac event-free survival distributions were estimated according to the Kaplan-Meier method. The log-rank test was used to compare MACE-free survival between the two groups. A p value < 0.05 was considered to represent a significant difference. All comparisons were based on two sided test. Statistical analysis was performed on SAS statistical software (SAS/STAT user’s guide, release 6.12; SAS Institute Inc).
Hazards ratios for MACE occurring were determinated in univariate and multivariate analysis with use of semi parametric Cox proportional hazards models. All variables associated with occurrence of MACE in univariate analysis at a level p<0.10 were introduced in the multivariate model. We performed a backward stepwise regression. The level for removing variable was p=0.05.
Results
Patient and lesion characteristics
The baseline clinical, angiographic characteristics and procedural data of patients are listed in Tables 1 and 2.
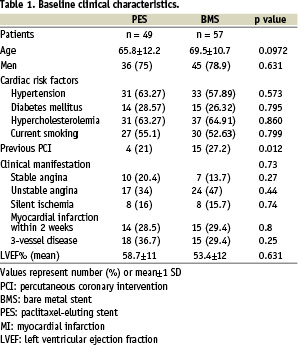
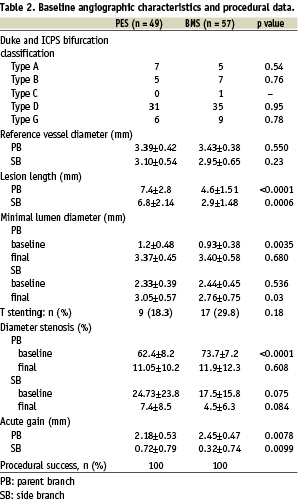
Compared to the BMS group, the PES group had more multivessel involvement and a longer lesion length in parent and side branches.
Procedural results
Procedural characteristics are summarized in Table 3.
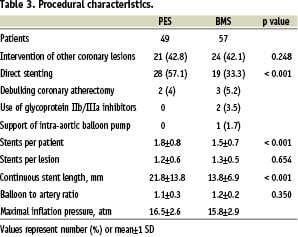
Compared to the BMS group, the PES group received more direct stenting, had more stents implanted and more segments stented. A second stent was implanted in the side branch on 9 patients of the PES group (18.3%) versus 17 patients of the BMS group (29.8%) using the T-stenting procedure (p=0.18). Debulking coronary atherectomy, intra-aortic balloon pump and GPIIb/IIIa antagonists were not used more frequently in the PES group compared to the BMS group.
The procedural success rate was 100% in both groups. Periprocedural creatine kinase-MB elevation >3 times normal developed in two PES patients and in three BMS patients. There were no incidents of death, stent thrombosis, Q-wave MI, or emergent bypass surgery during hospitalization in either group. No in-hospital complications occurred in our selected population. Quantitative angiographic results after the procedure are shown in Table 2. We found that the QCA minimal lumen diameter after procedure was larger owing to greater acute lumen gain in the parent branch of the BMS group compared to the PES group. Minimal lumen diameter increased from 1.20 mm±0.48 before angioplasty to 3.37 mm±0.45 after the procedure, whereas mean diameter stenosis decreased from 62.4%±8.2% to 11.05%±10.2% in the PES group.
Follow-up results
Clinical follow-up information was collected on all patients in the two groups. The mean clinical follow-up duration was 10±1.4 months (range 8 to 12) in the PES group and 20±13.4 months (range 16 to 32) in the BMS group. At one-year follow-up (Table 4), a total of 4 patients died in the BMS group: 1 of these patients had cardiac death (1.7%); there were no deaths and one inferior acute myocardial infarction in PES group.
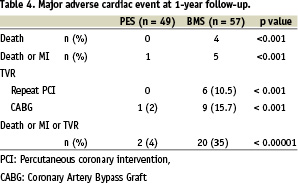
The total event rate at the end of the follow-up period, comprising cardiac death, myocardial infarction and any revascularization was 33.9% in BMS group and 4.1% in PES group. At ten months, the MACE – free survival rate was 95.9±2.8% in the PES group and 66.1±6.3% in the BMS group (p = 0.0003) (Fig. 1). MACE free survival was significantly higher in patients with implantation of PES as compared with BMS (crude HR: 0.12 [0.03-0.52] ; p = 0.005) and this association remained significant after adjustment for clinical and angiographic differences between groups (multivariate HR: 0.13 (0.03-0.65); p = 0.01).
Eight-month angiographic follow-up was performed on 56 BMS patients (98%) of 57 eligible patients and 49 PES patients (100%). The QCA results at follow-up are shown in Table 5.
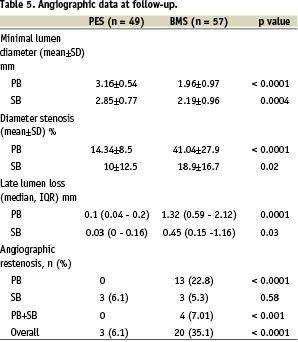
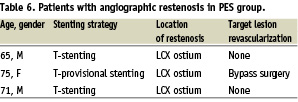
Late lumen loss (0.1 mm [0.04-0.2] vs. 1.32 mm [0.59-2.12] p=0.0001) and the overall angiographic restenosis rate (6.1% vs. 35.1% p < 0.0001) were significantly lower in the PES group compared to the BMS group. In the PES group, the three restenoses occurred in the side branch at the LCX ostium (Table 6).
Discussion
All bifurcation lesions can be treated with stents with a high rate of initial success, but with different rates of long-term outcome. The anatomic location of the LM lesion involving the bifurcation could increase the complexity of the procedure. A stepwise strategy is recommended to improve late outcome13, which seems to apply to the LM bifurcation. However, data are lacking as to the impact of stenting on long-term outcomes in this particular group of patients. Stenting of the parent vessel with subsequent balloon angioplasty of the side branch through the stent strut has been commonly used in treating coronary bifurcation lesions14. Few patients were treated with stent placement across the other artery in case of dissection or need for additional stenting, suggesting that this technique may be widely used for treatment of LMCA bifurcation lesions. Our study compared outcomes of PES with contemporary BMS implantation. The design of the current study was such that BMS patients were treated between November 2002 and October 2003 in the pre-DES era, whereas PES patients were treated in the subsequent period between November 2003 and December 2004. The study was conducted over a relatively short period (two years) and the stenting strategy (T-provisional stenting) was similar for the BMS procedure compared to the PES procedure. Our findings show that the global angiographic restenosis rate with BMS was 35.1%, and seemed to be rather high despite kissing-balloon final technique. These results are slightly higher than those of the restenosis rate of 28% of Park et al.15 due to a higher mean age (69.5±10.7 vs. 58±10 years) and a smaller reference vessel diameter of parent branch (3.43±0.38 mm vs. 3.8±0.6 mm). Predictors of restenosis after stent placement of unprotected LM coronary disease have not been studied in detail and there is only one recent study16 that comments on them. Lesions located at the distal part of LM with bifurcation involvement are associated with high risk of restenosis after stent therapy.
With the advent of DES in the clinical arena, indications for PCI were expanded and radically changed in the “real world” clinical practice. There are few reports regarding implantation of drug-eluting stents for LMCA bifurcation lesions. The principal major adverse cardiac event in survivors of LMCA angioplasty with DES remains the need for target vessel revascularization because of in-stent restenosis. Although ISR rates are much lower than those reported for BMS in the same clinical settings, rates still vary between 3% and 19% depending on lesion site (ostial, shaft or distal bifurcation), the incidence of diabetes mellitus and the number of stents used17,18. The major variable which seems to highly influence the long-term clinical outcome even with the use of DES, is still represented by the distal bifurcation with involvement of both LAD and left circumflex ostium. Left circumflex ostium is the most frequent reason for TLR following distal left main angioplasty even with the use of DES and independent of the technique used. Except T-SEARCH registry11 and Chieffo et al. results18 which involved small populations, included emergent intervention or protected LMCA stenoses, and had limited angiographic follow-up, there are few data about clinical and angiographic outcome of LMCA bifurcation narrowing treated with DES. So, the present study only included elective patients with unprotected LMCA bifurcation lesions and found that PES as BMS implantation was safe, was associated with a low procedure-related complication rate, and was followed by no episodes of death or stent thrombosis. The two groups are not totally similar in terms of clinical and procedural characteristics:
older age (69.5 vs 65.8 years ; p = 0.09), higher previous PCI (27% vs 21% ; p = 0.012), higher frequency of unstable angina (47% vs 34% ; p = 0.016), more stenting procedures of the side branch (29.8% vs 18.3%) in BMS group but in the other hand more multivessel disease and longer lesion in PES group. So, the target vessel revascularization rate of 2% and the restenosis rate of 6.1% in the PES group were less than after BMS implantation, indicating that PES is more effective in preventing in-stent restenosis compared to BMS. These results indicate that PES implantation may be very effective in suppressing intimal growth even in complex LMCA bifurcation lesions and may lead to an excellent long-term
clinical outcome.These findings confirm also in this high-risk population the strong relationship between angiographic late loss and target lesion revascularization after coronary stent implantation19. However, a prospective study with sirolimus-eluting stents (SES)20 for treatment of coronary bifurcation lesions shows a total restenosis rate at 6 months of 25.7% without significant differences between the double stenting (28%) and the provisional side-branch stenting (18.7%) groups. Moreover, a drug-eluting stent could potentially improve some of the late mortality associated with restenosis, but should not affect the high mortality associated with the substantial comorbidity of these patients going into the procedure. Recently, Park et al.21 compare the clinical and angiographic outcomes of sirolimus-eluting stent and bare metal stent (BMS) implantation for unprotected left main coronary artery (LMCA) stenosis in 102 and 121 patients respectively. In this study, there were no difference between incidents of death, stent thrombosis, Q-wave myocardial infarction (MI), or emergent bypass surgery during hospitalization in the two groups despite less acute gain in the SES group and a lower six-month angiographic restenosis rate (7.0% vs. 30.3%, p < 0.001) versus the BMS group. In the present study, the overall restenosis rate in bifurcation lesions of 6.1% (3/49 pts) after PES implantation indicates that treatment of bifurcation lesions remains challenging even in the era of drug-eluting stents22. However, the present results showing very low restenosis rates in the main vessel and a very low frequency of target lesion revascularization indicate that the LMCA bifurcation may become an inviting target for percutaneous intervention with PES.
Study limitations
The findings are based on a relatively short-term, single centre observational study and could be biased due to selection of interventional cardiologists with prior recognized experience with LMCA stenting. Furthermore, it is not a randomized trial and the number of study patients was too small to generalize our results to all patients with LMCA bifurcation lesions. However, the present study provides important new information regarding the safety and effectiveness of PES implantation for unprotected LMCA bifurcation
narrowing.
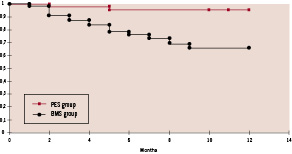
Figure 1. Kaplan-Meier curves for ten-month MACE-free survival in patients treated with Paclitaxel-eluting stents (PES group) and bare metal stents (BMS group). A statistically significant difference [HR: 0.13 (0.03 – 0.65) ; p = 0.01] was observed between the two groups. MACE: major adverse cardiac event including death, myocardial infarction and target-vessel revascularization.
Conclusion
Although surgery remains the reference method for revascularization, the whole clinical and anatomic spectrum of unprotected LM coronary artery bifurcation narrowing can be treated safely with PES and is associated with acceptable morbidity and mortality rates. In the near future, PES could become an effective option opening new horizons in the management of patients with LMCA disease and encourage the undertaking of a large, long-term, multicentre randomized study to compare PES implantation and bypass surgery for unprotected LMCA bifurcation lesions.

