Background
Computed tomographic angiography (CTA) is a robust non-invasive imaging technology which can provide detailed 3-Dimensional assessment of cardiac structure and function1-23. CTA provides extensive cardiac and vascular detail with simultaneous visualization of coronary arteries, coronary veins, cardiac chambers, and thoracic vasculature with definition of the 3-Dimensional relationships between these structures. Advances in CTA spatial and temporal resolution, electrocardiographic triggering and 3-Dimensional software, have allowed for the detailed assessment of coronary vessel anatomy1-18-23.
With the increased use of the coronary veins for cardiac electrophysiology procedures, mitral valve replacement procedures and revascularization, greater attention has been focused on details of coronary venous anatomy24-30. Individual variation in cardiac venous anatomy dictates potential sites of coronary venous pacing lead placement, making detailed anatomic definition of the coronary veins important to the deployment of coronary venous leads or devices that are situated in the great cardiac vein, middle or anterior intercardiac veins or coronary sinus. CTA can visualize and characterize the coronary sinus and its tributaries31-36. The study can provide detailed road maps for intervention in the coronary venous system, with assessment of coronary sinus os location and size, coronary sinus tributary os diameters, vessel diameter, angulations of branches off the coronary sinus/great vein, coronary venous anomalies, and 3-Dimensional localization of the corresponding myocardial segment overlying a specific point in a coronary vein branch vessel. In segments where the coronary arteries and veins overlap, the study can provide spatial details defining which vessel is closer to the myocardium (Figures 1-2).
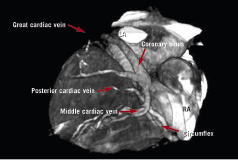
Figure 1. The relationship between the circumflex coronary artery and coronary sinus/great cardiac vein are displayed. The great cardiac vein is lateral and covering the circumflex only in one small area, not problematic for procedures involving the mitral annulus. The middle and lateral veins are also displayed. LA=left atrium, RA=right atrium.
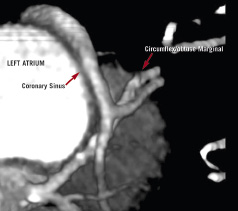
Figure 2. The relationship between the circumflex coronary artery and coronary sinus/great cardiac vein are displayed. The great cardiac vein is lateral and covering the circumflex for a longer distance of the circumflex and obtuse marginal. LA=left atrium, RA=right atrium.
Additionally, CTA can provide 3-Dimensional quantitative assessment of chamber volumes, regional wall thickening and wall motion and biventricular ejection fraction5,6,9,10,37-53.
Mitral annular procedures
For patients undergoing CS lead placement for mitral annular procedures, the relationships between the CS, circumflex and mitral valve annulus can be seen in two or three dimensional images. Thus, patients undergoing these procedures can have pre-procedural assessment to evaluate whether the circumflex position will be problematic.53 CT allows visualization of the mitral valve annulus, chordae tendonae, papillary muscles, as well as the moderator band and the tricuspid valve. Measurements are very accurate, to 0.10 mm because this is computerized data, there is no need to calibrate the image, with high in-plane spatial resolution.
Aortic valve procedures
The aortic valve is an easy valve to visualize on cardiac CT. Visualization of bileaflet, trileaflet, thickened, and calcified valves are quite robust (Figures 3-4).
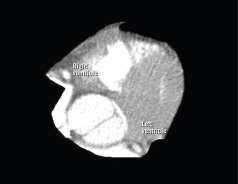
Figure 3. Bicuspid Aortic Valve. The aortic valve is well visualized and diameters of the aortic root can be measured to 0.1 mm accuracy.
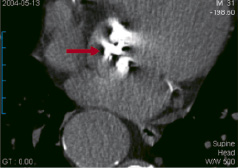
Figure 4. Severe aortic calcification. The white areas seen overlying the aortic valve represent severe calcifications.
We are able to define the anatomy both the aortic root and see the entire aorta in one image. The valve areas can be measured, and the relationship of the valve to surrounding structures is possible. We can see the valves open and close, planimeter the valves areas, however CT cannot accurately evaluate aortic valve gradients or regurgitation. The ability to see all the chambers of the heart simultaneously is somewhat advantageous. These images are intrinsically 3-D, and can be rotated in space and seen it from multiple angles. The 64 detector scanners will give even higher resolution images and even better visualization of the papillary muscles, the coronary sinus and its relationship to the mitral valve as well as the mitral valve plane.
Perhaps the most potential important use of CT for valve evaluation will be aortic valve calcification (AVC) assessment. CT allows for the most accurate and sensitive evaluation of AVC of any imaging modality (Figure 4).54-55
Comparison to Magnetic Resonance Imaging (MRI)
In contrast to cardiac MRI, cardiac CT study times are brief and patients with pacemakers, defibrillators and other metal structures can be safely studied without difficulty. Claustrophobia is not a problem, and no sedation is required. These attributes make this technology well-suited to research and clinical management in patients planning to undergo transcutaneous valve surgery.
Conclusions
Metal objects, including prosthetic valves, pacemaker wires, defibrillators and other implantable devices pose no problem for imaging with CT. Cardiac CT can assess 3-D-relationships prior to and after device implants. CT can evaluate relationships between different cardiac structures, coronary sinus/valves, coronary arteries/veins, aortic root/pulmonary outflow tract/aorta/atrial septum, that should provide useful data to the surgeon or cardiologist performing valve repair or replacement. CT angiography has been demonstrated to be at least 90% accurate in the depiction of coronary stenosis, when compared to invasive coronary angiography. In depth and accurate knowledge of the coronary artery anatomy (Figure 5) may provide useful data that facilities the procedure. Coronary artery and venous data is available on the same image set acquired to evaluate the myocardium, ejection fraction and cardiac structures and morphology.
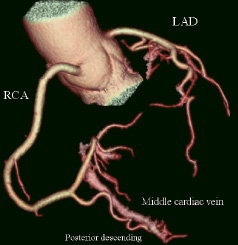
Figure 5. A three dimensional reconstruction of the coronary arteries, demonstrating the entire coronary tree, including the posterior descending. The middle cardiac vein is seen next to the posterior descending artery. Venous and arterial relationships are easy to establish on cardiac CT, as contrast fills both. LAD = left anterior descending; RCA = right coronary artery.