Introduction
It is known that myocardial ischaemia and infarction leads to severe metabolic and electrophysiological changes that induce silent or symptomatic life-threatening arrhythmias. Sudden cardiac death is most often attributed to this pathophysiology, but many patients survive the early stage of an acute coronary syndrome (ACS) reaching a medical facility where the management of ischaemia and infarction must include continuous electrocardiographic (ECG) and hemo- dynamic monitoring, and a prompt therapeutic response to incident sustained arrhythmias. During the last decade, the hospital locations in which arrhythmias are most relevant have changed to include the cardiac catheterization laboratory, since the preferred management of early acute ACS is generally interventional in nature. However, a large proportion of patients are still managed medically.
Both atrial and ventricular arrhythmias may occur in the setting of ACS and sustained ventricular tachyarrhythmias (VAs) may be associated with circulatory collapse and require immediate treatment. Atrial fibrillation (AF) may also warrant urgent treatment when a fast ventricular rate is associated with hemodynamic deterioration. The management of other arrhythmias is also based largely on symptoms rather than to avert progression to more serious arrhythmias. Prophylactic antiarrhythmic management strategies have largely been discouraged.
Although the mainstay of antiarrhythmic therapy used to rely on antiarrhythmic drugs (AADs), particularly sodium channel blockers and amiodarone, their use has now declined, since clinical evidence to support such treatment has never been convincing. Therapy for acute coronary syndrome and arrhythmia management are now based increasingly on invasive approaches. The changes in the clinical approach to arrhythmia management in ACS have been so substantial that the European Heart Rhythm Association, the Acute Cardiovascular Care Association and the European Association of Percutaneous Cardiovascular Interventions established a task force to define the current position.
Mechanisms of ischaemia-related ventricular arrhythmias
Generation of the ventricular action potential by voltage and sub-strate dependent ion currents is the basis for the contraction of each individual myocardial cell. This ionic balance can be disturbed by insults, such as ischaemia/reperfusion.
Arrhythmogenesis early in the course of an ACS, manifested as often polymorphic ventricular tachycardia (VT) or ventricular fibrillation (VF) is observed in a minority of patients with acute ischaemia and is often associated with genetic predisposition.1 Incidence of in-hospital mortality due to acute heart failure or VT/VF has declined markedly with the widespread use of reperfusion strategies.
Acute myocardial ischaemia leads to adenosine tri-phosphate deficiency, anaerobic glycolysis causing acidosis, elevation of extracellular potassium (K+), and lysophosphatidylcholine accumulation. This multifactorial sequence of events results electrophysiologically in (i) ionic imbalance: (a) shorter duration of the action potential by activation of the substrate related potassium current: IKatp and (b) less reduced resting membrane potential through inhibition of the inward rectifying potassium current: IK1; (ii) less contractile force by events that culminate in the mishandling of intracellular calcium (Ca2+); and (iii) a reduced conduction velocity because of less functional gap junctions.2
Myocardial reperfusion may cause profound electrophysiological alterations, dependent on the prior duration of ischaemia. A VT occurs more frequently with increasing duration of ischaemia, but later in the course of an ACS, and with extensive myocardial damage, the incidence of VT declines. Important contributors involved in arrhythmogenesis are the Na+/Ca2+ exchange pump, the slowly activating delayed rectifier K+ current and phosphorylation of sarcoplasmic reticulum proteins by CAMKII (calcium and calmodulin-dependent protein kinase II).3 The intracellular Ca2+ overload (among others caused by reactive oxidative stress) will result in spontaneous Ca2+ oscillations (calcium overload paradox) that trigger early and delayed after depolarizations induced ectopic beats. In addition, they will contribute to spatial and temporal dispersion of repolarization (variation in the action potential duration) and to re-entrant arrhythmias based on unidirectional conduction block, fractionation of cellular electrograms, and short action potential durations. For arrhythmogenic mechanisms, the currents flowing from the ischaemic/reperfused to the non-ischaemic zones are most important.
The mechanisms responsible for the initiation of these VA may differ based on the underlying disease (Figure 1)4: (intramural) re-entry in ischaemia, whereas triggered activity appears to be the dominant mechanism in reperfusion.5 Also when looking at the responsible mechanism for VT perpetuation, their role may differ but they contribute both to the severity of the arrhythmia and to sudden cardiac death.
Figure 1. Scheme of drivers for arrhythmias in acute coronary syndromes.Apre-existing substrate for ventricular arrhythmias, either secondary to an old myocardial infarction, due to a cardiomyopathy, or secondary to a genetic predisposition to ventricular arrhythmias, interacts with acute ischaemia, autonomic tone, and acute left ventricular strain to create triggered activity and ventricular arrhythmias.4 ARVC: arrhythmogenic right ventricular cardiomyopathy; DCM: dilated cardiomyopathy; HCM: hypertrophic cardiomyopathy; VF: ventricular fibrillation; VT: ventricular tachycardia; WPW: Wolf-Parkinson-White syndrome (Adapted from Heart, Kirchhof P, Breithardt G, Eckardt L. Primary prevention of sudden cardiac death, 92, 1873-8, Copyright 2006, with permission from BMJ Publishing Group Ltd and from J Cardiovasc Pathol, 19, Basso C, Rizzo S, Thiene G. The metamorphosis of myocardial infarction following coronary recanalization, 22-8, Copyright 2010, with permission from Elsevier).
Incidence, predictors, and outcomes of sustained ventricular arrhythmias in patients with acute coronary syndrome
Sudden death due to sustained VA is common in patients suffering from an untreated myocardial infarction (MI). In fact, electrical cardioversion (CV)/defibrillation and management of acute volume overload were the principal life-saving measures in the coronary care units before the advent of reperfusion therapies, beta-blockers, antithrombotic therapy, and statins.6 The electrical changes in acutely ischaemic myocardium, and especially in the border zone of an evolving MI, initiate and maintain these arrhythmias (see above). Prompt and adequate revascularization therapy, usually by interventional reopening of occluded vessels and stabilization of the culprit lesion with a stent, combined with initiation of adequate secondary prevention therapies (statin, dual antiplatelet therapy, beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers) aimed at preventing subsequent acute coronary events,4 have markedly reduced these life-threatening events in modern coronary care units. Patients who present with sustained VA in the first few days after a MI can hence be characterized by the following features, summarized in Figure 1:
(1) Late presenters (i.e. patients in whom reperfusion therapy was delayed due to an insufficient chain of care from first onset of symptoms to transfer to an acute coronary care centre, or long patient-related delay, severe acute ischaemia in Figure 1).
(2) Patients in whom revascularization was not or only partially successful due to technical difficulties (severe acute ischaemia in Figure 1).
(3) Patients who carry an arrhythmogenic substrate prior to the acute event, either due to a prior infarction or due to a predisposition to electrophysiological instability (‘pre-existing myocardial damage’ in Figure 1).
LATE PRESENTERS
Even in highly developed healthcare systems, only 70-80% of patients who present with ST-elevation myocardial infarction (STEMI) receive reperfusion therapy.7 Some patients never reach out for help to the healthcare system, while the diagnosis is delayed in others. Yet others will present with VF or syncope as the initial sign of the acute event, necessitating adequate resuscitation. High maximal creatine kinase (CK) values, Q waves on the ECG, markedly reduced left ventricular (LV) function in the sub-acute phase after a MI and a long history of symptoms attributable to the infarct prior to first treatment are good markers for these patients once they have reached the hospital. Patients at high risk in the setting of an ACS, easily assessed by clinical risk scores such as GRACE or TIMI,8-12 are likely to suffer from larger myocardial damage, especially when the ECG shows prominent ischaemic changes, the patient presents with persistent symptoms after initiation of therapy, or CK/troponin release patterns suggest extensive myocardial damage. These patients are at increased risk of sustained VA.13
INCOMPLETE REVASCULARIZATION
Rapid revascularization of the culprit lesion is often feasible, but may sometimes pose technical challenges, e.g. in highly calcified or bifurcated lesions. Furthermore, about 30-40% of STEMI patients and 70-80% of those with STEMI and cardiogenic shock present with a relevant stenosis in the non-culprit vessel.14 These patients remain at risk for recurrent ischaemic events even after the acute revascularization procedure and seem to be at increased risk for sustained VA.14 A careful review of the coronary anatomy can identify these patients. Emerging data suggest that early completion of revascularization may be beneficial, but further data are needed.15
ARRHYTHMOGENIC SUBSTRATE PRIOR TO THE INDEX EVENT
Most patients survive their first ACS. Owing to progression of arteriosclerosis, a second acute event will often occur despite maximal preventive therapy. Patients who suffer from an acute coronary event with pre-existing reduced LV function and myocardial scars are at risk for sustained VA in the acute and sub-acute phase of a MI. Echocardiographic signs of markedly reduced LV function or ECG signs of an old MI can identify such patients. Furthermore, patients with increased sympathetic activity, or taken to the extreme of cardiogenic shock, are at increased risk of sustained VA in the setting of a ‘recurrent’ acute coronary event. Recent evidence supports the assumption that sustained VA in the setting of an ACS is also dependent on an individual genetic predisposition to such events. This is most obvious in patients with inherited cardiomyopathies that confer electrical instability (Figure 1),4 but may also be mediated by common genetic variants.1,16
Recommendations for evaluation of patients with acute coronary syndrome at risk for ventricular tachyarrhythmia
Patients with acute coronary syndrome who present with either of the following conditions
– late from the onset of the symptoms,
– incomplete revascularization,
– presence of substrate prior to the event,
– or those patients with complications,
should be considered at increased risk for arrhythmia development during initial evaluation.
Antiarrhythmic therapy in patients with sustained ventricular arrhythmias and acute coronary syndrome
The incidence of sustained VT and VF occurring within 48 h of the onset of an ACS seems to have decreased over the past decades.17-19
This is most likely due to the widespread availability of revascularization therapy, limiting the size of infarction and to an increased use of beta-blockers.8 However, in a recent retrospective analysis of two randomized trials sustained VA occurred in almost 6% of patients in the very early phase of acute MI indicating the significance of VT/VF in this situation.20 The role of AAD therapy for the treatment of sustained VT/VF in ACS has been strongly debated and questioned.17 Only limited data exist from clinical trials concerning the use of AADs in ACS. Most of the reports available are limited by (i) uncontrolled patient selection, (ii) multiple-pragmatic treatment regimens, (iii) small sample size, (iv) variable endpoints, and (v) at least partially by some degree of selection and outcome bias. Controlled randomized trials comparing different AADs in ACS are completely lacking.
The nature of VT/VF in the setting of ACS is complex, dynamic, and different from the chronic phase of MI (see above).21,22 Variable degrees of ischaemia and reperfusion may be present which significantly affect both arrhythmia mechanisms and –even more importantly– the effects of AADs. Almost all AADs act either in a voltage or rate-dependent manner, and some drugs have both characteristics. Thus, AAD action may be significantly altered in ischaemic/reperfused myocardium as compared with non-affected myocardium. This may result in significant electrophysiological heterogeneity and gradients in conduction and refractoriness.
If ischaemia is suspected to be responsible for the arrhythmia, immediate reperfusion is of utmost importance.23 Early use of beta-blockers in the setting of ACS reduces mortality and the incidence of VA and is therefore recommended.17,24 Similarly, correction of hypomagnesaemia and hypokalaemia is encouraged because of the potential contribution of electrolyte disturbances to VA. Statin therapy reduces mortality in patients with coronary heart disease and is therefore part of the recommended routine medication. Early and intensive statin therapy has been reported to reduce the incidence of premature ventricular complexes (PVCs) and non-sustained VA.25
Antiarrhythmic drugs are widely used, but are of modest efficacy and have important side effects. Only sparse data exist to guide AAD therapy for sustained VA related to ACS. However, overwhelming data exist that have shown the potential harm of most AAD therapy for patients with ischaemic heart disease.26 Nevertheless, even with the advance of non-pharmacological treatment options as catheter ablation, temporary or chronic AAD therapy may still be considered for the treatment of refractory VA. Initial attempts to tackle VT/VF in ACS, even when recurrent, should be electrical CV/defibrillation. Antiarrhythmic drug treatment should be considered only if episodes of VT/VF are frequent and can no longer be controlled by successive CV/defibrillation. Especially in patients with recurrent VT/VF triggered by PVCs arising from partially injured Purkinje fibres, catheter ablation has been shown very effective and should be considered (see catheter ablation in ACS).27
Lidocaine is a class I AAD that may reduce the incidence of VA related to myocardial ischaemia, although no beneficial effect on early mortality has been demonstrated.28 Because of potential proarrhythmia, with a trend towards excess mortality, prophylactic treatment with lidocaine has largely been discouraged.17 On the other hand, prophylactic treatment with lidocaine after cardiac arrest and successful resuscitation has shown significant beneficial effects for both, recurrence of VA and survival.29 However, others reported a lower risk of death at 24 h after thrombolysis and prophylactic lidocaine and a neutral effect on overall mortality.30 Recent analysis of GUSTO IIB and III studies has shown reduced early mortality in patients with VF/VF after acute MI and a neutral effect on 30-day mortality.20 Considering the overall efficacy and side effects, lidocaine should be considered as an AAD for the acute intravenous management of recurrent VT/VF in ACS.
Amiodarone is a class III AAD with multiple additional electrophysiological properties. When AAD therapy is necessary in patients with severe structural heart disease, amiodarone may have the most balanced efficacy-to-risk profile. In a pooled database from two similar randomized clinical trials (the European Amiodarone Myocardial Infarction Trial and the Canadian Amiodarone Myocardial Infarction Trial), that evaluated use of amiodarone in primary prevention in patients recovering from MI, cardiac death and arrhythmic death or resuscitated cardiac arrest were significantly lower in patients receiving amiodarone, compared with placebo, if they were also receiving beta-blockers. There appeared to be no benefit of amiodarone over placebo in patients not receiving beta-blockers.31 However, even amiodarone treatment resulted in excess mortality when given over long periods to patients with advanced heart failure.32 It belongs therefore to the few AADs that are considered to have no or little effect on long-term prognosis when given to patients with severe structural heart disease and/or extensive MI. In the context of ACS, amiodarone therapy –compared with lidocaine– retrospectively has shown an increased short- and long-term mortality.20 On the other hand, in the setting of out-of-hospital cardiac arrest, amiodarone was associated with better survival to admission rate as compared with lidocaine in patients with refractory to shock therapy VF.33 Amiodarone should be considered for the suppression (intravenous or oral) and prevention (oral) of recurrent arrhythmias along with beta-blockers.
Flecainide, propafenone, and ajmaline exert their antiarrhythmic potential by significant slowing of conduction. In the setting of ACS, these effects may result in aggravation rather than termination of VT/VF. The antiarrhythmic potential of these AADs for the suppression and termination of VA has been mainly studied until the 1990s.34-37 However, in the setting of ACS, these drugs may cause an aggravation of VT/VF. After the publication of the CAST trial that has shown an increased mortality in patients after MI treated with encainide, flecainide, or moricizine as compared with placebo, further research to class IAAD and VA has largely been abandoned.26 Thus, these drugs should not be used in ACS.
Dofetilide and azimilide are class III AADs that prolong cardiac repolarization and refractory period with proven efficacy on the suppression of VA.38-40 The treatment with azimilide did not affect the mortality of patients with a recent MI and an LV ejection fraction of 15% to 35%.41 Only few data exist on the use of dronedarone for the treatment of VA; however, an increased mortality has been reported in patients with AF and heart failure treated with dronedarone.42 All class III AADs increase the QT interval with a risk for torsade de pointes tachycardias. However, none of these drugs had been specifically investigated for the treatment of VA related to ACS and can thus not be recommended for this indication.
Ranolazine is a piperazine derivative with a chemical structure similar to that of lidocaine. The MERLIN-TIMI 36 study randomized 6560 patients with ACS to ranolazine or placebo.43 Although there was no significant difference in the combined primary endpoint of cardiovascular death, MI, or recurrent ischaemia, the incidence of non-sustained VT (<30 s) was significantly reduced by ranolazine compared with placebo.43,44 The role of ranolazine as an AAD is nevertheless still investigational.45
Recommendations for antiarrhythmic therapy in patients with acute coronary syndrome and ventricular tachyarrhythmia
For patients with acute coronary syndrome (ACS) without ventricular arrhythmias, prophylactic antiarrhythmic drug treatment should not be administered.
– If life-threatening ventricular arrhythmias related to ACS occur despite optimal revascularization, early treatment with beta-blockers, balancing electrolytes, and sedation to reduce sympathetic drive and/or overdrive stimulation, repetitive electrical cardioversion/defibrillation should be considered first.
– If antiarrhythmic drug therapy is necessary on top of these measures for the acute treatment of recurrent ventricular arrhythmias related to ACS after failure or non-availability of other treatment capabilities, administration of intravenous amiodarone is reasonable, followed by intravenous lidocaine, if necessary (Figure 2).
Figure 2 Treatment recommendations for recurrent VT/VF and electrical storm in ACS. ACS: acute coronary syndrome; ICD: implantable cardioverter-defibrillator; LVAD: left ventricular assist device; VF: ventricular fibrillation; VT: ventricular tachycardia
– When experience is available, early catheter ablation should be considered when other treatments fail (see below).
– Ventricular tachyarrhythmia in the first minutes after successful reperfusion therapy can be transient without need for treatment, known as reperfusion arrhythmias.
– If frequent premature ventricular complexes and non-sustained ventricular tachycardia continue despite successful reperfusion therapy under sufficient beta-blocker therapy, they should only be treated if hemodynamically important. This treatment should follow the same principles as the treatment of sustained VA.
How to manage electrical storm and inappropriate implantable cardioverter-defibrillator shocks in patients with acute coronary syndrome
In patients with ACS, electrical storm and inappropriate implantable cardioverter-defibrillator (ICD) shocks are associated with poor prognosis.46-49
Electrical storm is defined as the three or more episodes of VT or VF in any 24-hour period.46,50 It results from interplay between pre-existing vulnerable substrate and acute triggers. It is a rare but very serious event and is associated with a poor prognosis.51 Most investigations failed to reveal any clear cause for the development of electrical storm. Acute ischaemia is more likely to induce VF or polymorphic VT than monomorphic VT.50
The majority of inappropriate shocks were related to supraventricular tachycardia.48,49 Both appropriate and inappropriate implantable ICD shocks were significant predictors of death, whereas no change was noted in mortality among those with anti-tachycardia pacing (ATP)-treated arrhythmias.52
ACUTE TREATMENT AND METHODS TO REDUCE INCIDENCE OF IMPLANTABLE CARDIOVERTERDEFIBRILLATOR SHOCK
Electrical storm constitutes a critical situation both on management of hemodynamically unstable arrhythmias and because it is associated with significant elevated sympathetic tone, which facilitate further arrhythmias.
The patient has to be hospitalized and monitored in an intensive care unit. The most effective treatment is to reverse the ischaemia with emergency coronary revascularization or with anti-ischaemic, antithrombotic (antiplatelet, anticoagulant) agents. The intravenous administration of magnesium and potassium may be undertaken in patients with QT prolongation or hypokalemia. The suppression of malignant arrhythmias is an accepted indication for placement of a percutaneous ventricular assist device53 (see below).
The key intervention in electrical storm is blocking the sympathetic system through the intravenous administration of beta-blockers, especially propranolol;54 combined with sedatives, such as benzodiazepine. Intravenous analgesics and sedatives should also be given. Amiodarone has moderate negative inotropic effects, is relatively safe in patients who have heart failure and is effective as adjunctive therapy to prevent recurrent ICD shocks.55 Trials have not confirmed lidocaine is superior to other antiarrhythmics.56 If an ICD fails to convert a life-threatening rhythm, external defibrillation pads should be ready for use.
Implantable cardioverter-defibrillator programming is probably a key issue to prevent electrical storm.57 Although all devices are pre-programmed, it is important to review the device settings because these settings may be inappropriate for the individual patient.50 Patients should receive an ICD with ATP programming even if the clinical presentation was VF, or VT was not induced at the electrophysiological study (EPS).58 Programming ICD to deliver ATP for VT faster than 200/min is safe, reduces the need for shocks and improves mortality compared with conventional therapy.59 The number of VT cycles needed for detection can be increased from nominal values to allow spontaneous termination, and sustained rate duration should be prolonged or disabled. Redetection can carefully be prolonged to reduce the risk of inappropriate detection of non-sustained VT in many patients.50,60 In some cases, it may be advisable to turn off the ICD in order to avoid multiple ineffective shocks provided that the patient is strictly monitored in an intensive care unit and that CV/defibrillation might be provided in a timely fashion in case of life-threatening arrhythmias.
On the basis of the observation that VT tends to be abrupt in onset and somewhat regular (high stability), sinus tachycardia tends to accelerate gradually, and AF is irregularly irregular (low stability), it was found that programming sudden onset and stability criteria helped to discriminate supraventricular arrhythmias and reduced the risk of inappropriate shock.61 In addition, just as the surface QRS complex during VT generally differs from that during sinus rhythm, discrimination algorithms can be used.
Radiofrequency ablation of PVC originating from the Purkinje fibre network holds great promise in the treatment of electrical storm. The typical indication for ablation is VT refractory to medical therapy in patients who also receive multiple ICD shocks.52 In patients with electrical storm, catheter ablation should be considered as a treatment option at an early stage.27,62
Recommendations for management of electrical storm and inappropriate shocks in patients with acute coronary syndrome
– Initial management of patients with electrical storm requires identifying and correcting underlying ischaemia.
– Amiodarone, beta-blockers and electrolyte correction as needed form the cornerstone of antiarrhythmic therapy.
– Patients who have implantable cardioverter-defibrillator may require device reprogramming.
– A focal rescue ablation approach targeting the trigger for ventricular fibrillation early after acute myocardial infarction seems promising (Figure 2).
Catheter ablation of sustained ventricular arrhythmias in acute coronary syndrome
Incessant sustained VA that occurs in ACS is a life-threatening condition, carrying a high morbidity and mortality rate. It can be difficult to control with AADs, as class I AADs and amiodarone efficacy in reduction of mortality is controversial and time is required for amiodarone to reach therapeutic levels to provide effective rhythm control. Catheter ablation of VA during the acute phase of an ACS is rarely performed, and most ablations for incessant VA occur post-MI. However, in patients with intractable, drug-refractory VA, catheter ablation after treating the underlying ischaemia can play an important role and these patients should be referred to a specialized ablation centre.
The two main mechanisms implicated in the induction of sustained VA in ACS are macro-re-entry from heterogeneous substrate, and after-depolarizations and triggered activity from impaired but ischaemia-resistant Purkinje fibres within areas of myocardial ischaemia leading to PVC,27 and both can be targeted for ablation (Figure 3).
Figure 3. Ventricular tachycardia in a patient with an acute coronary syndrome: (A) repetitive monomorphic ventricular tachycardia two days after percutaneous coronary intervention of the circumflex artery in the setting of an acute coronary syndrome; (B) recurrent ventricular tachycardia induced by a monomorphic premature ventricular complex.
Radiofrequency ablation using an irrigated-tip ablation catheter, in conjunction with a 3D-electroanatomical mapping system is most commonly undertaken. This is done via either an antegrade transseptal, retrograde aortic or a combined approach. In the majority of cases due the sub-endocardial location of the Purkinje fibres and the ischaemic myocardial substrate, endocardial mapping, and ablation suffices. Mapping of PVCs requires that they occur frequently during the electrophysiology procedure and ideally should be performed during an electrical storm, as usual pacing maneuvers and medications are often unable to initiate ischaemia-induced PVCs. Activation mapping can then be performed, while assessing for Purkinje potentials. These low-amplitude, high-frequency signals precede the ventricular extrasystole signal by up to 160 ms at the site where the culprit PVC originates, usually in the region of the ischaemic borderzone of the MI territory.27
When spontaneous PVCs and VA are not seen, pace-mapping can be performed against PVCs recorded prior to the procedure; however, only when they are monomorphic in nature. Ablation endpoint is the suppression of the triggering PVC, as well as the loss of the Purkinje potential. Substrate-guided ablation using bipolar amplitude mapping, particularly in patients with un-mappable VA, has also been successfully reported, although the best ablation approach has yet to be defined. Ablation lines and clusters through areas of ischaemia and slow conduction to homogenize substrate, as well as circumferential ablation around substrate and substrate isolation have been described.63-69
Reported acute success rates are up to 72%, with only 6% experiencing recurrence of VA storms. Recurrence occurred more frequently in patients with monomorphic VT electrical storm, as compared with those with polymorphic VT or VF. Recurrence was also significantly reduced only in patients where all VAs were suppressed during the ablation procedure, which has been shown to be a good marker of long-term success and survival.62
Complications associated with catheter ablation of VA include cardiac tamponade, ischaemic stroke, atrioventricular (AV) block, valvular injury, cardiac decompensation, and death. Peri-procedural mortality is reported to be up to 3% in this sub-group of unstable patients, and is mostly associated with uncontrolled, intractable arrhythmia. The long-term mortality post ablation is up to 18%, mainly due to VA and acute decompensated heart failure.70
In addition, ICDs have reduced mortality from VA due to myocardial ischaemia. However, it is also clear that both appropriate and inappropriate ICD shocks confer an increased mortality rate and reduced quality of life. Thus, early ablation of patients with electrical storm, which leads to significantly decreased recurrence rates for recurrent VA, should decrease long-term morbidity and mortality associated with ICD shocks.
Catheter ablation of VA in ACS should be recommended, particularly in electrical storm; however, due to the often hemodynamically unstable nature of these patients, it is a highly complex procedure with significant associated morbidity and mortality. Therefore, it requires highly trained electrophysiologists with an excellent knowledge base and experience in VT ablation and a high volume electrophysiological laboratory to perform such procedures. To facilitate this, a referral network similar to that for ACS should be established to improve patient access to such adequately equipped hospitals.
Recommendations for catheter ablation of sustained ventricular tachyarrhythmia in patients with acute coronary syndrome
– In patients with drug-refractory electrical storm, radiofrequency catheter ablation during an electrical storm is valuable in the management of sustained ventricular tachyarrhythmia (VA).
– Ablation endpoint is suppression of the triggering premature ventricular complex, loss of Purkinje potentials, and in un-mappable VA, substrate-guided ablation can be performed.
– Owing to hemodynamic instability, these complex procedures should be performed by experienced electrophysiologists.
– When no highly experienced operator in ventricular tachycardia (VT) ablation is available, early transfer to a high volume VT ablation centre should strongly be considered (Figure 4).
Figure 4. Catheter ablation of VA in patients with ACS. AAD: antiarrhythmic drug; ACS: acute coronary syndrome; ES: electrical storm; PVC: premature ventricular complex; VA: ventricular arrhythmia; VT: ventricular tachycardia
Arrhythmias in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction
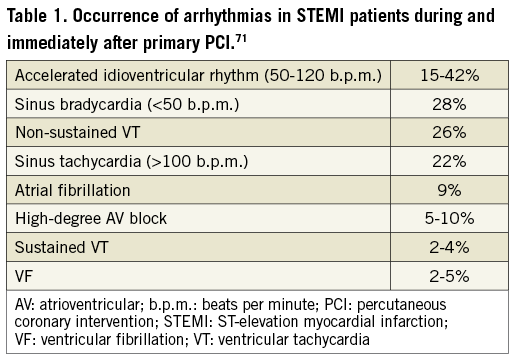
Arrhythmias and conduction disturbances are common during the early hours after an acute MI (Table 1) and a major cause of death in the pre-hospital phase.71,72 The occurrence at greatest frequency before or during primary percutaneous coronary intervention (PCI) indicates that ongoing myocardial ischaemia and reperfusion injury are major determinants for arrhythmias and conduction disturbances. Interestingly, larger infarct size is associated with occurrence of sinus bradycardia, accelerated idioventricular rhythm and sustained VT but not VF. During the primary PCI procedure, ventricular tachycardia and fibrillation should be managed according to ESC guidelines.7 In patients with cardiac arrest and who are unresponsive to conventional cardiopulmonary resuscitation, it is reasonable to use mechanical chest compression devices and emergency cardiopulmonary bypass support is reported to be feasible. In hemodynamically unstable patients with refractory incessant VT, percutaneous left ventricular assist devices (LVADs) may be appropriate (see below). Following intervention, the incidence of arrhythmias ranges from 6% to 28% for new-onset AF, 7-13% for non-sustained VT, 5-10% for high-degree AV block (≤30 beats/min lasting for ≥8 s), 7%-16% for sinus bradycardia (≤30 beats/min lasting for ≥8 s), 5% for sinus arrest (≥5 s), 3-6% for sustained VT, and 3-6% for VF according to retrospective registry data or prospective recordings from cardiac monitors implanted soon during an acute MI.73
The occurrence of AF is frequently associated with severe LV damage and heart failure. Episodes may last from minutes to hours and are often repetitive. The arrhythmia is most often well tolerated and no specific treatment is required, other than anticoagulation. In some instances, the fast ventricular rate contributes to heart failure, requiring prompt treatment using direct current cardioversion (DCCV) with further management as indicated below. Several studies have suggested that development of AF in the setting of acute MI is an independent predictor of all-cause mortality, irrespective of the treatment given.74,75 Atrial fibrillation not only increases the risk for ischaemic stroke during hospitalization but also during follow-up, and this includes patients with paroxysmal AF that has reverted to sinus rhythm at the time of discharge. Accordingly, patients with AF and risk factors for thromboembolism should be adequately treated with oral anticoagulation. Because AF will generally require anticoagulation, when choosing a stent in these patients, the benefits of drug-eluting stents on restenosis should be weighed carefully against the substantial bleeding risks that are associated with the prolonged combination of triple antithrombotic therapy (see below). Other supraventricular tachycardias are uncommon and are usually self-limiting.
Ventricular premature beats are almost universal on the first day of the acute phase and more complex arrhythmias (multiform complexes, short runs, or the R-on-T phenomenon) are common. Their value as predictors of VF is questionable. No specific therapy is required.
The long-term prognostic significance of early (<48 h) VF or sustained VT in patients with acute MI is still controversial.
In the APEX-AMI trial, VT/VF occurred in ~6% of patients with STEMI presenting for primary PCI.15 Two-thirds of these events occurred before the end of cardiac catheterization (defined as early events) and 90% within 48 h. Ventricular tachycardia/VF was not benign and was associated with substantially increased morbidity and mortality. Some of this association was related to older age, greater prevalence of comorbid conditions, and adverse presenting and post-cardiac catheterization features (ST resolution and TIMI flow) as shown by the attenuation of the risk with adjustment of these factors in a multivariate model. However, even after accounting for these variables, any VT/VF remained associated with a more than 3-fold higher risk of 90-day mortality in patients undergoing primary PCI. The prognostic significance of late VT/VF appeared to be greater than early VT/VF with more than 5- and 2-fold higher risks of 90-day mortality, respectively. Thus, these data support the prognostic importance of (any, early, or late) VT/VF as an independent and incremental risk marker, although this does not prove a cause-andeffect relationship. However, sustained VT/VF after primary PCI in the HORIZONS-AMI trial was not significantly associated with 3-year mortality or major adverse clinical events.76 Clinical management of sustained VT and VF after primary PCI is according to ESC guidelines.7
Recommendations for management of arrhythmias in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction
– Ventricular tachyarrhythmia (VA) developed during primary percutaneous coronary intervention (PCI) should be treated using direct current cardioversion (DCCV), overdrive pacing, beta-blockers and amiodarone for sustained ventricular tachycardia (VT)/ventricular fibrillation.7
– Electrolyte balance correction, beta-blockers, and amiodarone should be considered for treatment of polymorphic VT.
– For refractory VA in hemodynamically unstable patients, percutaneous ventricular assist device may be considered.
– Atrial fibrillation developed during PCI with high ventricular rate leading to hemodynamic compromise should be treated using DCCV with further management as indicated below.
Arrhythmias in cardiogenic shock complicating acute myocardial infarction
Cardiac arrhythmias including VT/VF, AF, and conduction disturbances are common in patients with acute MI complicated by cardiogenic shock and are associated with high short-term mortality.77-81 Cardiogenic shock, acute ischaemia, and the use of inotropes are main risk factors for the development of arrhythmic events.81 Therefore, correcting factors underlying cardiogenic shock, substrate, and triggers for arrhythmia, play main role in their management.17,82,83
VENTRICULAR ARRHYTHMIAS
Sustained VT occurs in 17-21% and VF is seen slightly more often (24-29%) in selected patients with cardiogenic shock and acute MI, undergoing thrombolysis or primary PCI.77,78 In cardiogenic shock, sustained VT/VF might deteriorate hemodynamic status and LV dysfunction. The goal of therapy should be to restore the rhythm immediately to avoid hypoperfusion, which leads to end-organ damage. Regardless of the cause of cardiogenic shock, sustained VT/VF must be treated promptly with DCCV without hesitation. Catheter ablation may be indicated as a salvage procedure if VT recurs (see above).27 Antiarrhythmic therapy (usually intravenous amiodarone, lidocaine) and electrolyte balance correction could be considered if necessary for acute management.17 Care should be taken with intravenous amiodarone to avoid hypotension. For selected patients with refractory VT/VF and rapidly deteriorating hemodynamic and clinical status, implantation of percutaneous LVAD and extracorporeal membrane oxygenation (ECMO)-assisted primary PCI have been found promising as a bridge to recovery, in gaining time to implement and assist appropriate therapies and prolonging survival.53,84-95 Implantation of percutaneous LVAD (Impella 2.5 assist device) in patients with MI and cardiogenic shock, as well as presenting with cardiac arrest was accompanied by reduction of tissue hypoxia, hemodynamic stabilization, and improvement of neurological outcome.84,85,93,94 Extracorporeal membrane oxygenation-assisted PCI significantly improved recovery and survival of patients with cardiogenic shock and refractory VT/VF as compared with intra-aortic balloon pump (IABP) with 69.23% of patients successfully weaning off the support in the ECMO group and only 12.5% in the IABP group (P=0.02).92 The latter is no longer recommended.96-99 The IABP-Shock II study demonstrated no beneficial effect of IABP on tissue hypoxia, time to hemodynamic stabilization, short- and long-term mortality in patients with cardiogenic shock as compared with medical treatment.98,99 Recent meta-analysis on the effect of IABP according to the type of reperfusion in patients with MI and cardiogenic shock showed overall no effect on the risk of in-hospital and long-term mortality and trend to higher risk of in-hospital death with IABP support in patients undergoing primary PCI [relative risk 1.18, 95% confidence interval (CI) 1.04-1.34].96 Intra-aortic balloon pump is not expected to work in case of VF, as there is no circulation to augment.
Proper hemodynamic support with inotropes and vasopressors is required, though caution must be taken for dopamine use, since it increases risk of arrhythmias in patients with shock,100 which are less seen with other inotropes. Coronary reperfusion is key to improving survival. Recent pooled analysis of both the SMASH and SHOCK trials82 showed that in cardiogenic shock patients, early revascularization reduced risk of death by 18% (relative risk 0.82, 95% CI 0.70-0.96) compared with the initial medical stabilization. Therefore, early hemodynamic stabilization and arrhythmia management should not delay revascularization.
ATRIAL FIBRILLATION
About 11-20% of patients with acute MI presenting with cardiogenic shock develop AF.77,78 Several mechanisms underlying cardiogenic shock can predispose to AF by creating either a substrate or a trigger for this arrhythmia. Hemodynamic changes as an increase in pulmonary capillary wedge pressure and left atrial pressure, can lead to AF. The adverse hemodynamic consequences of AF can quickly lead to a worsening of symptoms, which may be difficult to manage. Immediate DCCV should be performed to restore sinus rhythm and hemodynamic stability when cardiac output is compromised.7 Amiodarone intravenous can be used for acute rate control with caution of hypotensive effect.101 Though evidence on the efficacy of amiodarone in the setting of cardiogenic shock is limited, in one study of single bolus intravenous amiodarone use for acute rate control it also resulted in (delayed) pharmacological conversion to sinus rhythm.101 In patients with pre-existing AF on oral amiodarone therapy, it may also enhance success of DCCV.102 Other rate controlling agents must be avoided due to negative inotropic effects. In refractory cases, AV node ablation with biventricular or LV stimulation could be considered for rate control, as they have been found feasible in correction of hemodynamic derangement of patients with cardiogenic shock and severe heart failure.103,104
CONDUCTION DISTURBANCES
High-grade AV block and asystole develop in about 23-35% of acute MI patients with cardiogenic shock,77,78 especially in inferior infarctions with proximal right coronary artery (RCA) occlusion. The rate of complete heart block is much lower in adequately revascularized infarct patients, and prompt revascularization of the infarct artery should be attempted. Bradyarrhythmias are induced by either autonomic imbalance or ischaemia and necrosis of the conduction system (see section below). It is important to recognize which of them are transient and which are likely to progress to irreversible and symptomatic high-degree AV block, which has been associated with a mortality rate approaching 80% due in large part to greater loss of functioning myocardium.Temporary transvenous pacing is necessary for patients with severe and symptomatic bradyarrhythmias if they do not resolve within few minutes after reperfusion.7,105
Recommendations for management of arrhythmias in cardiogenic shock complicating acute myocardial infarction
Regardless of the type of arrhythmia, treatment of the underlying cardiogenic shock with prompt revascularization should be done as the primary procedure and should not be delayed by arrhythmia treatment.
– Acute management of ventricular tachycardia (VT)/ventricular fibrillation (VF) in the setting of cardiogenic shock includes immediate direct current cardioversion (DCCV), amiodarone, lidocaine if necessary.
– Percutaneous left ventricular assist device and extracorporeal membrane oxygenation-assisted percutaneous coronary intervention can be used in case of refractory VT/VF.
– Catheter ablation may be considered as a salvage procedure if arrhythmia persists (see above).
– Atrial fibrillation should be managed by DCCV if high ventricular rate compromises cardiac output; amiodarone can be used for rate control and assisting cardioversion.
– Atrioventricular node ablation with biventricular or left ventricular stimulation could be considered if above rate control measures fail.
– Severe and symptomatic bradyarrhythmias accompanied by hemodynamic instability require placement of temporary pacemaker if they do not resolve within few minutes after reperfusion.
Incidence, prognostic implications, and treatment of atrial fibrillation in patients with an acute coronary syndrome
Atrial fibrillation, the most commonly encountered clinical arrhythmia, often coexists with acute MI. Atrial fibrillation has been reported to complicate the course of acute MI in 2.3-21% of hospitalized patients.106 In recent years, the widespread use of early reperfusion therapy (thrombolysis and PCI) as well as the use of beta-blockers, angiotensin-converting enzyme inhibitors and angiotensin II inhibitors has led to a substantial decline in the incidence of post-MI AF. However, as the population ages and as AF increases with age, we can expect that AF will still remain a frequent and worrisome complication of acute MI.
Atrial fibrillation may already be present at the time of hospital admission for acute MI, or may develop during the hospital stay. Preexisting AF accounts for approximately one third of all cases of AF observed in patients with acute MI, and new-onset AF for the remaining two-thirds.107
Possible underlying mechanisms of AF in the setting of acute MI are atrial ischaemia or infarction, acute hypoxia or hypokalaemia, pericardial inflammation, increased LV diastolic pressure and left atrial pressure, hemodynamic impairment secondary to LV dysfunction and abnormalities of autonomic regulation.108 These mechanisms may be found alone or in combination, and may superimpose on predisposing diseases, such as previous cardiomyopathy, valvular disease, or chronic lung disease.
Once AF develops, usually there is a significant worsening of hemodynamics due to the high ventricular rate, irregular ventricular filling, and/or loss of atrial contribution to cardiac output.
Independent predictors of the occurrence of AF in acute MI include older age, elevated heart rates at admission, pre-existing AF, LV hypertrophy, presence of heart failure symptoms, and LV dysfunction. These risk factors have been described regardless of the type of reperfusion therapy (i.e. none, thrombolysis, PCI). Moreover, patients who develop AF more often have hypertension, diabetes, previous MI, multi-vessel coronary artery disease, higher levels of biomarkers of myocardial damage, and low TIMI 3 flow grade after reperfusion therapy.106,107
The prognostic impact of AF that occurs in the setting of acute MI is still controversial, with some studies describing an independent adverse effect on mortality and others failing to detect such an association.106 However, a recent systematic review and meta-analysis, including 43 studies and 278 854 patients, showed that AF carries an excess risk of in-hospital, short-term (<30 days), mid-term (>30 days to 1 year), and long-term (>1 year) mortality among patients with acute MI, with at least a 40% increase, regardless of the type of AF (pre-existing or new-onset). Increased risk included both sudden and non-sudden cardiac death. This worse prognosis persisted, in patients with new-onset AF, even after adjustment for age, diabetes mellitus, hypertension, prior MI, heart failure, and coronary revascularization.109 Moreover, according to a recent large community study, the mortality risk, in patients with new-onset AF, seems to be greatest when the arrhythmia develops later than 30 days post-acute MI [hazard ratio (95% CI) 2.58 (2.21 to 3.00) vs. 1.81 (0.45 to 2.27) for AF between 3 and 30 days, and 1.63 (1.37 to 1.93) for AF within 2 days].107
In addition to increased mortality, patients with acute MI and AF have also a higher incidence of re-infarction, cardiogenic shock, heart failure, and asystole, probably as an expression of the more severe impairment of coronary circulation and hemodynamic status when AF develops.106
Finally, AF complicating acute MI is also associated with an increased risk of subsequent ‘spontaneous’ AF, and also with an increased risk of ischaemic stroke both during hospitalization and during follow-up; even if the AF is transient and reverses back to sinus rhythm before hospital discharge.106
Literature evidence for the management of AF in the setting of acute MI stemming from controlled clinical trials is lacking, so the treatment is essentially founded on practical basis. In many cases, the arrhythmia is well tolerated and no specific treatment is required.
In other instances, the high ventricular rate associated with AF may contribute to hemodynamic impairment and heart failure, requiring prompt therapeutic intervention. Adequate rate control represents the most important first therapeutic approach in this setting, and may be accomplished either by administration of beta-blockers or possibly non-dihydropyridine calcium antagonists, either orally or intravenously. In patients with acute MI and AF associated with severe LV dysfunction or heart failure, the negative inotropic effect of betablockers or calcium antagonists may result in further impairment of pump function. In such circumstances, rate control may be achieved by intravenous administration of amiodarone and/or digitalis.7
Urgent DCCV is recommended for patients with severe hemodynamic instability or intractable ischaemia, or when adequate rate control cannot be achieved with pharmacologic agents. In this latter case, transesophageal echocardiography should be considered to exclude the presence of thrombi in left atrium. In addition to electrical CV, amiodarone can be used for restoration of sinus rhythm when the hemodynamic situation is stable. This drug is usually preferred to other AADs because of its limited negative inotropic effect. The administration of class IC AADs, instead, is considered harmful in patients with acute MI and hence is not recommended.7,110 In the post hoc analysis in patients with coronary heart disease and atrial fibrillation from the ATHENA (A placebo-controlled, double-blind, parallel arm Trial to assess the efficacy of dronedarone 400 mg b.i.d. for the prevention of cardiovascular Hospitalization or death from any cause in patiENts with Atrial fibrillation/atrial flutter) trial, dronedarone reduced all-cause mortality, cardiovascular hospitalization, and the first ACS event. However, experience with dronedarone in the setting of ACS is limited, and the drug is not recommended for thus indication.111
Finally, patients with AF and moderate-to-severe thromboembolic risk (CHA2DS2-VASc score ≥2) should be adequately treated with oral anticoagulants (either vitamin K antagonists or new oral anticoagulants) to reduce the risk of stroke or systemic embolisms (see below).
Recommendations for the management of atrial fibrillation in acute coronary syndrome
– For patients with acute coronary syndrome and pre-existing or newly developed atrial fibrillation (AF), rate control using beta-blockers or possibly calcium antagonists is recommended, whereas in patients with severe LV dysfunction using amiodarone and/or digitalis is recommended.
– Urgent direct current cardioversion is required if AF is accompanied by hemodynamic instability.
– For restoration of sinus rhythm in addition to electrical cardioversion amiodarone can be considered. Other antiarrhythmic drugs might be harmful in the setting of acute myocardial infarction.
– Adequate anticoagulation according to the individual risk of stroke and embolism is recommended, usually requiring a period of combination therapy of antiplatelet agents and anticoagulants.
Risk assessment for thromboembolic events, bleeding, and choice of antithrombotic therapy in patients with atrial fibrillation and acute coronary syndrome
Patients with ACS and permanent, paroxysmal or persistent non valvular AF are a special subgroup with an increased risk for ischaemic and embolic events, as well as bleeding complications. Since these events are closely related to clinical outcomes including mortality, decision making in the individual patient should be made by taking into account the risk for thromboembolic and bleeding hazards alike.
STROKE RISK STRATIFICATION
Based on the recent ESC guidelines stroke risk stratification should be made by the CHA2DS2-VASc score, which means that all patients with ACS will have a score of at least 1 and will therefore be candidates for oral anticoagulation.112-114 Patients with STEMI usually are treated with primary PCI and stenting in over 90% of cases, while PCI will be performed in about 50-60% of patients presenting with non-ST elevation ACS. Both groups of patients have an indication for dual antiplatelet therapy (DAPT). Hence, ‘triple’ therapy (DAPT and oral anticoagulation) for a defined period after the event is usually required.7,8 One controlled trial suggested that therapy with clopidogrel and an oral anticoagulant could be slightly safer than ‘triple therapy’,115 but more data are needed to confirm this.
BLEEDING RISK STRATIFICATION
Patients with an increased thromboembolic risk usually have clinical characteristics that are also associated with increase bleeding tendency, i.e. advanced age, female gender, renal dysfunction, femoral access, and history of prior bleeding hazards, especially of peptic ulcer. Accordingly, the use of specific risk scores (HAS-BLED score) to stratify for bleeding tendency in patients with AF116 seems practicable. In AF patients with and without anticoagulation therapy, it has higher accuracy in prediction of bleeding events and easier to use as compared with other scores.117,118 In patients with ACS, receiving triple antithrombotic therapy HAS-BLED score was found to have diagnostic value in prediction of bleeding.119 HAS-BLED score is currently recommended for risk stratification of bleeding in patients with AF and ACS.112,116,120,121
CHOICE OF ANTITHROMBOTIC THERAPY BASED ON THROMBOSIS AND BLEEDING RISKS
When AF affords anticoagulation in addition to DAPT, ‘triple’ antithrombotic therapy [DAPT plus an anticoagulant, usually a vitamin K antagonist (VKA) with an INR goal of 2.0-2.5] is recommended for the shortest time necessary,122 which is usually 1 month after bare metal stents and 3(-6) months after drug-eluting stent in stable/ elective patients as well as 6 months after ACS independent of the stent type and treatment strategy used, followed by one antiplatelet agent (clopidogrel or aspirin) plus an anticoagulant (‘dual’ therapy) for up to 12 months, and then by anticoagulant monotherapy lifelong.122 VKAs were shown to be at least as effective as aspirin in secondary prevention after acute MI.123 Ongoing research and expert-based position papers might widen the indication for non-VKA oral anticoagulants (NOACs) as replacement for VKAs in this clinical setting in the near future.124
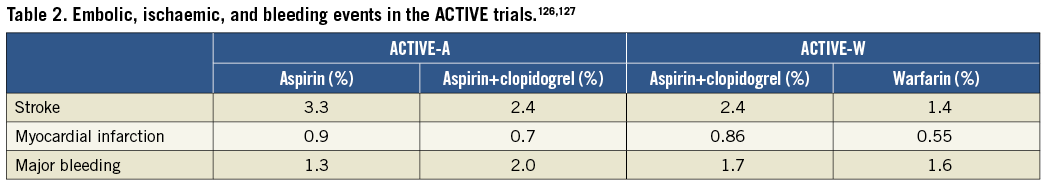
Against the existing guidelines, in clinical practice ‘triple’ therapy is less often used than recommended.125 In weighting the risk of embolic stroke and bleeding, some extrapolations from trials comparing antiplatelet therapies and anticoagulation have been included in clinical decision making. In the ACTIVE-A trial,126 DAPT with aspirin and clopidogrel has been more effective than aspirin alone in preventing stroke and systemic embolism in patients with AF. However, DAPT was inferior to warfarin in the ACTIVE-W study.127 Table 2 summarizes the embolic, ischaemic and bleeding events in the ACTIVE-trials.
From these data and the relatively low stroke rate in the first 3 months after ACS, it seems reasonable to recommend DAPT alone or VKA plus clopidogrel for 12 months for stable/elective patients with non-valvular AF with a CHA2DS2-VASc score of 1 when the bleeding risk is high.120 In patients with non-valvular AF plus ACS, independent of the stent type and treatment strategy used, ‘triple’ therapy for 4 weeks, followed by ‘dual’ therapy for 12 months should be used and in selected cases with low risk of stent thrombosis/ischaemic events ‘dual’ therapy alone may be considered when the CHA2DS2-VASc score is 1 and the bleeding risk is high.120 In all instances, this therapy might be followed by oral anticoagulation alone. However, in patients with a higher CHA2DS2-VASc score ‘triple’ therapy, followed by ‘dual’ therapy and finally oral anticoagulation alone should be considered as indicated above.
There exist two subgroups of patients with stent implantation and/ or ACS and AF, (i) the subgroup of patients with a history of AF already under oral anticoagulation, and (ii) a subgroup of patients with AF occurring under chronic DAPT. While recent recommendations allow the further use of NOACs in a reduced dosage in case patients were already pre-treated with a NOAC, little is known about the treatment strategy in the latter group and the updated position paper, a joint effort of the Working Group on Thrombosis, as well as EHRA, EAPCI, and ACCA, are non-specific by offering both, a start with VKAs or NOACs.120
Recommendations for risk assessment for thromboembolic events, bleeding and choice of antithrombotic therapy in patients with atrial fibrillation and acute coronary syndrome
– In patients with acute coronary syndrome and atrial fibrillation, prevention of thromboembolic events should be based on individualized risk stratification of thromboembolic events (risk of stroke-CHA2DS2-VASc score) to define the need for anticoagulation, risk stratification of bleeding (HAS-BLED score) to define the level of anticoagulation or choice of non-vitamin K antagonist oral anticoagulant strategy, and measures to minimize bleeding complications (stent choice, radial approach, and consequent short and long-term dual antiplatelet therapy).120
New bundle branch block and atrioventricular conduction disorders as complication of myocardial infarction
Atrioventricular conduction disturbances are well-known complications of acute MI.128,129 During the first few hours of myocardial ischaemia, they may be related to an autonomic imbalance with a vagal hyperactivity leading to a transient slowing of AV conduction. Myocardial ischaemia and necrosis may induce transient dysfunction or irreversible damage of the AV conduction system that may lead to the development of a new bundle branch block (BBB) or worsen a symptomatic high degree AV block necessitating temporary or permanent cardiac pacing.
In order to fully understand the relationship between myocardial ischaemia-infarction and the occurrence of new AV conduction disturbances, it is important to review the vascular supply of the different parts of the conduction system. The AV node and also the His bundle are supplied by the AV nodal artery that takes origin from the RCA in a 90% of the cases and from the left circumflex artery in 10% of the patients. A post mortem study has shown that proximal left anterior descending coronary artery (LAD) septal perforators perfuse the right bundle branch and the anterior fascicle of the left bundle branch in 90% of cases, whereas the posterior fascicle of the left BBB is perfused by the conus branch of the RCA in the majority of the cases.130 There is dual blood supply to each of the fascicles in half of the patients.123 An occlusion of the LAD therefore will induce a right BBB or an anterior left fascicular block. The development of a new left BBB will occur only in the presence of a proximal occlusion of both the RCA and the LAD.130
A second or third degree AV block in patients with an acute inferior wall MI is almost always (90% of the patients) located above the His bundle. Most often, this only results in a moderate bradycardia with a junctional escape rhythm with narrow QRS complexes. This conduction disorder most frequently is transient and is associated with a low mortality risk.
In patients with an anterior wall MI, a high degree AV block is most often located below the AV node. Total AV block generally occurs abruptly during the first 24 h after MI and is frequently preceded by the development of a new right BBB with the right or left axis deviation and QR pattern in lead V1. Most often, it is associated with an extensive myocardial necrosis of the septum and anterior wall in the presence of severe multivessel disease involving both the LAD and the RCA or a dominant left circumflex artery. Usually it causes catastrophic hemodynamic problems frequently leading to lethal pump failure.
Patients with a BBB have more comorbidities and are less likely to receive timely reperfusion therapy.131 It remains uncertain if the presence of a BBB at presentation has a prognostic importance. After adjustment for confounding factors, the presence of a BBB was no longer associated with an increased mortality risk. However, patients who develop a new left BBB within 60 min after admission have a three times higher 30-day mortality.132
Recommendations for management of new bundle branch block and atrioventricular conduction disorders in acute coronary syndrome
– Prompt opening of the infarct vessel is often sufficient to reverse new-onset ischaemic conduction disturbances. This is especially true for atrioventricular (AV) block in the setting of inferior infarctions.
– Temporary pacing is indicated for symptomatic life-threatening bradycardia not resolving after successful reperfusion and after medical treatment in the presence of high-degree AV block and intraventricular conduction defects.
– Permanent pacing is considered for disturbances that persist beyond the acute phase after the myocardial infarction.
Temporary pacing in intensive cardiac care unit in patients presenting with acute coronary syndrome: indications and techniques
TEMPORARY PACING IN CARDIAC INTENSIVE CARE UNIT
Temporary endocardial pacing has been used since the early 1960s to maintain cardiac output during episodes of extreme bradycardia, AV block, and asystole. Before the advent of cardiac pacemakers (PMs), the combination of acute MI and complete AV block was usually fatal, but now pacing electrodes can be safely placed percutaneously into the right ventricle under local anaesthesia. Prognosis is influenced not only by complications of the procedure, but also by the underlying myocardial damage, which originally lead to the conduction defect. In patients, who have not suffered an acute MI and are admitted to cardiac intensive care unit, temporary pacing may be required for treatment of a systole or bradycardia due to primitive cardiac conduction diseases, drug toxicity, electrolyte disturbances, or surgery.133
TECHNIQUES FOR TEMPORARY PACING
Endocardial temporary pacing leads are introduced via a central vein: right interior jugular, right subclavian vein or femoral veins. Pacing wires are commonly 5 Fr or 6 Fr. Under fluoroscopy, the lead is advanced into the right atrium and then, crossing the tricuspid valve, placed at the right ventricle apex. A check for positional stability, asking the patient to take some deep breaths or cough forcefully and watch for failure of capture, is suggested. A chest X-ray to confirm satisfactory positioning of the wire and to exclude a pneumothorax, is recommended as well.
Following cardiac surgery, patients may have temporary epicardial electrodes in case of postoperative bradyarrhythmia. These are used in the same way as transvenous pacing leads, but the threshold may be higher.
In emergency situations, transthoracic pacing is a better alternative, although it is not a substitute for temporary transvenous PM, and represents only a bridge to maintain life.
COMPLICATIONS
A temporary PM is a foreign body that may remain in the circulation for days and has a high propensity for infections, thus requiring surgical asepsis and antibiotic prophylaxis.134,135
Moreover, in case of a femoral approach for temporary pacing, restricted patient mobility may be cause of asymptomatic deep vein thrombosis, therefore antithrombotic prophylaxis as well is recommended.
The main frightening complication of temporary pacing in an ACS setting is the cardiac perforation causing cardiac tamponade.
The incidence of complications and malfunctions may be significant, occurring within 24 h in about 50% of patients and within 48 h in 86% of patients. Failure to capture or sense, VT during catheter insertion, fever and phlebitis are the most common complications. Other possible, more rare ones include phrenic capture, vascular complications for femoral approach (hematoma, pseudoaneurysm, arteriovenous fistula), hemothorax, and pneumothorax for subclavian and jugular accesses, cardiac perforation and tamponade. Sepsis, phlebitis, and pulmonary embolus are more common with temporary PMs in place for 72 h or longer.136
In many patients, particularly after acute MI, placing a pacing lead within the right ventricle will promote ventricular ectopic activity and occasionally prolonged VA.134 These will usually resolve once manipulation of the lead has ceased but will occasionally require removal of the lead or repositioning.137
An eventual cardiac perforation is usually manifest by raised pacing thresholds and occasionally by pericarditic pain and a pericardial friction rub. At worst, this will result in cardiac tamponade and will require appropriate urgent treatment. The increased risk of cardiac perforation and tamponade may be related to several factors such as
(1) the emergency setting;
(2) not-specialist doctors inserting the wire;
(3) higher stiffness of the leads;
(4)concomitant use of potent antithrombotics (GP IIb/IIIa inhibitors);
(5) inferior MI (with frail wall).
These and other considerations led to the drafting of new detailed guidelines by ESC and EHRA.105
Recommendations for temporary pacing in intensive cardiac care unit in patients presenting with acute coronary syndrome: indications and techniques
– Temporary transvenous pacing should not be used routinely and only as a last resort when positive chronotropic drugs (e.g. isoproterenol, atropine, etc.) are insufficient or contraindicated.
– Temporary transvenous pacing should be limited to cases of (i) high-degree atrioventricular block without adequate escape rhythm; (ii) life-threatening bradyarrhythmias, such as those that occur during interventional procedures (e.g. during percutaneous coronary intervention) or, rarely, in acute settings such as acute myocardial infarction, drug toxicity, electrolyte disturbances, or concomitant systemic infection.
– If the indications for permanent pacing are established, every effort should be made to implant a permanent pacemaker as soon as possible.
– An external stimulator (transcutaneous) does not provide reliable ventricular stimulation and therefore should only be used, under strict haemodynamic and electrocardiographic monitoring, when no other option is available. As soon as possible, an alternative action should be undertaken (administration of chronotropic drugs or temporary or permanent pacing).
Electrical cardioversion for arrhythmias in acute coronary syndrome patients with implanted rhythm devices
The different techniques for electrical CV depend on the various types and positioning of paddles, energy strategies and waveforms used. When performed in patients with an implanted PM and ICD systems, the choice between the different techniques can affect the outcome and safety of a CV.
When using biphasic defibrillators, self-adhesive defibrillation pads are safe and effective and an acceptable alternative to standard defibrillation paddles for both defibrillation and CV. The majority of studies comparing paddle size orientations and positioning (anteriorapex, anterior-posterior, anterior-left infrascapular, anterior-right infrascapular) have shown equal effectiveness in defibrillation (for VAs) or elective AF CV success, although an anterior-lateral electrode position was reported to increase efficacy and require fewer shocks for common atrial flutter.138 In recent resuscitation guidelines, an anterior-posterior position is generally accepted as an alternative position to an anterior-lateral position.139
The numerous case reports on device and lead failure following external CV in patients with implanted PM systems, has led to certain precautions including paddle positions to increase the safety of the procedure.
The risk of damage to the device is minimized by diodes that shunt current away from device and may be further reduced by keeping maximal distance between shock electrodes and the device. Leads may not be protected by these measures and current density may increase at the lead tip, particularly with unipolar leads, leading to myocardial damage at the electrode-endocardial surface. Such damage may result in local myocardial oedema with a transient increase of pacing threshold and fibrosis with permanent progressive increased pacing threshold and a deterioration of sensing function. These observations thus further argue for an anterior-posterior position for CV and also for defibrillation in patients with devices.
Very few studies have analysed the safety of external CV in patients with implanted PM systems.140 Transient loss of capture (up to 30 min) occurred in 50% of patients, a six-fold increase of ventricular pacing thresholds, sensing failure in 41% of patients, and three cases of PM malfunction were reported in a study evaluating patients with PM devices implanted in the right pectoral region and with unipolar electrodes.141 It was concluded that CV represents a serious hazard to patients with an implanted PM. In that study, however, only monophasic shocks were used and placed in an anterior-lateral orientation, which may create an electrical field in the same direction as the ventricular lead. An anterior-posterior positioning of CV electrodes is superior as it prevents this ‘antenna-like effect’ of the ventricular lead and result in lower energy requirements for termination of AF.141 Since biphasic shocks are superior to monophasic shocks for CV of AF142 and in terminating VF, all new defibrillators deliver shocks using biphasic waveforms. Mono- and biphasic shock waveforms for external CV were recently compared with regard to safety and efficacy in a prospective study of patients with implanted devices.143 Lower energy levels and at least >8 cm distance to the implanted device were adopted to minimize risk for damage to the devices and leads. Systems were tested immediately before and after CV, and 1 h and 1 week later with respect to device and lead integrity. Pacing impedances were reduced immediately after CV and returned to baseline values within 1 week. Ventricular sensing was reduced immediately after CV. There was no device or lead dysfunction in any patient. Cardioversion was successful in 95% of patients. The lower cumulative energy requirement for biphasic as compared with monophasic shocks indicated a theoretical advantage for biphasic shocks.
Electrical CV can thus be safely and effectively performed in patients with implanted rhythm devices, if the precautions outlined are considered. These recommendations also apply to emergency situations of VA in patients with implanted devices.
Recommended external electrical cardioversion technique in patients with implanted rhythm devices
– The anterior-posterior paddle/pad position on the chest is recommended
– The placement of paddles/pads should not delay defibrillation
– The paddle/pad should be placed on the chest wall ideally at least 8 cm from the generator position
– Biphasic shocks are preferred for electrical cardioversion
– Check for changes in pacing or sensing parameters 1 h after cardioversion
Conclusion
This document summarizes the current position, contemporary approaches, and offers recommendations on how to identify ACS patients at risk for arrhythmias; manage tachyarrhythmias and bradyarrhythmias using pharmacological and non-pharmacological, device- and catheter-based approaches including electrical CV, implantation of temporary PMs, programming of ICD, catheter ablation; and implement clinical and referral strategies. These recommendations are provided for acute care and management of VA, AF, bradyarrhythmias, and prevention of stroke and embolism in patients with ACS, and arrhythmias developing during coronary interventions, in patients with implanted devices and cardiogenic shock. Management of intractable arrhythmias requires the teambased approach including specialists in acute cardiac care, interventional cardiology, and electrophysiology.
Further supportive to the current knowledge evidence on the specific issues of arrhythmias management in the setting of ACS and answers to the gaps in knowledge emphasized in the current document should be pursued in future studies.
Supplementary material
Supplementary material is available at EuroIntervention online.
Acknowledgements
EHRA Scientific Documents Committee, Prof. Gregory YH Lip (EHRA Scientific Documents Committee Chair), Prof. Bulent Gorenek (EHRA Scientific Documents Committee Co-Chair), Prof. Christian Sticherling, Prof. Laurent Fauchier, Prof. Hein Heidbuchel, Dr Angel Moya Mitjans, Prof. Marc AVos, Dr Michele Brignole, Prof. Gheorghe-Andrei Dan, Dr Michele Gulizia, Dr Francisco Marin, Prof. Giuseppe Boriani, Dr Deirdre Lane, and Dr Irene Savelieva.
Conflict of interest statement
Detailed conflict of interest statements are available as supplementary material online.
Conflict of interest
EHRA-ACCA-EAPCI POSITION PAPER ON CARDIAC ARRHYTHMIAS IN ACS - REVIEWERS - 2014
EXPERT: Boriani Giuseppe
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Boston Scientific: Pacemaker, cardioverter defibrillators (2013)
– Medtronic: Pacemaker, cardioverter defibrillators (2013)
EXPERT: Fauchier Laurent
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Boehringer-Ingelheim: antithrombotic therapy (2013)
– Daiichi Sankyo: antithrombotic therapy (2013)
– Pfizer: antithrombotic therapy (2013)
– Bayer Healthcare: antithrombotic therapy (2013)
– Bristol Myers Squibb: antithrombotic therapy (2013)
– Sanofi Aventis: arrhythmias (2013)
– Boston Scientific: Cardiac Rhythm Management (2013)
– Medtronic: Cardiac Rhythm Management (2013)
– Novartis: Heart Failure (2013)
EXPERT: Lane Deirdre
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Bristol Myers Squibb/Pfizer: Atrial fibrillation (2013)
D. Research funding (departmental or institutional).– Boehringer-Ingelheim: Atrial fibrillation (2013)
– Bayer Healthcare: Atrial fibrillation (2013)
EXPERT: Lettino Maddalena
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Boehringer-Ingelheim: Anticoagulants (2013)
– The Medicines Company: Anticoagulants (2013)
– Daiichi Sankyo: Antithrombotic agents (2013)
– Eli Lilly: Antithrombotic agents (2013)
– Sanofi Aventis: Antithrombotic agents (2013)
– Bayer Healthcare: Antithrombotic agents, anticoagulants (2013)
– Bristol Myers Squibb: Antithrombotic agents, anticoagulants (2013)
– Astra Zeneca: Antithrombotic agents, anticoagulants, statins (2013)
– Merck Sharp & Dohme: Statins, Ezetimibe (2013)
– Pfizer: Statins, novel oral anticoagulants (2013)
EXPERT: Mehilli Julinda
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Roche Diagnostics: Antithrombotic drugs (2013)
– Lilly/Daiichi Sankyo: Antithrombotic drugs (2013)
– Biotronik: PCI (2013)
– Terumo Inc: PCI (2013)
– Abbott Vascular: PCI (2013)
EXPERT: Potpara Tatjana
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Bayer: stroke prevention in atrial fibrillation (2013)
– Boehringer-Ingelheim: stroke prevention in atrial fibrillation (2013)
– Pfizer: stroke prevention in atrial fibrillation (2013)
EXPERT: Roffi Marco
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Daiichi Sankyo: antiplatelet therapy (2013)
– Lilly: antiplatelet therapy (2013)
– Astra Zeneca: antipletelet therapy (2013)
D. Research funding (departmental or institutional).– Biosensors: devices (2013)
– Boston Scientific: devices (2013)
– Medtronic: devices (2013)
– Biotronik: devices (2013)
– Abbott Vascular: devices (2013)
EXPERT: Schiele Francois
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Astra Zeneca: ACS (2013)
– Daiichi Sankyo: ACS (2013)
– Eli Lilly: ACS (2013)
– Sanofi Aventis: ACS (2013)
– Medicines Company: ACS (2013)
– Abbott Vascular: angioplasty (2013)
– Boehringer-Ingelheim: anticoagulant (2013)
– Bayer: anticoagulation (2013)
– Boehringer-Ingelheim: anticoagulation (2013)
– Servier: heart failure (2013)
– Amgen Inc: hypercholesterolemia (2013)
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Astra Zeneca: ACS (2013)
– Daiichi Sankyo: ACS (2013)
– Sanofi Aventis: ACS (2013)
– Merck Sharp & Dohme: Cholesterol lowering (2013)
– Servier: heart Failure (2013)
EXPERT: Sinnaeve Peter R
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– None
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Astra Zeneca: ACS (2013)
– Lilly: ACS (2013)
– Bayer: ACS & AF (2013)
– Boehringer-Ingelheim: ACS & AF (2013)
– GlaxoSmithKline: ACS & CAD (2013)
– Merck Sharp & Dohme: CAD & ACS (2013)
– Abbott Vascular: PCI (2013)
– Duke University: trials (2013)
– Sanofi Aventis: trials, consultancy (2013)
D. Research funding (departmental or institutional).– Astra Zeneca: basic science and epidemiology (2013)
EXPERT: Sticherling Christian
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Bard: Ablation therapy (2013)
– Bayer: Anticoagulants, atrial fibrillation (2013)
– Bristol Myers Squibb: Anticoagulants, atrial fibrillation (2013)
– Medtronic: Defibrillators, Pacemaker (2013)
– Sorin Group: Defibrillators, Pacemaker (2013)
– Biotronik: Defibrillators, Pacemaker, (2013)
D. Research funding (departmental or institutional).– Biosense Webster: Atrial fibrillation (2013)
– Biotronik: CRT (2013)
EXPERT: Widimsky Petr
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Servier: Antiischemic agents (2013)
– Astra Zeneca: Antithrombotic agents (2013)
– Bayer: Antithrombotic agents (2013)
– Boehringer-Ingelheim: Antithrombotic agents (2013)
– Daiichi Sankyo: Antithrombotic agents (2013)
– Eli Lilly: Antithrombotic agents (2013)
– Sanofi Aventis: Antithrombotic agents (2013)
– Abbott: Stents (2013)
– Medtronic: Stents (2013)
This list represents the relevant relationships of the above experts with Industries and other entities that were reported to us at the time of publication of the Guidelines.
EHRA-ACCA-EAPCI POSITION PAPER ON CARDIAC ARRHYTHMIAS IN ACS - AUTHORS - 2013
EXPERT: Blomstrom-Lundqvist Carina
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Sanofi Aventis: AF
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Medtronic: AF
– Biotronik: Arrhythmia
D. Research funding (departmental or institutional).
– Medtronic: AF
– Biotronik: Arrhythmias
EXPERT: Brugada Terradellas Josep
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Boston Scientific: devices
– Sorin Group: devices
– St Jude Medical: devices
– Biotronik: devices
EXPERT: Camm John
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Cameron Health: All
– ChanRx: antiarhhythmic drug
– Johnson & Johnson: Apixaban
– Forest Pharmaceuticals: Azimilide
– Wiley Blackwell: Clinical Cardiology
– Boehringer-Ingelheim: Dabigatran
– BMS: DSMB
– Biotronik: DSMB. Ablation
– Merck Sharp & Dohme: DSMB. Ablation
– AGA: DSMB. several
– Novartis: DSMB. several
– Infobionics: ECG monitoring
– Oxford University Press: Europace and ESC textbook
– GlaxoSmithKline: General Advice
– Servier: Multiple products
– Sanofi Aventis: Multiple products
– Menarini: Ranolazine
– Gilead: Ranolazine
– Bayer: Rivaroxaban
– Medtronic: Subcutaneous monitoring
D. Research funding (departmental or institutional).
– Servier: Antiarrhythmic drug
– BMS/Pfizer: Apixaban
– Daiichi Sankyo: Edoxaban
– Sanofi Aventis: Edoxaban
– Richmond Pharmacology: Many phase 1 NCEs
EXPERT: Gorenek Bulent
TYPE OF RELATIONSHIP WITH INDUSTRY:
None
EXPERT: Hindricks Gerhard
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Stereotaxis: catheter ablation
– Biosense Webster: catheter ablation
– Medtronic: Pacemaker
– St Jude Medical: Pacemaker, catheter ablation
– Biotronik: Pacemaker, catheter ablation
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Stereotaxis: catheter ablation
– Biosense Webster: catheter ablation
– Medtronic: Pacemaker
– St Jude Medical: Pacemaker, catheter ablation
– Biotronik: Pacemaker, catheter ablation
D. Research funding (departmental or institutional).
– St Jude Medical: catheter ablation, pacemaker
– Biotronik: catheter ablation, pacemaker
EXPERT: Huber Kurt
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Pfizer: atorvastatin, edoxaban
– Medicines Company: bivalirudin; cangrelor
– BRAHMS GmbH: copeptin assay
– Boehringer-Ingelheim: dabigatran
– Eli Lilly Lilly/Daiichi Sankyo - speakers fees; advisory board fees (prasugrel): prasugrel; abciximab
– Bayer: rivaroxaban
– Astra Zeneca: ticagrelor; rosuvastatin
EXPERT: Kirchhof Paulus
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– BMS: cardiovascular
– Boehringer-Ingelheim: cardiovascular
– Daiichi Sankyo: cardiovascular
– Medtronic: cardiovascular
– Pfizer: cardiovascular
– St Jude Medical: cardiovascular
– Sanofi Aventis: cardiovascular
– Meda pharma: cardiovascular
– Merck Sharp & Dohme: cardiovascular
– Otsuka Pharmaceuticals Development and Commercialization (consultancy): cardiovascular
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Boehringer-Ingelheim: cardiovascular
– Bayer Healthcare: cardiovascular
– Portola Pharmaceuticals: cardiovascular
– BMS / Pfizer alliance: cardiovascular
D. Research funding (departmental or institutional).
– St Jude Medical: cardiovascular
– Sanofi Aventis: cardiovascular
– Meda pharma: cardiovascular
EXPERT: Kuck Karl-Heinz
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Edwards Lifesciences: Speaker Fees, Honorary, Consultancy
– Medtronic: Speaker Fees, Honorary, Consultancy
– Abbott Vascular: Speaker Fees, Honorary, Consultancy
– Cordis: Speaker Fees, Honorary, Consultancy
– Biosense Webster: Speaker Fees, Honorary, Consultancy
– St. Jude: Speaker Fees, Honorary, Consultancy
– CCM- Impulse Dynamics: Speaker Fees, Honorary, Consultancy
EXPERT: Kudaiberdieva Gulmira
TYPE OF RELATIONSHIP WITH INDUSTRY:
None
EXPERT: Raviele Antonio
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Biosense Webster: CARTO
– Sanofi Aventis: Dronedarone
– St Jude Medical: NaviX
– Bayer: Rivaroxaban
– Merck Sharp & Dohme: Vernakalant
EXPERT: Santini Massimo
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Medtronic: RESEARCH IN PACING AND ELECTROPHYSIOLOGY
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Medtronic: RESEARCH IN PACING AND ELECTROPHYSIOLOGY
EXPERT: Valgimigli Marco
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Terumo Inc: Interventional cardiology
– Accumetrics: Platlet Function Assay
– Medtronic: stent
– Abbott Laboratories: stent
– Abbott Vascular: stent
– Cordis: stent
– CID: stent
– Astra Zeneca: ticagrelor
– Chiesi Pharma: tirofiban
– Iroko Cardio: Tirofiban
EXPERT: Vos Marc
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– None
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Medtronic: CRT
– Gilead: Na late blockers
D. Research funding (departmental or institutional).
– Medtronic: CRT
– Gilead: Na late blocker
EXPERT: Vrints Christian Jm
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– None
D. Research funding (departmental or institutional).
– Bracco Pharmaceutical: contrast dye
– Medtronic: Interventional cardiology devices
EXPERT: Zeymer Uwe
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Medicines Company: Anticthrombotic
– Novartis: Antihypertensives
– Astra Zeneca: Antithrombotic
– Daiichi Sankyo: Antithrombotic
– Sanofi Aventis: Antithrombotic
– Lilly: Antithrombotic
– Bayer Healthcare: Antithrombotic
– B.Braun: Drug eluting Balloon
– Medtronic: Renal Denervation
D. Research funding (departmental or institutional).
– Novartis: Antihypertensives
– Daiichi Sankyo: Antithrombotic
– Sanofi Aventis: Antithrombotic
– Lilly: Antithrombotic
EXPERT: Lin Tina
TYPE OF RELATIONSHIP WITH INDUSTRY:
None
EXPERT: Tilz Roland
TYPE OF RELATIONSHIP WITH INDUSTRY:
A. Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Bayer: Oral anticoagulation
– Sanofi Aventis: Oral anticoagulation
– Bristol Myers Squibb: Oral anticoagulation
– Pfizer: Speakers fee
– Biotronik: Speakers fee
– Hansen Medical: Speakers fee
– Biosense Webster: Speakers fees, Honoraria
B. Payment to your Institution: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc.
– Biosense Webster: AF ablation course
D. Research funding (departmental or institutional).
– St Jude Medical: Man and Machine Trial
– Hansen Medical: Man and Machine Trial

