The editorial refers to “Drug-eluting stent implantation for chronic total occlusions: comparison between the sirolimus- and paclitaxel-eluting stent” by Hoye A et al., published in this issue of EuroIntervention.
During the last few years, the introduction of new technologies such as directable dissecting and ablative devices and CTO-dedicated guidewires, coupled with improvements in operator experience, have significantly increased the success rate in crossing CTO lesions. However, despite the routine and systematic use of bare metal stents, the long term patency rates have been disappointing. Several randomized trials have compared balloon angioplasty with stent implantation in patients with CTO1-9. Collectively, a recent meta-analysis has been shown that the need for repeat revascularisation was decreased from 32.06% in the balloon arm to 16.98% in the group allocated to stenting (OR 0.41, 95% CI [0.31,0.53], p <0.0001), with an overall MACE rate reduction from 35.4% to 23.2% (OR 0.49, 95% CI [0.36,0.68], p<0.0001). In addition, the restenosis and reocclusion rates were both decreased by stent, (60.9% to 41.1% [OR 0.36 95% CI 0.23,0.57]; 16% vs. 6.8%, [OR 0.36, 95% CI 0.22,0.59], respectively) (Agostoni et al. Am Heart J. In press).
Yet, the incidence of restenosis and the need for repeat revascularisation using bare metal stent (BMS) in this subset of patients remain higher than in non-occluded lesions10, perhaps due to a more negative vascular remodeling, greater mean stent length, calcification, and greater plaque mass of CTO lesions.
In two registries evaluating the effect of sirolimus-eluting stents and paclitaxel-eluting stents in CTO patients, the need for TVR rate at 6 months was 1.5% and 0.9%, respectively. (Alexander Abizaid and Chaim Lotan, presented at Transcatheter Cardiovascular Therapeutics, September 2004).
These results are clearly very encouraging. Nevertheless, a powered prospective, randomised trial to support this clinical practice has yet to be conducted. Therefore, a systematic review was done to better quantify the benefits of coronary stenting in CTO patients using drug-eluting stents (DES) and to provide meaningful insights into the separate clinical end points. Four studies have been published11-14 and one more was presented at TCT 2004 by Kim et al. Overall 874 patients were included, of which 340 were treated with DES. All the patients included had a native vessel occlusion older than 2 weeks. The median clinical and angiographic follow-up was 12 months (range 6-12 months) and 6 months (range 6-12 months), respectively. Death and myocardial infarction rates were not different in the two groups, death rate was 0.88% in DES vs. 0.94% in BMS (OR 0.91[0.21,3.98] p=0.9), and MI rate was 3.8% vs. 4.5% (OR 1.6[0.52,2.17], p=0.87). However, the probability of repeated revascularisation was reduced by 87% in DES (OR 0.13[0.06,0.25], p<0.0001). This resulted in an overall reduction in the rate of MACE from 33.5% to 9.4% (OR 0.19[0.09,0.39], p<0.0001) in favour of DES usage. All 5 studies had protocol mandated 6-months angiographic follow-up and the restenosis rate was significantly different, 5.98% in DES vs. 30.63% in BMS (OR 0.12[0.05-0.28], p<0.0001). Furthermore, MLD after DES was 0.93 mm larger than after BMS and late loss was strongly reduced by DES as compared to BMS (0.23 vs. 1.18 mm), p<0.0001. Subacute thrombosis (SAT) was documented in two patients, one occurred after sirolimus stent implantation11 and the other after BMS implantation14.
The study by Hoye et al. (in the current issue of EuroIntervention) provides an additional insight into the long term clinical follow-up after implantation of sirolimus, paclitaxel and BMS in CTO. As expected, the survival-free of target vessel revascularisation was significantly higher in the sirolimus-eluting stents (SES) and paclitaxel-eluting stents (PES) groups compared with the BMS group (97.4% and 96.4% versus 80.8% respectively, p=0.01). SAT was reported in only one patient who had a sirolimus stent implantation. Although this report has a potential selection bias due to the fact that the three groups are not concurrent, the results are in line with previous reports. In addition, the lack of systematic angiographic follow-up in the present report may possibly explain the differences in need for repeat revascularisation between the three groups.
Thus, when taken together current findings suggest, even if do not prove, that DES in this subset of patients is safe and effective. However, the cost-effectiveness of this practice remains unknown. The extra cost of DES might be offset by the lower restenosis rate and need for repeat revascularisation. These and other issues needs to be properly evaluated in properly-powered prospective randomized trials.
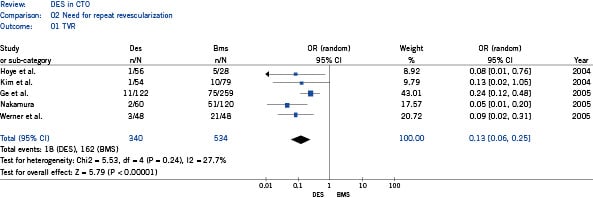
Figure 1. Comparison of the risk of need for repeat revascularization in patients treated with drug eluting stent versus bare metal stent in each study and in the overall population, showing odds ratio (OR) and 95% confidence intervals (CI).

