After the recent change in ownership, Twitter is turning into something else. I notice it in the content, my feed is full of unsolicited reading suggestions that sooner or later I will be able to disable. However, one thing that still works as before is the trending topic column, which is quite sensitive when it comes to highlighting “the things that everyone is talking about”. And here, real discoveries are often made.
For example, a few weeks ago I noticed the hashtag #ChatGPT everywhere and tried to understand more about it. ChatGPT is an intelligent bot, and although it takes a lot to be amazed in the age of Siri, Alexa and other kinds of voice assistants, this bot is smart. And when I say smart, I mean something wasn’t clear to me until I tried it myself with my fellows.
Basically, the bot can answer any question in great detail, and is very focused on generating texts. We asked it to generate a synopsis or even the text of a hypothetical scientific article, and the result was amazing... and disturbing. I first wondered if I would be able to distinguish between a scientific text generated by artificial intelligence or an autograph text, and the answer is no, especially if this technology improves further. Of course, the contents are more important than the form in the preliminary phases in which we think about the merit of an article, but it is a fact that this novelty could cause some problems in the medical publishing community.
Indeed, how much of that text is reworked by the bot, and how much is genuine plagiarism of other existing texts? What are the ethical boundaries of using a bot to generate a text? These are all questions that scientific journals will soon have to find an answer to, or maybe I’m overreacting to a dystopian scenario that is a figment of my imagination. We’ll see. In the meantime, let’s enjoy the articles in this issue of the journal, which are not written by ChatGPT but by a number of real esteemed and respectable authors.
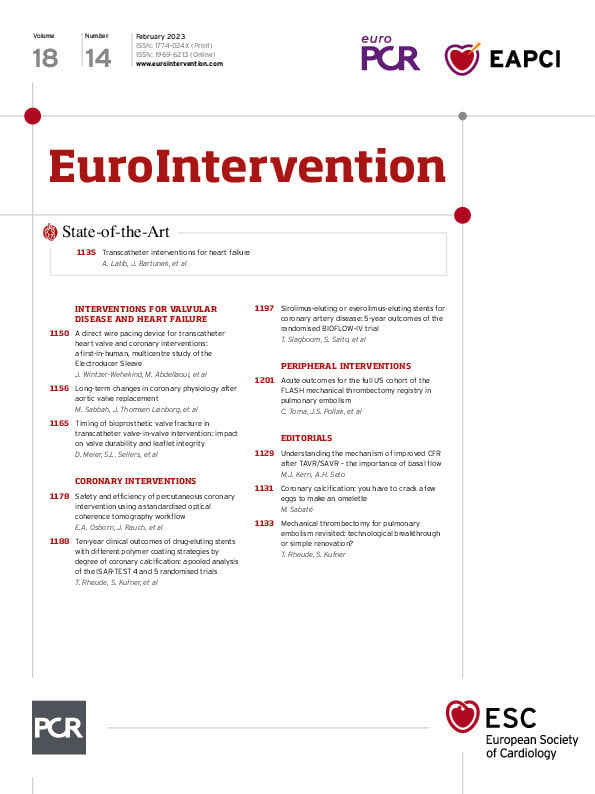
We open this issue with a state-of-the-art by Azeem Latib, Jozef Bartunek and colleagues who offer us a thorough examination of transcatheter interventions for heart failure. The last decade has seen an increase in non-valvular catheter-based therapies that complement existing guideline-directed medical therapies. These modalities address mechanistic pathophysiologic targets critical in the progression of heart failure including congestion, left ventricle remodelling and neurohumoral activation. Their review explores the physiology, rationale, and the current stages of clinical development of existing procedures and includes expert commentaries on implantable haemodynamic monitors, left atrial decompression, neuromodulation for management of heart failure, device-based therapy for cardiorenal syndrome and cardiac contractility modulation.
Also, in interventions for valvular disease and heart failure, Jérôme Wintzer-Wehekind, Mohamed Abdellaoui and colleagues report on the first-in-human use of the Electroducer Sleeve. This new purpose-built device provides direct wire pacing without the need for a temporary venous pacemaker. It was tested in 60 patients requiring either transcatheter aortic valve implantation (TAVI) or complex percutaneous coronary interventions (PCI) and was performed in procedures by either radial and femoral vein or artery access. The device proved to provide safe and effective unipolar pacing and was well tolerated. Of course, larger prospective studies are warranted.
Left ventricular hypertrophy and exhaustion of coronary flow reserve (CFR) are among the deleterious effects of long-term severe aortic stenosis. Muhammad Sabbah, Jacob Lønborg and colleagues investigate data from 34 aortic valve replacement patients and whether improvements in CFR in the left anterior descending artery are related to hyperaemic resting flow and minimal microvascular resistance as well as how changes in CFR affect left ventricular mass and stroke work. Their study demonstrates that increased CFR after valve replacement is not due to increased maximal hyperaemic flow or reductions in microvascular resistance from reduced left ventricular mass, but because resting flow and stroke work decrease in response to a reduction in myocardial demand. This article is accompanied by an editorial by Morton J. Kern and Arnold H. Seto.
Does the timing of bioprosthetic valve fracture – before or after valve-in-valve TAVI – impact the long-term durability of transcatheter heart valves? David Meier, Stephanie L. Sellers and colleagues present their bench study assessing this question, using small ACURATE neo or 23 mm SAPIEN 3 transcatheter heart valves, deployed in 21 mm Mitroflow valves. Through hydrodynamic testing, second harmonic generation, scanning electron microscopy and histological analysis, their findings suggest that bioprosthetic valve fracture performed after valve-in-valve seems to offer the largest haemodynamic benefit without any long-term trade-offs in terms of transcatheter heart valve performance or structural valve damage.
In coronary interventions, Eric A. Osborn, Judah Rauch and colleagues on behalf of the LightLab Initiative investigate whether a standardised optical coherence tomography (OCT) workflow impacts PCI safety and procedural efficiency. Their results show reductions in radiation dose, vessel preparation time, device utilisation, and unplanned vessel treatment relative to angiography-guided PCI. While procedure times using the OCT-guided workflow were slightly longer, there was no detectable difference in contrast use relative to angiography guidance alone.
Tobias Rheude, Sebastian Kufner and colleagues report on the 10-year outcomes by degree of coronary artery calcification after new-generation drug-eluting stent implantation with different polymer-coating strategies (polymer-free vs biodegradable-polymer vs permanent-polymer). In a pooled analysis of 4,953 of patients with both moderate-severe or severe coronary artery calcification, there was an incremental risk of adverse events according to the degree of calcification. The authors conclude that the effects are not influenced by the different polymer-coating strategies currently available. This article is accompanied by an editorial by Manel Sabaté.
Continuing with biodegradable vs permanent polymers stents, Ton Slagboom, Shigeru Saito and colleagues deliver the 5-year outcomes of the BIOFLOW-IV trial which compared the Orsiro biodegradable-polymer sirolimus-eluting stent with the XIENCE Prime/XIENCE Xpedition durable polymer everolimus-eluting stents. The results, including a 5-year target vessel failure rate of 12.3% for the biodegradable-polymer group and 10.8% for the permanent-polymer group, showed low event rates and the absence of late or very late definite or probable stent thrombosis, demonstrating safety and a sustained treatment effect at 5 years.
In peripheral interventions, Catalin Toma, Jeffrey S. Pollak and the FLASH investigators evaluate the safety and effectiveness of mechanical thrombectomy using the FlowTriever System for patients with intermediate- and high-risk pulmonary embolisms. Results from the FLASH registry, a multicentre, prospective registry with up to 1,000 patients treated with the FlowTriever System suggest that the safety profile of the FlowTriever System is robust, with low rates of major adverse events (1.8%) and all-cause mortality at 48-hour and 30-day follow-up (0.3% and 0.8%, respectively). Further studies are needed for longer-term follow-up. This article is accompanied by an editorial by Tobias Rheude.
And now let’s let the articles speak for themselves.