I am always a bit unsure when it comes to answering questions regarding whether the future of EuroIntervention should be digital or printed. Fortunately, on this specific question, it’s not up to me – that decision belongs to our Publisher.
In fact, after each EuroPCR (where course participants who are also PCR Companions receive a year of free subscription, did you know that?), many of us have been asked to choose whether we prefer a digital or printed version of EuroIntervention. My own answer has been "digital" for many years, because it seemed to me that this was the direction the world was going in, but then I discovered that there are still many readers who would choose the printed option, and I began to wonder why.
To begin with, based on the feedback we have received, some readers obviously find our printed version to be a nice and inviting product to browse through (and here I certainly am not congratulating myself or the Editorial Board, but the production team and graphics department).
During the Editorial Board meeting which took place at the recent EuroPCR, an intriguing strategic approach was proposed by one of our Section Editors – if we want to increase the international visibility of the Journal (for example, in the United States), we must be ready to send physical copies of the Journal directly where it would most likely be of interest and read – for instance, to interventional cardiology units.
I confess that I had never thought about anything like this. EuroIntervention in the break rooms found next to cath labs, placed on the table, available to all those who want to browse through it; where they can flip through the 100 or so pages to see if there is any news in the field of interventional cardiology and beyond of interest to them and their fellow interventionalists.
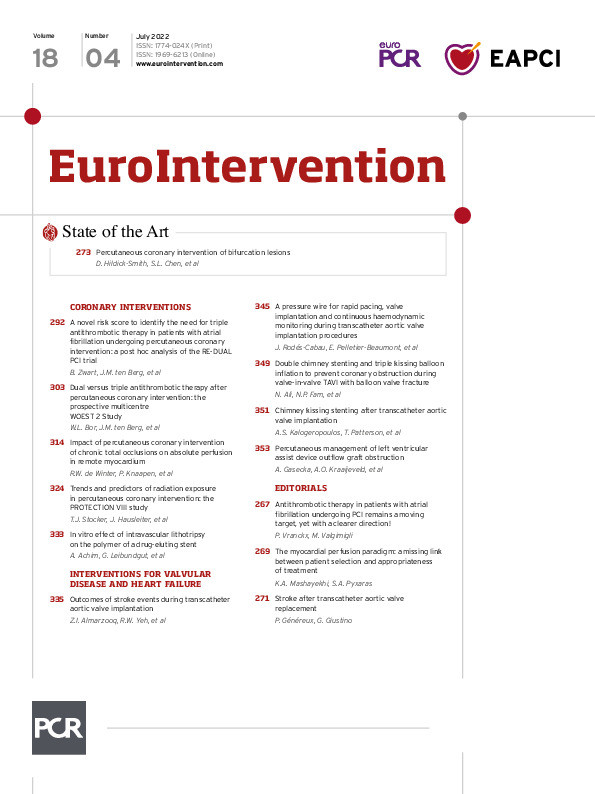
Perhaps this is just the type of news you’ll find in this issue now, so let me briefly introduce it.
We begin with a EuroIntervention state-of-the-art on the treatment of bifurcation coronary artery disease by percutaneous coronary intervention (PCI). Authors David Hildick-Smith, Shao-Liang Chen and colleagues lead us through this critical review of the different steps to consider when treating bifurcation lesions. From understanding anatomical and physiological factors, to the different stent techniques (from stepwise provisional stenting to 2-stent techniques), the authors discuss current evidence and experience, pointing out the approach best employed depending on the complexity of the intervention while underlining the importance of experience on the part of the operator as well as the operator’s commitment to a disciplined and complete approach.
Continuing with coronary interventions, Bastiaan Zwart, Jurriën Maria ten Berg and colleagues have developed a simplified thrombotic risk score to choose between the use of triple antithrombotic therapy or double antithrombotic therapy when treating atrial fibrillation patients. The authors performed a post hoc analysis of data from the RE-DUAL PCI trial, concluding through their scoring system that while triple antithrombotic therapy could be appropriate for a small group of patients, double antithrombotic therapy is the better choice for the majority of patients. This article is accompanied by an editorial by Pascal Vranckx and Marco Valgimigli.
Continuing with dual and triple antithrombotic therapy, Willem Lambertus Bor, Jurriën Maria ten Berg and colleagues considered the real-world data from the WOEST 2 registry comparing antithrombotic regimens and outcomes after PCI in patients who use oral anticoagulants. Though major adverse cardiac and cerebrovascular events were not significantly different between the two therapies, dual antithrombotic therapy was associated with a substantially lower risk of bleeding without a significant increase in ischaemic events.
What is the impact on the coronary physiology of remote myocardium when you revascularise chronic total coronary occlusions (CTO) using PCI? Ruben W. de Winter, Paul Knaapen and colleagues respond to this question by performing quantitative perfusion assessments using positron emission tomography and conclude that the beneficial effects of CTO PCI with its improvements in stress flow and coronary flow reserve in the CTO territory itself can also be seen to go beyond the treated myocardium, increasing perfusion in more remote territories as well. This article is accompanied by an editorial by Kambis A. Mashayekhi and Stylianos A. Pyxaras.
Radiation exposure remains a critical issue for all interventionalists and cath lab staff. In this next article, Thomas J. Stocker, Jörg Hausleiter and colleagues discuss the German PROTECTION VIII study which looked at variations in radiation exposure over a period of 10 years. Their study, which enrolled almost 4 million patients undergoing PCI, demonstrated that, while radiation doses have been significantly reduced, there remains a large variability between different centres. The challenge of keeping radiation doses as low as reasonably possible remains constant, and education, training, and the use of improved equipment and low-dose acquisition protocols need to be further implemented.
Now, we turn to valvular interventions. A small percentage of our patients undergoing transcatheter aortic valve implantation (TAVI) experience a procedure-related stroke whose consequence can be catastrophic. Zaid I. Almarzooq, Robert W. Yeh and colleagues studied cases of TAVI-related stroke between 2012 and 2017, highlighting this critically important and potentially preventable source of patient mortality and morbidity, as well as of the additional burden on the healthcare system. Accompanied by an editorial by Philippe Généreux and Gennaro Giustino, the authors urge an increased awareness and better understanding of what can be done to avoid these negative results.
Finally, authors Josep Rodés-Cabau, Emilie Pelletier-Beaumont and colleagues provide us with an intriguing look at the SavvyWire, a new pressure wire for use during TAVI procedures. This wire, whose ease of use can facilitate clinical decision-making during TAVI, is connected to the OptoMonitor which provides pressure signals and TAVI-specific metrics for continuous haemodynamic monitoring.
And now… let’s turn to the articles and see what they have to say for themselves.
Supplementary data
To read the full content of this article, please download the PDF.