I realised a few days ago that, since I became Editor of this Journal, I haven’t physically attended an international congress. We all know the reasons – the pandemic, the lockdown, complex travel restrictions. The last congress I physically attended was Ron Waksman’s CRT, in Washington DC, in February 2020. In those days at CRT there was talk of what was still an epidemic, and the few participants wearing masks were not taken seriously. Still, I remember that in one session the speaker before me fainted, struggling to finish his talk, as if for lack of breath. A few weeks later, on social media, he declared his suspicion of having contracted a mild form of COVID-19 during the event.
The world then quickly changed, and with it the world of scientific congresses. I could never have imagined how the pandemic was going to impact on my nascent relationship with EuroIntervention and the Journal in general. The reasons are easy to understand. Within a few weeks we had to convert all editorial activities into an online efficiency, automating many processes (not necessarily a disadvantage). At the same time, we at the Editorial Office found ourselves managing a quantity of articles that practically doubled compared to previous years (this too remains positive for me) – all those incredible months in which cardiologists around the world received fewer patients with heart attacks (the so-called “missing STEMIs”) and we Journals received more scientific articles. I’m not sure I’ve thanked enough all those in the EuroIntervention team who have ensured the quality of the Journal with competence and professionalism for so many years and what they managed to do in those months… Not the least of these was managing a new Editor with all his requests, among other things.
This Editorial Board was born in times of emergency and, since I began running it, I have never had the opportunity to meet participants at an international congress – participants who could tell me if they liked what we’re doing, or if we are all wrong. Sometimes I think I miss this direct feedback. Then I realise that, in retrospect, even this may not be a disadvantage, because it allowed us during those difficult, yet memorable months to focus solely on the final product that we try to achieve each month and which is gradually taking on the shape we had in mind from the very beginning.
For better or worse, the absence of positive or negative judgements has allowed us to work towards the evolution of our project, with the now imminent release of the impact factor to be our judge – a project that is made up of intermediate stages, such as this issue, whose contents I will now summarise.
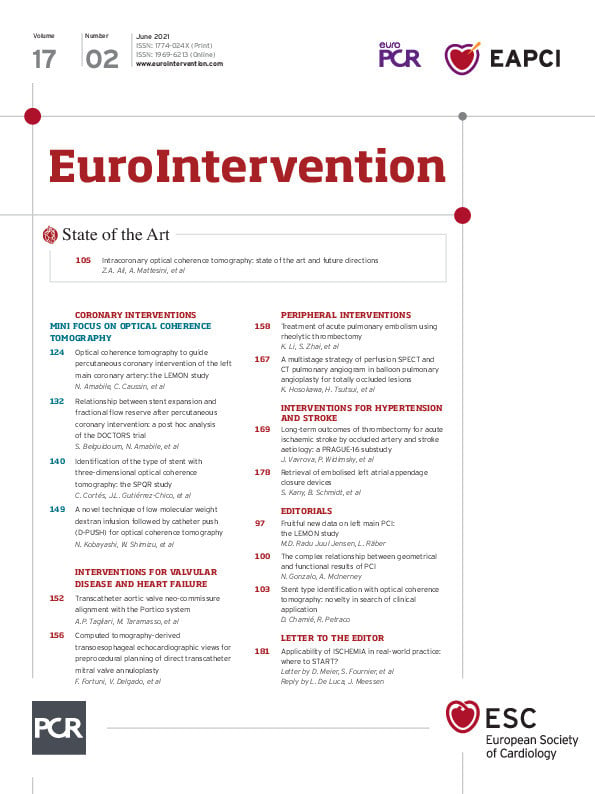
This issue’s mini focus is on intracoronary optical coherence tomography (OCT), beginning with a State of the Art by Ziad A. Ali, Alessio Mattesini and colleagues. Intracoronary OCT, with its high resolution and diagnostic capabilities, is increasingly used in percutaneous coronary interventions (PCI), yet its use still lags behind intravascular ultrasound in clinical practice. The authors, to encourage and facilitate the further adoption of this technique, provide the latest information concerning its execution and simplified image interpretation, as well as an algorithmic approach for the use of intracoronary OCT in PCI guidance. The usefulness of OCT in acute coronary syndromes is highlighted along with the latest clinical data, ongoing trials and future perspectives.
Our OCT mini focus continues with authors Nicolas Amabile, Christophe Caussin and colleagues reporting on the LEMON study which examined the feasibility and safety of using OCT instead of intravascular ultrasound in left main stem PCI guidance. While further research is still needed, this is an additional step in OCT acceptance. The article is accompanied by an editorial by Maria D. Radu Juul Jensen and Lorenz Räber.
In a substudy of the DOCTORS trial, Salim Belguidoum, Nicolas Amabile and colleagues look at stent expansion criteria and final PCI functional results in non-ST-elevation segment acute coronary syndrome patients who underwent OCT-guided PCI. With no observed relationship between optimal stent expansion and final post-PCI fractional flow reserve values, current geometric methods appear limited in assessing device deployment, and new strategies need to be elucidated to predict PCI success better. Nieves Gonzalo and Angela McInerney provide an editorial on this article.
Could OCT be a useful tool in identifying previously implanted but unknown stent types in cases of stent failure? In the next article in our mini focus, authors Carlos Cortés, Juan Luis Gutiérrez-Chico and colleagues use a specially developed protocol combining three-dimensional OCT, automatic strut detection and longitudinal views. This article is accompanied by an editorial by Daniel Chamié and Ricardo Petraco.
Our mini focus ends with an article on improving OCT image quality using a low molecular weight dextran infusion followed by catheter push in patients with kidney disease or unknown renal function, where large volumes of contrast media would be problematic. Nobuaki Kobayashi, Wataru Shimizu and colleagues show that this method can improve OCT imaging over conventional methods in exploring tight stenotic lesions, such as visualising the distal part of a lesion, thus ultimately aiding in PCI strategies.
With the steady extension of indications for transcatheter aortic valve implantations to younger populations, authors Ana Paula Tagliari, Maurizio Taramasso and colleagues look at the importance of neo-commissure alignment to avoid post-procedural complications or rapid transcatheter heart valve deterioration. Evaluating the Portico device alignment technique, they employed 3D-printed aorta models to validate proposed orientation steps for successful, reproducible deployment – steps which could be easily adapted to real-life scenarios.
In peripheral interventions, Kun Li, Shuiting Zhai and colleagues evaluate the AngioJet rheolytic thrombectomy system. Their research shows this approach to be feasible and safe, as well as reducing complications in the treatment of intermediate- and high-risk pulmonary embolisms when the system is used with local thrombolysis. With further trials, this could prove to be a first-line treatment option, which can also offer a fast clinical response in acute settings where the time needed for systemic thrombolysis is limited.
Catheter-based or mechanical thrombectomy has proven to be an effective treatment for treating patients with acute ischaemic strokes. In a PRAGUE-16 substudy, Jana Vavrova, Petr Widimsky and colleagues look at the important role stroke aetiology and the occlusion site play in clinical outcomes after interventions using either stentrievers or aspiration devices. Patients with occlusions of either an isolated middle cerebral artery or an isolated internal carotid artery, as well as those with tight stenosis or tandem occlusions, had significantly better clinical outcomes than patients with posterior circulation ischaemic strokes or anterior strokes caused by carotid artery terminus occlusions where the treatment technique needs to be further refined.
Finally, Shinwan Kany, Boris Schmidt and colleagues look at the retrieval of embolised left atrial appendage closure occluders, concluding that, while transcatheter retrieval from the left atrium or the aorta appears safe and feasible, for retrieval from the left ventricle patients should be referred for heart surgery.
We hope there is something for everyone in this issue, so now it is your turn to enter and take a look!
Supplementary data
To read the full content of this article, please download the PDF.