This month, there are so many topics to discuss that I hardly know where to begin. Yet, there is one subject that has taken precedence in recent times and concerns a changing of the guard among our Deputy Editors. The news has been known for a few months among those working within the PCR galaxy, but now that it has become public knowledge that Lars Søndergaard has accepted a new challenge in his prestigious career, becoming the Chief Medical Officer of a device company, we can discuss it openly. Lars’ new position, while an exciting opportunity for him, is obviously incompatible with serving the Journal, and so, by mutual agreement, we are ending his appointment.
First and foremost, I would like to express my deepest gratitude to Lars for his invaluable contributions to EuroIntervention as a Deputy Editor over the past years. His keen eye for selecting high-quality articles and his dedication to the Journal’s development have played a significant role in establishing its credibility as it stands today. I have always felt the benefit of his experience and support in this venture, and I wish him well and many further professional successes.
With this change, I am delighted to announce that Michael Joner has stepped into the role of Deputy Editor, and we warmly welcome him to the team. In reality, this is a well-deserved promotion, as Michael has already been serving as a Section Editor and has distinguished himself through his strong sense of teamwork and exceptional professionalism in managing papers, elevating them to the highest editorial standards possible. Michael is the ideal choice, and for all of us it was such a logical and consequential one, earned in the field and fully merited, that it is practically superfluous to explain it further.
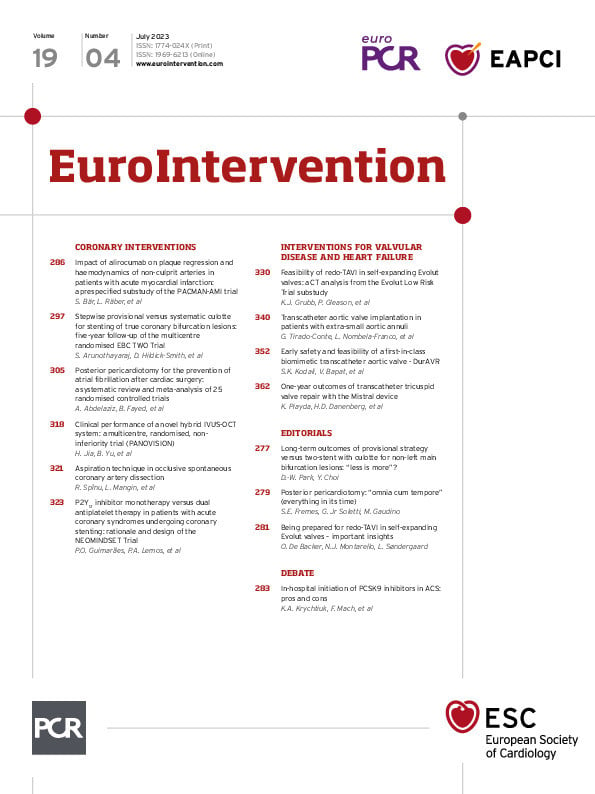
The turnover within our Journal’s team aims to maintain high standards and ensure the best for our readers. As we continue to evolve and adapt, we remain committed to delivering the most relevant and impactful content to our audience. And now, without further ado, I invite you to explore the table of contents of this issue, where you will find a wealth of knowledge and insights that reflect our ongoing dedication to excellence in interventional cardiology.
In this issue, we present a debate on whether in-hospital PCSK9 inhibitor initiation should become a standard of care for patients presenting with acute coronary syndromes (ACS). Konstantin A. Krychtiuk and Marc J. Claeys advocate that trial evidence and low rates of low-density lipoprotein cholesterol target goal achievement have opened the door for a “strike early and strike strong” approach for lipid-lowering after ACS. In contrast, François Mach and Baris Gencer caution that while PCSK9 inhibitors have their place in the management of ACS, they should not be used as an acute therapy but, rather, as a preventative therapy after discharge.
Turning to original studies in coronary interventions, Sarah Bär, Lorenz Räber and colleagues looked at acute myocardial infarction patients, reporting on the effects of alirocumab on coronary haemodynamics, as assessed by quantitative flow ratio, and percentage diameter stenosis, assessed by 3D quantitative coronary angiography, in non-infarct-related arteries. In this prespecified substudy, treatment with the PCSK9 inhibitor alirocumab added to rosuvastatin for one year resulted in significant regression of 3D quantitative coronary angiography percentage diameter stenosis compared to an increase with placebo, although it did not translate into a significant improvement in coronary physiology.
Next in coronary interventions, Sandeep Arunothayaraj, David Hildick-Smith and colleagues report on the five-year clinical results of the EBC TWO Trial. At 5 years, patients with non-left main true bifurcation disease who had received upfront culotte stenting did not gain any benefit over those who had undergone provisional stenting. Major adverse cardiovascular rates were similar between the two groups at five years, and bifurcation-specific adverse cardiac events remained infrequent in both cohorts, leading the authors to conclude that the stepwise provisional approach should remain the standard technique. This article is accompanied by an editorial by Duk-Woo Park and Yeonwoo Choi.
We then turn to a meta-analysis in the surgical space from Ahmed Abdelaziz, Badr Fayed and colleagues, evaluating the role of posterior pericardiotomy in preventing postoperative atrial fibrillation. In this systematic review of 25 studies with over 4,000 patients, they found that allowing the pericardial effusion to drain freely into the left pleural space reduces the prevalence of pericardial effusion, consequently reducing the risk of atrial fibrillation and tamponade as well as the length of hospital stay after cardiac surgery. In an accompanying editorial, Stephen E. Fremes, Giovanni Jr Soletti and Mario Gaudino discuss how study design has affected similar studies and share their optimism about the positive impact that posterior pericardiotomy could have in this field.
In a coronary intervention research correspondence, Haibo Jia, Bo Yu and colleagues report on the safety and use of PANOVISION, a novel hybrid intravascular ultrasound (IVUS) and optical coherence tomography (OCT) system. The primary endpoint for the study was to demonstrate non-inferiority to IVUS or OCT alone and then to evaluate image quality and procedural safety. In addition to higher pullback speeds, longer pullback lengths and good performance in image acquisition, the hybrid imaging system demonstrated good clinical performance and safety.
Finally, Patricia O. Guimarães, Pedro A. Lemos and colleagues present the design of the NEOMINDSET Trial, an ongoing randomised trial evaluating the efficacy and safety of single antiplatelet therapy with a potent P2Y12 inhibitor compared with traditional 12-month dual antiplatelet therapy following percutaneous coronary intervention with drug-eluting stents in ACS patients. The investigators hypothesise that single antiplatelet therapy is non-inferior for ischaemic events and superior for bleeding events compared with dual antiplatelet therapy. Enrolment is projected to finish in late 2023.
We then turn to interventions for valvular disease and heart failure. The feasibility of redo-TAVI is complexified by the native anatomy, implantation depth and the second bioprostheses, and Kendra J. Grubb, Patrick Gleason and colleagues used computed tomography-based simulations to evaluate five implantation positions of either the self-expanding Evolut-in-Evolut valves or balloon-expandable SAPIEN 3-in-Evolut valves. While redo-TAVI in an Evolut can be done in most patients, the study suggests that the lowest risk of coronary compromise was found when a SAPIEN 3 was placed at node 4 of the Evolut frame.
Small aortic annuli are common in women and have been associated with poorer outcomes after surgical aortic valve replacement. Gabriela Tirado-Conte, Luis Nombela-Franco and colleagues analyse and compare the periprocedural complications, haemodynamic performance, and midterm clinical outcomes in patients with severe native aortic stenosis and extra-small aortic annuli undergoing TAVI with either self-expanding or balloon-expandable valves. The use of self-expanding valves was associated with a lower rate of intraprocedural complications, higher device success at 30 days and better haemodynamic outcomes, while those treated with balloon-expandable valves more frequently had moderate to severe prosthesis-patient mismatch.
Does valve leaflet design impact haemodynamics and aortic flow patterns? Susheel K. Kodali, Vinayak Bapat and colleagues evaluate this question in their first-in-human trial of the DurAVR transcatheter heart valve, a biomimetic valve for the treatment of patients with symptomatic severe aortic stenosis. The DurAVR, a novel balloon-expandable valve, is moulded from a single piece of tissue into the shape of a native aortic valve, facilitating a larger orifice area and near-normal flow patterns. At 1 year, there was evidence of improved haemodynamics and normalised flow characteristics, opening the pathway for further studies.
Finally, in a research correspondence, Kerstin Piayda, Haim D. Danenberg and colleagues present the long-term outcomes of transcatheter tricuspid valve intervention with the Mistral device. This helix-shaped nitinol wire aims to reduce the coaptation gap without directly interfering with the leaflets or the annulus. The one-year outcomes showed a significant and sustained reduction in tricuspid regurgitation, along with favourable right heart remodelling.
Let’s turn to the articles now, and let them speak for themselves.