Since the Charles T. Dotter’s pioneering work, the techniques he developed have taken on more and more importance. They fully began to fly with their own wings when, in 1977, Andreas Gruentzig made medical history by performing the first successful angioplasty.1
Less than 10 year after the ground breaking work of Andreas Gruentzig, in November 1986, “a woman of Surinam extraction from China underwent the first successful stent implantation in the Netherlands. Both the procedure and the follow-up were uneventful.”
Patrick Serruys remembers that...
On that same day another woman with post infarct angina (a small subendocardial infarction) became the second candidate... Once again the procedure was technically easy and successful. Afterwards, however, complications set in when the platelet count sampled in the morning indicated a level of 600,000 platelets. Three days later the stented vessel occluded under rather dramatic circumstances, and despite immediate recanalisation with streptokinase and angioplasty, a large anterior myocardial infarction occurred.
The third patient was a young man. Ten days post stent implantation he was re-admitted with excruciating pain at the back of his thigh, accompanied by paresis of his right foot. A quick biochemical analysis revealed an increased level of CK without CK MB, as well as an adjusted and adequate anticoagulation profile. Our surgical colleagues and neurologists made the diagnosis of deep muscular haematoma which was compressing the quadriceps nerve, although earlier this was not detectable by physical examination (a complication I had never seen before). It was decided to interrupt the anti-coagulation therapy, and 2 days later the patient presented with a subacute occlusion of his left anterior descending artery, which was immediately recanalised. Subsequently the patient was sent to surgery for a single bypass graft to his LAD.
With a success rate of 33% and a failure rate of 66% it was decided to interrupt this program. Soon after Jacques Puel, Michel Bertrand, Tony Rickards, and our group had a series of ongoing multiple discussions about the optimal post treatment anticoagulant regimen. It was assumed that a large right coronary artery or bypass graft would be a more appropriate target for this device, and a stringent and extensive anticoagulation regimen was proposed including a small amount of thrombolytic drugs at the time of implantation together with heparin, persantine, dextran, aspirin, and vitamin K antagonist.
In 1987 the stent program was resumed, but this time we had to face bleeding complications. It was not unusual to have large growing haematomas, haemorrhages or gastric or retroperitoneal bleeding. The editorial published in the European Heart Journal at that time was entitled, “Are we the sorcerer’s apprentice?”, reflected our increasing doubt about the proper applicability of this therapy.2
And here we are today – on the 21st of July in 2006 – a day when we had the opportunity to sit down and have a conversation with one of our very first successfully stented patients. What follows are a series of excerpts from that conversation – Ms. Schutte: A patient’s perspective – and an historic one at that.
EIJ: ...On November 1, 1986, you were one of the first patients in the world to receive a stent in your coronaries (Figure 1). Can you still remember that day? Can you tell us about your complaints at the time?
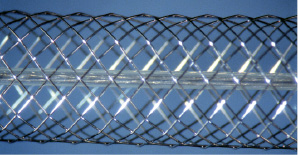
Figure 1. The Wall Stent.
Ms. Schutte: It was winter and I was shopping when suddenly I experienced severe cramps around my jaw. Initially, I thought it was because of the cold, and thought that the pain would go away once I put on my scarf. But it didn’t, the pain persisted, and I decided to go right to my general practitioner. He sent me immediately to the cardiology department of a small regional hospital for an exercise test. Based on the results, the doctors suspected a narrowing of my coronaries. The local cardiologist referred me to the Erasmus MC to see about the possibilities of an angioplasty.
EIJ: How long did you have these complaints?
Ms. Schutte: About a week.
EIJ: In the Erasmus MC you met Professor Serruys. Do you still remember his diagnosis and the treatment he proposed to you?
Ms. Schutte: Oh, yes. He told me there was a severe narrowing in one of my coronaries and then asked if I wanted to participate in a study. It was a new procedure where they would implant a sort of tube in me, instead of the conventional angioplasty with a balloon. The disadvantage of the then conventional treatment was the possibility of a substantial collapse of the coronary. He told me the preliminary results of the new procedure looked promising, and that it would be the first in The Netherlands for using this approach. I agreed to participate right away.
EIJ: You believed that the treatment would be a success?
Ms. Schutte: Sure, I thought so. I knew that there had been someone else, a man, who had participated in this study before, but he needed to have bypass surgery 2 months later. So you see, I was the first person in which the procedure was successful.
EIJ: You were born in Surinam?
Ms. Schutte: Yes, I was born in Paramaribo, Surinam, which at that time was still a Dutch colony....I had Dutch nationality. My family moved to The Netherlands when I was still very young and decided to stay.
EIJ: When Professor Serruys interviewed you 10 years ago you told him you still felt like a guinea pig (Figure 2). What is your reaction today, especially if I tell you that we’re using stents like yours in more than 3 million procedures worldwide each year?

Figure 2. 1996 interview between Ms. Schutte and Prof. Patrick W. Serruys.
Ms. Schutte: That’s great, it seems they’ve improved a lot.
EIJ: Do you still follow the news about developments in this field?
Ms. Schutte: Absolutely! When I come across an article in a journal, or when I see something on television... I’m also curious to see what’s been happening and what’s changed. That’s very important to me.
EIJ: How do you feel now? What are your daily activities?
Ms. Schutte: I feel very well. I’m living without any complaints. I like gardening, and also taking my dog for a walk.
EIJ: And the pain you felt in 1986? Did it ever return?
Ms. Schutte: Not at all. After the treatment the doctors provided me with some sublingual nitroglycerin, but I never needed it.
EIJ: Do you still carry these drugs?
Ms. Schutte: Yes, I do. I still carry nitroglycerin spray in my purse. I feel safer with it, just in case I might need it one day. Anyway, it might be useful for someone else.
EIJ: Can you tell me about the drugs you used in 1986, and about the drugs you’re using now?
Ms. Schutte: At that time I was using metoprolol, nifedipine and several other drugs...but I can’t remember their names. Now I’m on aspirin (38 mg), atorvastatin (20 mg) and candesartan (8 mg).
EIJ: In 1987, one year after the stent implantation, we performed a repeat angiography. The stent was fully patent. Today we’re going to perform a multislice CT scan to check your coronaries (Figure 3).
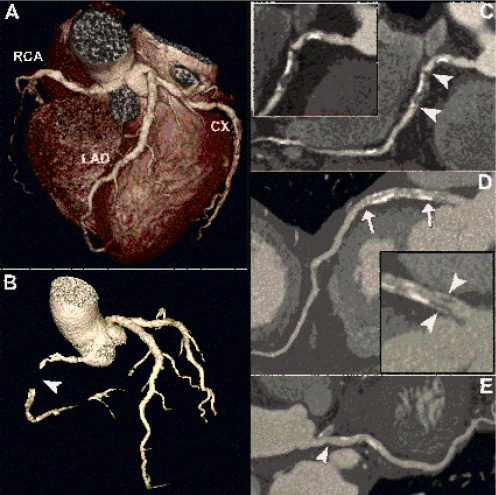
Figure 3. CT coronary angiography 20 years after stenting of the left anterior descending coronary artery (LAD). The 3D volume-rendering image gives an overall overview of the cardiac anatomy (A). Despite being asymptomatic, this patient shows clear progression of coronary artery disease as demonstrated by an occlusion of the right coronary artery (RCA, arrowheads in panels B and C) and a 50% narrowing (panel D inset, arrowheads) at the proximal stent edge of the LAD. The stent edges are marked by arrows (panel D). The circumflex artery shows a non significant narrowing in its proximal part (panel E, arrowhead).
The advantage of this technique is that a catheter isn’t necessary any more. Inherent risks, like bleeding in the groin, disappear with this investigation... and because of that we won’t need to hospitalise you.
Ms. Schutte: Wonderful...
——— After the MSCT scan ————
EIJ: How was the MSCT scan?
Ms. Schutte: It was great. The scan took only 20 seconds and you can go home immediately afterwards. I hope it will be widely used... and soon!
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1.
Moving image 2.