Abstract
Aims: To assess efficacy and safety of oral treatment with prednisone at immunosuppressive dose after percutaneous coronary interventions (PCI) in patients with multi-vessel coronary artery disease (CAD).
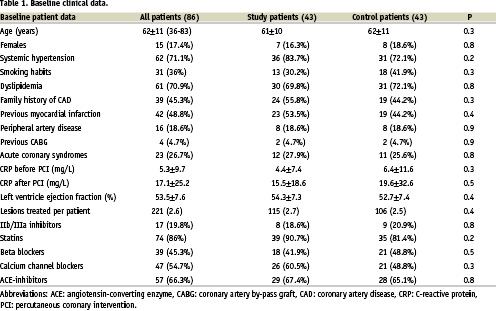
Methods and results: Eighty-six consecutive patients with multi-vessel CAD were successfully treated with multiple PCI. Forty-three patients (115 coronary stenoses), with C-reactive protein >3mg/L 48 hours after PCI and in absence of contra-indications received 45-day high-dose oral prednisone treatment (study-group). Forty-three patients (106 coronary stenoses), did not receive prednisone (control-group). The primary clinical endpoint was 12-month event-free survival rate (defined as freedom from death, myocardial infarction, and the need for target vessel revascularisation). Angiographic restenosis at 8 months was assessed in the study group only. Event-free survival rates were 93 and 69.8% in the study and the control group, respectively (relative risk 0.34, 95%CI: 0.12 to 0.96, p=0.006). Target vessel revascularisation rate in the study group was 7% compared to 27.9% in the control group (p=0.01). Quantitative coronary angiography performed on 104 lesions of 39 prednisone-treated patients (91%) showed 4 restenotic lesions (3.8%). The mean late lumen loss was 0.61±0.35mm and loss index 31.3±21.6%.
Conclusion: Oral immunosuppression with prednisone effectively reduces clinical restenosis in patients undergoing complex, multi-vessel PCI.
Introduction
The sustained evolution of percutaneous techniques has further enlarged indications of non-surgical myocardial revascularisation means to a wider spectrum of patients with coronary artery disease (CAD). Specifically, the advent of drug eluting stents (DES) has reduced restenosis rates and consequently has fostered the enthusiasm for extending the indications of percutaneous coronary intervention (PCI) to more complex patients1-5. The use of DES however is burdened by the high economic cost (in particular if several units are required as in patients with multi-vessel CAD), and this limits its applicability in most medical care services world-wide and in particular in countries with limited resources. Furthermore, the safety and long-term efficacy of either Sirolimus or Paclitaxel DES implantation in patients with multi-vessel CAD remains to be determined. Nevertheless, observations derived from a non-randomised comparison of patients treated with multiple Sirolimus-DES implantation with the surgical arm of the ARTS I study6 suggest that, at the short-term, multiple DES implantation in patients with multi-vessel CAD may be equivalent to coronary artery bypass graft (CABG)7. Although this comparison needs confirmation from randomised studies, it appears to be a possible alternative to CABG.
The importance of inflammation in the mechanisms of restenosis is well known8-9. Accordingly, sustained immunosuppressive doses of oral prednisone in patients with single vessel stent implantation proved the efficacy of steroids to prevent restenosis in the randomised IMPRESS study10. Further evidence in support of a systemic pharmaceutical approach to reduce restenosis has been recently provided by the ORBIT11 and the OSIRIS12 investigators. Both studies have demonstrated the anti-restenotic capabilities of rapamycin given orally in patients with “de novo” lesions and with in-stent restenosis respectively.
Following the encouraging results previously obtained by our groups in IMPRESS 1, this trial aimed to test the safety and the efficacy of the simple and inexpensive corticosteroid treatment to prevent restenosis after PCI in the challenging clinical and angiographic setting of patients with diffuse and multi-vessel CAD and elevated C-reactive protein (CRP) levels. Conventional PCI techniques were therefore used instead of DES as an alternative, in many cases, to conventional CABG.
Methods
Between March 2002 and May 2003, 117 consecutive patients with multi-vessel CAD were treated with multiple PCI in the two academic institutions participating in the study. Patients entering this prospective registry were informed of the experimental nature of the medical treatment and of the alternative of a surgical revascularisation in some cases. All patients who enrolled gave their informed consent according to the ethical regulations of the relevant institutions.
Study design
All patients were pre-treated with aspirin and a thienopiridine, either ticlopidine (250mg bid for 72 hours) or clopidogrel (300mg loading at least 6 hours before PCI); the thienopiridine was continued for one month and aspirin indefinitely. Statins were recommended in all patients. Following PCI, total creatine kinase and its MB isoform, were measured at 6, 12 and 24 hours. Elevation of creatin kinase MB >3 times the upper normal limit during the follow-up period was registered as a myocardial infarction.
CRP levels were measured before and 48 hours after PCI using a high-sensitivity method. Patients with high CRP levels (>3mg/L)13 and in absence of contra-indications were prescribed high-dose oral prednisone at hospital discharge. The study exclusion criteria were as follows: DES implantation, life expectancy <24 months, the occurrence of any in-hospital complication related to the PCI procedure, contra-indication to the use of aspirin or thienopiridines, and contra-indications to high-dose steroid use including: diabetes, recent myocardial infarction (<3 weeks), active peptic ulcer, active infectious disease, and uncontrolled severe hypertension. The potential undesirable metabolic effects that high dose steroids could induce in diabetic subjects withheld the investigators from treating such patients. No restriction was utilised for the clinical presentation of angina, the angiographic characteristics of the coronary lesions and the PCI strategy, except the employment of DES.
The scheme of the steroid treatment was the same as that used in the IMPRESS randomised trial10; briefly, prednisone was given orally at a dose of 1mg/kg for 10 days, 0.5mg/Kg for 20 days and 0.25mg/kg for 15 days. This dosage was chosen from the immunossupressive protocol utilised for heart transplantation.
All patients were controlled clinically 45 days after the procedure. The outcome was analysed per protocol. Those treated with steroids were screened for the correct and complete assumption of the steroid therapy and the eventual occurrence of side-effects. All patients underwent a provocative stress test within 6 months of the PCI and a subsequent out-patient clinic control. Angiographic follow up was scheduled for the steroid-treated patients only, 8 months after PCI, to assess the occurrence of angiographic restenosis. At twelve months after the index procedure, and twice a year thereafter, all patients were controlled in the out-patient clinics by assigned independent clinicians to verify the incidence of any major adverse cardiac event (MACE) comprised in the primary endpoint: one-year incidence of death (from any cause), myocardial infarction after discharge (defined as the rise and fall of creatin kinase-MB and ischemic electrocardiographic changes suggestive of acute myocardial ischemia), and recurrence of symptoms or ischemia requiring revascularisation. Target lesion revascularisation (TLR) and target vessel revascularisation (TVR) were also assessed.
Pecutaneous coronary intervention and quantitative coronary analysis (QCA)
Interventions were performed employing either the femoral or the radial approach. All patients had multi-vessel interventions. Unfractioned heparin was always used intravenously to maintain an activated clotting time >250 seconds during the procedure. Whenever possible, the “spot stenting” technique was preferred to the full coverage with stents in cases of diffuse coronary disease. PCI were considered successful when a % diameter stenosis (%DS) ≤30% and a TIMI flow ≥2 was obtained in each lesion treated. Angiographic recordings for QCA were obtained in at least two orthogonal views of each of the coronary segments treated, after the administration of intracoronary nitroglycerin. At follow-up angiography the same orthogonal views were obtained. The compact discs containing the angiographic images were sent to an independent core laboratory (European Imaging Laboratory, Rome, Italy) for centralised QCA using the automated edge-detection system CMS (Medis Medical Imaging Systems), as described elsewhere10. All the lesions recorded at baseline, after PCI and at follow-up were of adequate quality for QCA; and the value of all lesions were used for statistical calculations.
Statistical analysis
Continuous data are expressed as means and standard deviations; discrete variables are given as absolute values and percentages. Appropriateness of the sample size was estimated considering the findings obtained in the previous IMPRESS study that used the same endpoint and steroid therapeutic scheme. Clinical events at 12 month were reduced from 35% in the control group to 7% with prednisone10. The sample size of IMPRESS 2 MVD was therefore calculated expecting a similar 70% difference between two groups (expected occurrence of clinical events 30% in controls and <10% in prednisone-treated patients). To test this hypothesis, 40 patients per arm were calculated to offer a 90% beta power at a two-sided significance level of 0.05. The study included 86 patients to account for possible drops-out at follow-up. The Student’s t-test was used to compare differences between continuous variables. The chi-square statistic with Yates’ correction, or Fisher’s exact test when appropriate, were used to test associations of categorical data. A logistic multivariate model was tested to assess the predictive value of factors related to the occurrence of clinical events. The parameters of the model included: treatment with prednisone, left ventricle ejection fraction, angiographic lesion type, length of the stented lesion, and vessel diameters calculated on-line by QCA before and after PCI. The event-free survival curves were obtained by Kaplan-Meier method and compared by log-rank test (Figure 1).
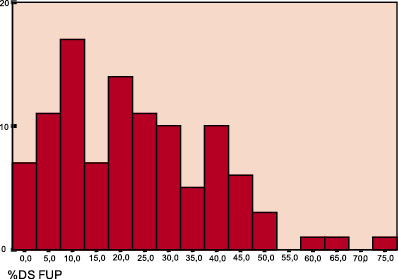
The distribution of late loss and the %DS of the treated lesions at follow-up were analysed by a frequency distribution curve (Figure 2). Calculations and graphs were made using the SPSS software (9.0 release for Windows). A probability value of less than or equal to 5% was considered significant.
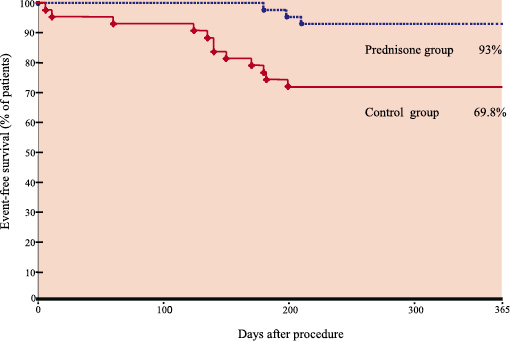
Figure 1. Event-free survival curves (death, non-fatal myocardial infarction and repeat revascularisation due to recurrence of ischemia) in the two study groups at 12 months follow-up. Log-rank= 8.14, p=0.004.
2a
2b
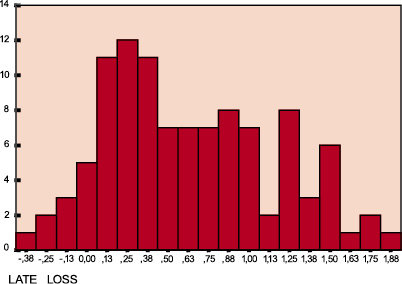
Figure 2. Frequency distribution curves of the %DS (a) and the late loss (b) at follow-up of the cortisone-treated lesions. Both indexes are non-normally distributed and skewed towards the lowest values (median %DS= 20%, and late loss= 0.45mm).
Results
Patients
Of the 117 consecutive patients treated with multi-vessel PCI during the study period, 21 (18%) were diabetics, 6 had been admitted for acute myocardial infarction, and 4 had in-hospital complications after PCI (3 revealed creatin kinase MB release as defined for non-Q wave myocardial infarction and 1 needed blood transfusion and vascular surgical repair at the puncture site). These patients were not considered for inclusion in the study. Therefore, 86 patients were registered. Forty-three patients showed persistently high CRP levels 48 hours after PCI, had no contra-indications to steroids, and subsequently completed the 45-day oral treatment with cortisone; these patients represent the study group. Of the remaining 43 patients (control group), 12 (13.9%) reported a history of significant gastric-duodenal disease, 9 (9.3%) received at least one DES, 10 (11.6%) had evidence of normal CRP values before hospital discharge, 3 patients refused an elective angiographic follow-up and 4 patients initially screened for the drug therapy did not start the cortisone treatment. Other 6 patients, without exclusion criteria, were included in this group to match an identical number of prednisone cases.
The 43 patients of the study group started the steroid treatment 3.5±0.5 days after PCI. Of these, 25% had elevated CRP levels before the PCI and 75% showed CRP elevation only after PCI. Patients were treated on 115 coronary lesions (2.7 per patient); 13 lesions (11.3%) were treated with balloon angioplasty only while 119 stents were placed on the remaining 102 lesions. Rotational atherectomy was needed in one case of very calcified and diffuse left anterior descending CAD; directional atherectomy was used in a left anterior descending lesion before stenting. Eleven lesions (9.6%) were chronic total occlusions. Thirty-two percent of stents were deployed without lesion predilation (direct stenting).
In the 43 patients of the control group, 106 lesions were treated (2.5 per patient); 16 lesions (15.1%) were treated with only balloon angioplasty and 90 with 96 stents. Rotational atherectomy was needed in 2 cases of very calcified and diffuse lesions. Seven lesions (6.6%) were chronic total occlusions. Direct stenting was performed in 29.2% of lesions.
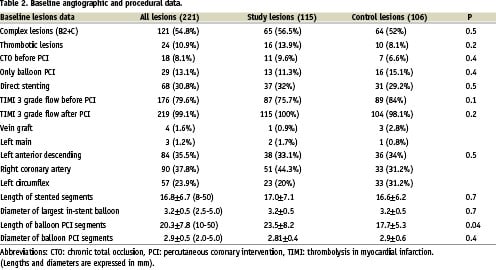
Baseline clinical, angiographic and procedural details of all patients are presented in tables 1 and 2.
Clinical primary endpoint
Clinical follow-up was obtained in all patients at 12 months. In the study group 6 patients (14%) reported side effects to prednisone therapy. Three complained of gastric pain, 2 had an increase in blood pressure and 1 had fluid retention. Side-effects did not require treatment suspension and were always controlled medically. During follow-up, no patient died or suffered myocardial infarction; recurrence of stable angina occurred in 2 patients (4.7%); one underwent TLR (on 1 out of 5 lesions previously treated), and one could not repeat coronary angiography for geographical reasons (his symptoms were controlled with the upgrading of medical treatment). Repeated TLR was performed in 2 additional patients without signs or symptoms of ischemia showing moderate angiographic restenosis (DS%>50<60). Total TLR rate per patient was therefore 7% (3/43) and it was identical to the TVR rate.
In the control group 2 patients complained of gastric pain after discharge and were managed with anti-acids. Two patients (4.7%) died, both after reinfarction within the first month after PCI; 2 patients had a non-fatal non-Q wave myocardial infarction due to sub-occlusive restenosis manifesting 4 months after discharge, one received a new PCI and one was treated medically; 10 patients (23.3%) underwent TLR, in 9 cases because of symptoms recurrence (PCI in 7 patients and CABG in 3). In two patients needing TLR due to restenosis, a progression of disease was also observed in other coronary segments. Total TLR rate per patient was 23.3% while the TVR was 27.9% (Table 3).
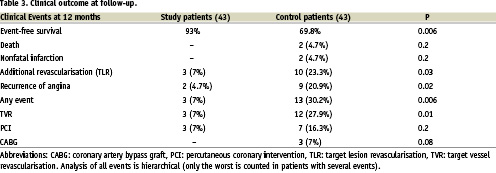
The occurrence of MACE was reduced therefore from 30.2% in the control group to 7% with prednisone (relative risk 0.34, 95%CI: 0.12 to 0.96, p=0.006) and the event-free survival at 12 months was 93% in the study group and 69.8% in controls; log-rank= 8.14 p=0.004 (Figure 1). From multivariate regression analysis, treatment with prednisone was the only independent variable that correlated with the occurrence of MACE: relative risk 0.39, 95%CI: 0.17 to 0.62, p=0.001.
Angiographic results
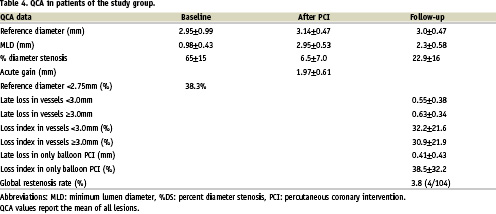
Thirty-nine of the 43 prednisone-treated patients underwent protocol angiographic follow-up (91%) at a mean time of 280±126 days. QCA was performed on 104 of the 115 treated segments. Three patients refused to repeat angiography because they were totally asymptomatic and had a negative stress test. One patient with recurrence of angina could not repeat angiography as mentioned before for geographic reasons. The angiographic endpoint of binary restenosis rate (DS%≥50) inside the stent, within 5mm of the stent edges or in the segments treated with balloon angioplasty was 3.8% (4 out of 104 lesions); no sub-acute occlusion occurred, no vessel was totally occluded, there was no image of edge effect, and only one of the 4 restenotic lesions had a %DS >60%. The mean late lumen loss per patient was 0.61±0.35mm and loss index 31.3±21.6%. Late lumen loss in patients with high CRP levels before PCI was 0.76±0.46 mm, compared to 0.55±0.31 mm in patients with normal CRP before PCI (p=0.2).
Restenosis occurred in 2 cases within short stents (13 mm each), and in 2 cases in the gap left between 2 adjacent stents. Details of the QCA provided by the core laboratory are reported in table 4. Of note, 38.3% of treated vessels were smaller than 2.75 mm before PCI. Late loss >1 mm was observed in 26 lesions, always treated with stents. Figure 2 shows the frequency distribution of the %DS and late lumen loss of the treated lesions at the QCA follow-up. In both graphics measurements are clearly skewed toward lower levels.
Discussion
The results of this prospective, non-randomised, observational assessment of the clinical and angiographic outcome of patients undergoing multi-vessel PCI show that 45-day oral therapy with prednisone is efficacious in reducing the occurrence of clinical events in patients with complex coronary lesions and high post-PCI CRP levels.
On the one hand, elevated serum CRP level has been proposed as a possible marker of augmented risk for clinical events in subjects with CAD14-15 and for restenosis after PCI16; on the other hand, the multi-vessel extension of the CAD is itself a strong predictor of events after conventional PCI. Despite the high-risk profile of our patients, oral immunosuppression with prednisone was associated with a remarkable low-rate of clinical events at follow-up and of angiographic restenosis as shown by QCA data. The advantage of systemic treatment in a MVD population is also supported by the notion of an inter-lesion dependence of the risk of restenosis in patients treated with multi-vessel stenting, suggesting a patient and not only a lesion-derived propensity to restenosis in patients with multiple lesions17.
Because of the importance of inflammation in the mechanisms of restenosis, anti-inflammatory therapy with steroids after PCI has been experimented previously18-20. In particular, the randomised, placebo controlled M-Heart study18 and a randomised study by CW Lee et al.19 showed that neither a single i.v. bolus administration of methylprednisolone given before PCI nor an i.v. bolus followed by 1 week oral administration of prednisone20 reduce restenosis. Several possible reasons can explain the apparently conflicting results between our study and these previous trials. The most obvious is the different dosage and length of the steroid treatment. Indeed, a single low-dose approach or a short one-week drug scheme are unlike to achieve immunosuppressive effects and to arrest the tissue growth that ensues the vessel wall injury caused by PCI8-9. Steroids exert beneficial effects on platelet function, on smooth muscle cells proliferation and on collagen synthesis as well as inflammatory cells migration and activation, thus interfering with several steps of the cascade leading to neo-intima formation and subsequent lumen loss21-22. However, systemic immunosuppressive effects as those obtained in our studies are dose-dependent and require weeks of treatment to be achieved23. Finally, the steroid treatment in our experience has been focused on subjects with elevated CRP levels after PCI. In this setting, anti-inflammatory drugs may be more efficacious than in non selected patients.
The findings reported in our work confirm and expand the results observed previously by our groups in the IMPRESS randomised study10. IMPRESS was performed on a highly selected population treated with single stent implantation on the culprit lesion and with evidence of normal CRP level at baseline and sustained elevation 72 hours after PCI. The findings of this study were of limited clinical applicability but served as a proof of concept for the rationale of targeting inflammation systemically with oral steroids to prevent restenosis. The present registry included some patients with complex coronary anatomy such as chronic total occlusions, diffuse and/or calcified lesions, thrombotic and bifurcation lesions and small vessels, representative of a difficult “real world” population. Multiple PCI were performed using different techniques, with infrequent use of IIb/IIIa glycoprotein inhibitors (19%) and intravascular ultrasound guidance (12%), disregarding the value of basal CRP and with a large use of statins. Although sub-analysis of the different lesion types and PCI strategies would not have been statistically meaningful, the angiographic results at follow-up were consistently good in all cases that frequently included challenging anatomies, as the one depicted in Figure 3.
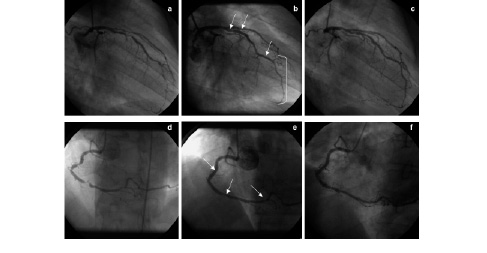
Figure 3. Left and right coronary angiograms of the same patient. Left anterior descending artery before PCI, the distal circumflex is chronically occluded (2a). After a 3.0 x 13 mm stent implantation in the mid segment, 2.5 x 16 mm stent in the distal segment, and 2.5 x 26 mm stent in the diagonal branch (arrows), and only balloon PCI (2.5 mm diameter) over 50mm of the distal segment of the vessel (between brackets) (2b). Elective 8-month control angiography with almost unchanged result compared to post-intervention images (2c). Right coronary artery before PCI (2d). After a 3.0 x 13 mm stent implanted in the proximal segment, only balloon dilatation with a 3.0 mm balloon in the mid segment and a 2.5 x 13 mm stent in the distal tract (arrows) (2e). Elective 8-month control angiography (2f).
The late lumen loss observed in this study (0.61±0.35mm) is larger than the late loss of the previous IMPRESS (0.39±0.6mm) despite the identical drug scheme, a difference that may reflect a more severe form of atherosclerotic disease in patients with diffuse and multi-vessel CAD and worse co-morbidity, as suggested by the smaller vessel diameters in the registry. Another hypothesis is the possible detrimental effect of a more prolonged and sustained action of high CRP levels before steroid treatment in many patients of the registry compared to the previous study. However, the late lumen loss reported in our study is nearly half of that reported in randomised trials with use of modern bare metal stents implanted in single lesions1-5, much lower than that expected in clinical practice according to our patients characteristics24, and not comparable with other series of multi-vessel stenting17,25 because no QCA information is available in this setting. Late lumen loss after DES implantation is even lower (<0.4±0.5mm); yet it has been demonstrated that a late lumen loss ≤0.6 mm is sufficient to reduce clinical restenosis below 5-10%4. Within such a reduced range of in-stent proliferation, further minimal angiographic differences might be clinically meaningless.
As to the clinical results of our registry, 4.7% rate of recurrence of angina at 12 months in patients with multi-vessel CAD is very similar to that observed in the randomised IMPRESS study, confirming both the systemic efficacy of the treatment and the appropriateness of the calculated study sample size. Furthermore, the results of our registry compare favourably with those of the much larger RESEARCH registry26. In this non-selected population of patients treated with Sirolimus-DES implantation the recurrence of angina was indeed 3.7% at one year. Although the population enrolled in the RESEARCH registry is closer to “real-life” than in randomised trials, the indiscriminate Sirolimus-DES implantation in all-comers may not be representative of a real-life interventional approach world-wide.
Our patients were treated quite aggressively (2.7 lesions per patient, acute gain 1.97±0.61mm) and their clinical outcome is equivalent to that observed in patients revascularised by means of modern CABG techniques6. Comparison with other series of patients with MVD suggest that prednisone treatment may provide similar results to those obtained with multiple DES implantation in ARTS 2 (six-month MACE rate 6.4% including diabetic patients)7. Conversely, the dismal outcome obtained with multi-vessel PCI and bare metal stents in the control group confirms the known poor value of this alternative6.
Study limitations
Whether the results obtained in the study group apply to patients with persistently elevated CRP levels only, or can be obtained also in patients with normal CRP remains to be determined in future studies.
The study is limited by its non-randomised, non-blinded nature. However, it was not the intention of the authors to repeat the previous IMPRESS experience, but rather to test its applicability, safety, and clinical efficacy in the real-world context of a prospective, controlled registry. This objective was accomplished in a high-risk population that is normally excluded from randomised trials. Indeed, all our patients presented at least one exclusion criteria to enter studies like RAVEL, SIRIUS, or TAXUS1-5 and the accurate angiographic analysis of the prednisone-treated group supports the therapeutic potential of this systemic approach. However, the lack of systematic QCA in the control group does not allow quantifying the “anti-restenosis effect” of the steroid treatment suggested by the excellent clinical outcome.
The exclusion of diabetic patients remains the main limitation of the applicability of this strategy. Diabetic patients bare a high risk for restenosis after PCI, making CABG, and possibly DES implantation, a much better option6-7. The potential undesirable metabolic effects that high-dose steroids could induce in diabetic subjects withheld the investigators from treating such patients.
Conclusions
Diffuse multi-vessel CAD is a challenging subset of patients in which PCI is often complicated by a high incidence of adverse clinical events, mainly target vessel failure, and elective CABG still offers superior results6. With the advent of DES this type of patient is being treated also percutaneously, but definitive information about the outcome and the economic impact of this strategy is still awaited.
The administration of oral prednisone after conventional PCI offers promising results that may be an interesting alternative to more expensive treatments, particularly in countries with limited resources. This strategy can be safely applied to an important proportion of patients after exclusion of diabetics and those with contra-indication to high-dose prednisone.
Unlike sponsored studies, the independence of our research, conducted without economic support from industry or any other financial source, represents the strength of a study of this nature, conceived and developed without conflict of interest.

