For some time, we have been witnessing a silent revolution that concerns the way we debate and discuss our science. Anyone can discuss and debate in public, and certainly on the occasion of a scientific event, and the lucky ones can do so directly with the authors. Today, however, I am speaking about written reactions.
In the past, anyone who wanted to express an opinion contrary to the contents of an article could do so by writing a Letter to the Editor – and in fact you can still do this. Then came the journal websites, and some offered a form that could be easily filled out below the articles where anyone could leave their comments. This passage from one medium to another already tells us something about the language difference necessary to assert one’s reasons – more formal in the first case, more casual in the second.
The next stage of this imaginary journey is represented by social networks –in particular, Twitter for interventional cardiology– which provides an ever-open window on scientific literature. In this always open parallel debate, the tones can be quite harsh, favoured by the necessary brevity of the form.
Anyone who follows social networks will know about recent discussions on divisive themes. The debate between individuals on certain topics is too important to be traced back to a short paragraph, but I want to share a feeling. When someone posts a clinical case and just asks the community for an opinion on the best strategy based on clinical and anatomic characteristics, the debate invariably becomes less hostile and more focused. Abandoning the reciprocal positions, the convergence is total and focused on the interest of the individual patient, which reproduces the constructive and professional atmosphere of a hospital meeting. Sometimes I think that it could be a good idea to do the same thing in our public debates – talk more about science through clinical cases. It could make the tone more informative and less dramatic.
That said, our task on these pages is to select the best science to inform and guide your interventional practice on a case-by-case basis. Here is the usual summary of the present issue.
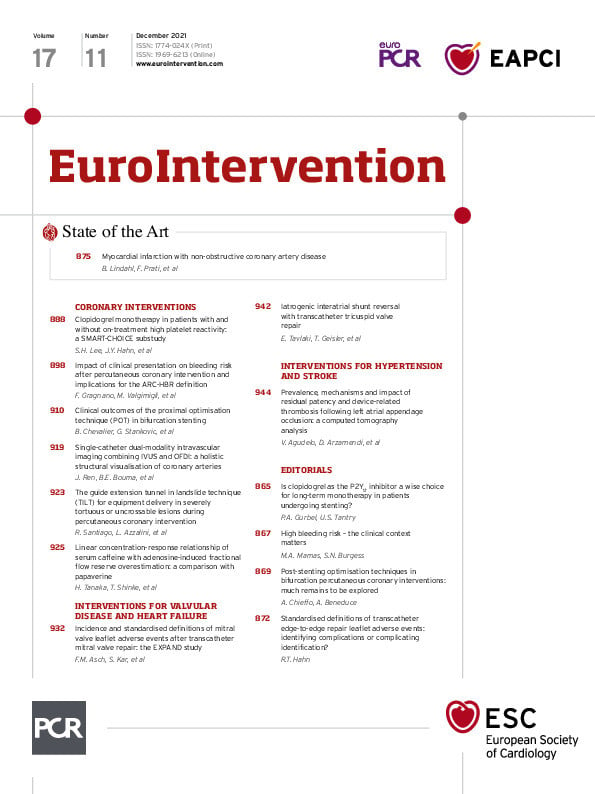
Myocardial infarction with non-obstructive coronary arteries – MINOCA – has been increasingly studied over the last decades yet remains difficult to fully assess with challenges to its diagnosis and management as well as a lack of a clear consensus on its definition. In this EuroIntervention State of the Art, Bertil Lindahl, Francesco Prati and colleagues define the disease and present our current understanding of MINOCA, including its epidemiology and treatment. The authors take a close look at imaging modalities and the use of non-invasive imaging, such as computed tomography (CT) scanning, which could be a key in future MINOCA diagnosis as well as in those areas that need further research to fill in the gaps of our understanding of this disease which can be observed in up to 10% of patients, most of whom are women.
In coronary interventions, Seung Hun Lee, Joo-Yong Hahn and colleagues present the results of a substudy from the SMART-CHOICE trial looking at the impact of clopidogrel monotherapy in patients with and without on-treatment high platelet reactivity. While it was seen that high platelet reactivity was linked to high rates of major adverse cardiovascular and cerebrovascular events in patients receiving clopidogrel monotherapy, the use of clopidogrel plus aspirin provided no additional benefits in these patients. Bringing in to question the use of clopidogrel in this situation, the authors point to the possible use of more potent P2Y12 inhibitor monotherapy, though further research is still needed. This article is accompanied by an editorial by Paul A. Gurbel and Udaya S. Tantry.
How does the clinical presentation of a patient undergoing percutaneous coronary intervention (PCI) play out in terms of bleeding risk? And, is this reflected in the Academic Research Consortium’s High Bleeding Risk (ARC-HBR) criteria? Felice Gragnano, Marco Valgimigli and colleagues investigated the impact of clinical presentation on bleeding risk in more than 16,800 all-comer patients undergoing PCI and looked at the results in relation to the ARC-HBR criteria. Clinical presentation was seen to have a correlation with the risk of bleeding in patients presenting with acute coronary syndromes (ACS) who showed a tendency to a greater bleeding risk than those presenting with chronic coronary syndromes (CCS). Clinical presentation thus does have an effect on bleeding risk after PCI, when examined in light of the ARC-HBR criteria, though the authors concluded that ACS was less accurately characterised than CCS and should be added as an additional minor risk criterion to the ARC-HBR criteria to further bolster its applicability. In general, clinical presentation can affect the risk of bleeding events after PCI and should be taken into account. This article is accompanied by an editorial by Mamas A. Mamas and Sonya N. Burgess.
Can post-implantation deployment techniques influence the clinical outcomes of bifurcation stenting? This was the question posed by Bernard Chevalier, Goran Stankovic and colleagues in the next article drawn from the e-ULTIMASTER registry. They found that the use of the proximal optimisation technique (POT) was associated with a reduction in the event rate, while the kissing balloon technique had limited influence, leading the authors to conclude that the POT would be a better deployment technique when approaching bifurcation stenting. This article is accompanied by an editorial by Alaide Chieffo and Alessandro Beneduce.
Jian Ren, Brett E. Bouma and colleagues present their latest laboratory research using a dedicated algorithm and novel single-catheter dual-modality system which combines intravascular ultrasound (IVUS) with optical coherence tomography (OCT)/optical frequency domain imaging (OFDI). When used in the coronary arteries, this system establishes what the authors call “a holistic structural visualisation”. Laboratory testing demonstrated how this system could aid in PCI by providing complementary diagnostic information in a single-colour, easily grasped map that shows both macro- and microstructures of the coronary arterial wall and its disease burden.
Does your patient’s morning cup of coffee impact your fractional flow reserve (FFR) measurement? Authors Hideaki Tanaka, Toshiro Shinke and colleagues study the association between serum caffeine level and adenosine-induced FFR, concluding that a cup of coffee does have a direct impact on adenosine-induced FFR overestimation, underlining the importance of standardised caffeine control to ensure accurate adenosine-induced FFR measurements.
Turning to valvular disease and heart failure, Federico M. Asch, Saibal Kar and colleagues look at different types of leaflet adverse events related to MitraClip NTR/XTR in the EXPAND study in order to provide a series of standard definitions for the different types of leaflet adverse events observed. The most serious of these, leaflet injury, was seen to occur during implantation, while single leaflet device attachment was often observed during implantation or at follow-up. Taken as a whole, leaflet adverse events were low, with the authors hoping that these definitions would help in identifying these events and aid in their diagnoses and management. This article is accompanied by an editorial by Rebecca T. Hahn.
Using cardiac CT angiography, Victor Agudelo, Dabit Arzamendi and colleagues sought to clarify the definition, prevalence, mechanisms and clinical impact involved in left atrial appendage patency and device-related thrombosis following left atrial appendage occlusion. The authors observed malapposition, peri-device leakage and fabric permeability as the most common mechanisms, though patency itself was not associated with adverse clinical events or outcomes.
And now, on to the articles themselves.
Supplementary data
To read the full content of this article, please download the PDF.