Recently, one of my Fellows said: “I follow scientific journals through Instagram”; and I remember I couldn’t believe my ears.
I was under the impression that with Twitter, the mission of the Journal’s digital presence on social media was abundantly satisfied and I didn’t think there was much room for improvement. As those who follow EuroIntervention through Twitter are aware, our social media board and staff manage the EuroIntervention account with care in order to distil the best of our content, in the most useful way possible, so that our audience can receive concise, timely and graphically appealing information. But Instagram was far beyond my imagination, as it is notoriously a visual social network by vocation. When I looked at Instagram all I saw was no texts, no links and a square image.
“Sorry, dear Fellow, in what sense can you follow scientific literature via Instagram, how is this possible?”
A few live demonstrations followed, smartphone in hand, and a whole world opened up to me; respected journals with high impact factors are very active on Instagram and produce an enormous amount of content.
“Yes, but how do you follow a Journal on Instagram if you can’t link to articles?” I asked. And it was at this point I became the Fellow while my Fellows became my mentors. “There are posts, there are stories, and then polls, hashtags, countdowns and so on and so forth”, they told me.
I discovered a whole generation of young interventionalists who browse their mobile phones like a catalogue, attracted by the most captivating images, which then brings them back to a Journal and its related content. Unlike PubMed, it is not you who are looking for the articles, but the articles who are looking for you. And some Journals really do it perfectly.
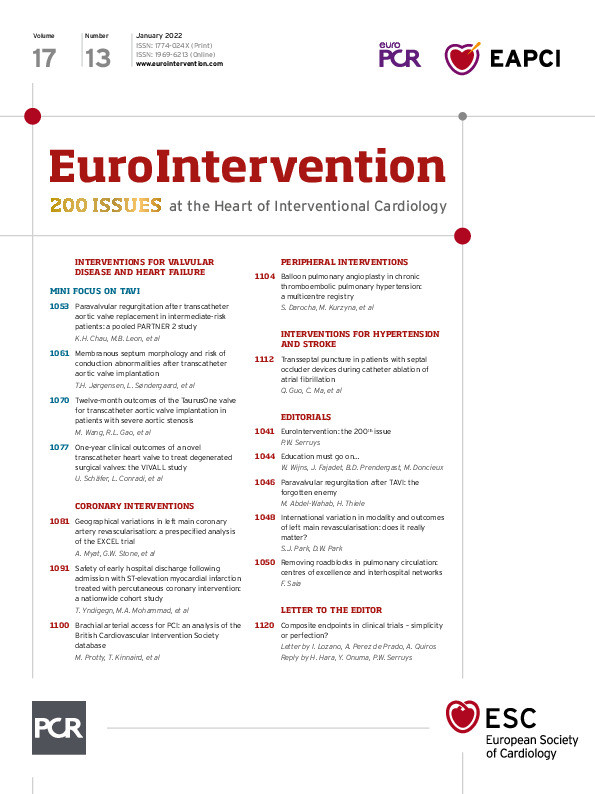
So, the challenge was accepted. EuroIntervention has landed on Instagram (@eurointervention), yet another step in our digital transition. I’m announcing it in this issue of the Journal because it is symbolic – it is our 200th issue since we began publishing and, while we are respectful of our history, we like to look resolutely towards the future as well.
We will return to this subject later, but in the meantime, here’s what we’ve prepared for you this month (which some of you will discover on Instagram, others on Twitter and still others on PubMed).
Our first 2022 issue includes a mini focus on transcatheter aortic valve implantation (TAVI), beginning with an article on paravalvular regurgitation (PVR). Katherine H. Chau, Martin B. Leon and colleagues explored the mechanisms underlying the increased mortality seen in patients with moderate or worse PVR post-TAVI, evaluating data from the PARTNER 2 study. Their findings show that adverse cardiac remodelling associated with PVR could be part of the explanation for worsening outcomes, and they emphasise the importance of these findings in avoiding PVR post-TAVR. This article is accompanied by an editorial by Mohamed Abdel-Wahab and Holger Thiele.
The TAVI mini focus continues with a look at the morphology of the membranous septum, specifically whether the relationship after TAVI of the membranous septum and transcatheter heart valve (THV) implantation depth could predict the risk of new-onset conduction abnormalities. Troels H. Jørgensen, Lars Søndergaard and colleagues found that post-TAVI there was an increased risk the greater the overlap of the THV with the lower border of the membranous septum, leading the authors to encourage operators to consider membranous septum morphology in the planning of their procedures.
Moyang Wang, Runlin Gao and colleagues evaluated the safety and efficacy of the self-expanding TaurusOne valve in treating symptomatic severe aortic stenosis. The China TaurusOne TAVI study showed improved haemodynamic results and quality of life scores with similar results for patients with either bicuspid or tricuspid aortic valves.
Our last article in the TAVI mini focus looks at the VIVALL study on valve-in-valve (ViV) implantation using the ALLEGRA transcatheter heart valve. In this first-in-human clinical study and in vitro tests, authors Ulrich Schäfer, Lenard Conradi and colleagues find this novel device to be safe with favourable results in the ViV treatment of failing surgical aortic valves, even those with very small inner diameters.
Are there regional variations in outcomes of left main coronary revascularisation? To explore this question, Aung Myat, Gregg W. Stone and colleagues used data from the EXCEL trial to see whether outcomes after percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) for left main coronary revascularisation remained consistent whether they are from European or North American trial centres. Studying differences in the patient demographics, anatomy, pharmacotherapy and procedural characteristics, the authors found that the relative risks for the 30-day and five-year primary composite endpoint of death, myocardial infarction or stroke were similar after PCI versus CABG, irrespective of geography. However, the five-year rates of ischaemia-driven revascularisation after PCI were significantly higher in North American centres than in the European ones. Why the latter difference exists needs further study. This article is accompanied by an editorial by Seung-Jung Park and Duk-Woo Park.
Using data from the SWEDEHEART registry, authors Troels Yndigegn, Moman A. Mohammad and colleagues examined whether early discharge of low-risk ST-elevation myocardial infarction (STEMI) patients who had been treated with PCI is associated with adverse outcomes. They found no increase in major adverse cardiovascular events at one year for low-risk STEMI patients, which could lead to a protocol ensuring patient safety while reducing hospital time and thus allow for a more efficient use of available coronary care resources.
Szymon Darocha, Marcin Kurzyna and colleagues used a prospective, multicentre registry to examine the safety and efficacy of balloon pulmonary angioplasty (BPA) for treating adult and paediatric patients with chronic thromboembolic pulmonary hypertension (CTEPH) who are ineligible for pulmonary endarterectomy. With a high overall survival rate and significant improvement in haemodynamic, functional, and biochemical parameters three years after BPA, this could prove to be a useful treatment for CTEPH. This article is accompanied by an editorial by Francesco Saia.
Qi Guo, Changsheng Ma and colleagues describe the sequential technique of transseptal puncture during catheter ablation used in atrial fibrillation patients who have previously been treated for the closure of an atrial septal defect with an atrial septal occluder. They concluded that this technique can be used safely, facilitating transseptal puncture and atrial fibrillation catheter ablation in patients with atrial septal defect closure devices.
As mentioned above, this is the 200th issue of EuroIntervention. To mark this milestone in our publishing career we have invited my predecessor and the founding Editor-in-Chief of the Journal, Patrick W. Serruys to recount his own history of EuroIntervention. We also asked the joint Chairs of PCR, Jean Fajadet and William Wijns, who run our annual meeting EuroPCR, to speak about the Journal from their very special vantage point.
Let’s begin.
Supplementary data
To read the full content of this article, please download the PDF.