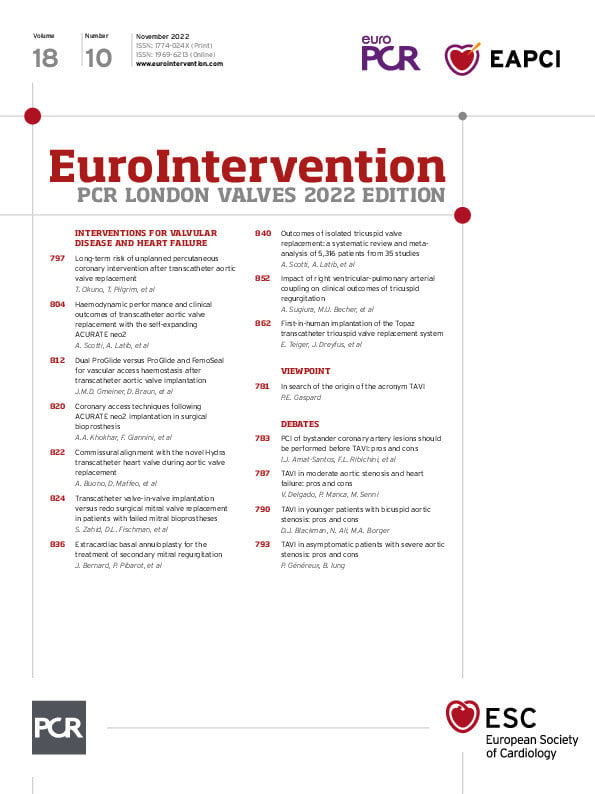
The fall meeting season continues with the traditional PCR London Valves. This annual meeting has been reinventing itself year after year without ever losing sight of the ingredients that made it successful to begin with. This year, the Course will do this by showing more cases than ever before.
In the words of the Course Directors, “this year the Main Arena will be filled with wall-to-wall LIVE cases from Copenhagen, London and Toulouse and Virtual LIVE recorded cases from Bern and Mainz. The first LIVE case on Monday will be featuring some ‘Wow cases’, showing how far we have come in the field in the past 20 years”.
In addition, there will be a daily Spotlight session in the Main Arena: Sunday will focus on “transcatheter aortic valve intervention as a mature procedure” with a discussion on the implications of lifelong management of younger and older patients. Monday will be dedicated to transcatheter mitral valve intervention: why it is progressing more slowly than expected, and what can we do? Tuesday will focus on the boom in and directions of transcatheter tricuspid valve intervention.
PCR London Valves is made up of a series of dedicated practical and livestreamed sessions that include aortic, mitral and tricuspid tracks. New this year, participants will also be able to follow three Simulation Lab Learning Pathways on transcatheter aortic valve implantation (TAVI) as well as simulations on mitral or tricuspid interventions. In step 1, participants will watch experts perform practical demonstrations in the Simulation Lab Learning Room; in step 2, participants will move on to the Hands-on Lab to practice what they have learnt in the Simulation Lab Learning Room; in step 3, participants move on to the Training Village for more device-specific training on what they have just learnt. What a journey!
And, of course, let’s not forget the daily late breaking trial sessions (with one co-hosted by EuroIntervention), the interactive case corners, the abstract corner, the sessions dedicated to nurses and allied professionals, the Innovation Hub, the Fellows Course, and so much more. Did I forget anything? Why yes, of course, EuroIntervention. As this issue coincides with PCR London Valves, it is entirely dedicated to valves and structural intervention, so now let me introduce exactly what we have here.
We begin with an intriguing series of debates touching on key topics at PCR London Valves. In the first, Ignacio J. Amat-Santos and Sara Blasco-Turrión vs Flavio L. Ribichini and Valeria Ferrero debate the question of whether percutaneous coronary interventions (PCI) of bystander coronary artery lesions should be performed before TAVI. In the second debate, the question of whether you should perform TAVI in patients with moderate aortic stenosis and heart failure is discussed by Victoria Delgado, Paolo Manca and Michele Senni. TAVI in younger patients with bicuspid aortic stenosis? Join Daniel J. Blackman, Noman Ali and Michael A. Borger for the third debate to see what they think about this question and, in the final debate, Philippe Généreux and Bernard Iung argue whether TAVI makes sense in asymptomatic patients with severe aortic stenosis.
The challenge of coronary access after TAVI is at the centre of the first of our clinical articles in which authors Taishi Okuno, Thomas Pilgrim and colleagues explore the incidence, characteristics, and predictors of unplanned PCI. They noted that patients with coronary artery disease (CAD) at the time of TAVI were more at risk of unplanned PCI than those patients without acute coronary syndromes and that the number of diseased vessels, male sex, and younger age were independently associated with an increased risk of unplanned PCI. They suggest that an assessment of CAD at the time of TAVI is thus critical in planning the long-term management of these patients.
The use of the first iteration of the ACURATE neo in TAVI was associated with a significant incidence of paravalvular aortic regurgitation with an adverse prognostic impact. But what about the new-generation ACURATE neo2, what improvements can be seen with this latest device? This is the subject of the next article by Andrea Scotti, Azeem Latib and colleagues who looked at the results of patients enrolled in the NEOPRO and NEOPRO2 registries undergoing TAVI with the ACURATE neo and neo2 devices. The ACURATE neo2 was seen to have lower rates of moderate or severe paravalvular aortic regurgitation, even in the presence of heavy aortic valve calcifications. There was also no increase in the need for pacemaker implantation. Further studies are needed, but this shows clear improvements for the new platform.
Jonas M.D. Gmeiner, Daniel Braun and colleagues compare two different percutaneous vascular closure strategies in the next article which looks at a dual ProGlide strategy versus a combination of one ProGlide and one FemoSeal after large-bore arteriotomy for TAVI. Patents treated with the combination strategy had less access-related vascular complications and bleeding than the dual ProGlide group leading the authors to conclude that a combined suture- and plug-based strategy might be the best approach to take.
What is the best strategy to take in patients with degenerated mitral bioprostheses: valve-in-valve transcatheter mitral valve replacement (ViV-TMVR) or redo surgical mitral valve replacement (redo-SMVR)? This was the question asked by Salman Zahid, David L. Fischman and colleagues who used the American Nationwide Readmission Database to evaluate in-hospital and short-term outcomes of ViV-TMVR compared with redo-SMVR. While ViV-TMVR patients were older and had a higher burden of comorbidities, ViV-TMVR still had lower odds of in-hospital mortality, complications, and resource utilisation. In terms of mortality at 30-days and six-months, no difference was observed between the ViV-TMVR and redo-SMVR groups which supports the safety and efficacy of ViV-TMVR when surgery would be too risky.
Jérémy Bernard, Philippe Pibarot and colleagues provide us with a research correspondence on the treatment of secondary mitral regurgitation (MR) in patients with heart failure. As we know, this is critical as it represents a marker of increased mortality and rehospitalisation, yet the recommended approach through mitral annuloplasty remains complex and can increase the risk of perioperative complications. Here the authors evaluated the safety and efficacy of a novel technique for managing secondary MR in patients with systolic heart failure, extracardiac annuloplasty using the BACE (Basal Annuloplasty of the Cardia Externally) device. In this pilot study, its use proved to be safe and feasible, reducing secondary MR resulting in positive left ventricular remodelling, and improvement in the patient’s quality of life and functional status. Controlled trials are warranted.
The next article, a meta-analysis, takes an “historic” approach studying data from surgical tricuspid valve replacement studies as a basis for evaluating the emerging therapeutic option of transcatheter tricuspid valve replacement (TTVR) for the management of secondary tricuspid regurgitation. Authors Andrea Scotti, Azeem Latib and colleagues believe that results from this type of analysis can play a critical role in clinical decision making for tricuspid valve replacement. These data can be seen as representing a benchmark for newer approaches to tricuspid regurgitation and can be useful in judging the durability of emerging bioprosthetic devices.
Atsushi Sugiura, Marc Ulrich Becher and colleagues investigate the impact of right ventricular-pulmonary artery (RV-PA) coupling on clinical outcomes in the treatment of tricuspid regurgitation (TR) in patients undergoing mitral transcatheter edge-to-edge repair (TEER). By dividing the tricuspid annular plane systolic excursion (TAPSE) by the pulmonary artery systolic pressure (PASP), they determined a ratio of this coupling. They then show that this ratio affects the outcome of TR in patients undergoing mitral TEER. This offers a new framework for determining the clinical relevance of TR to its severity and concomitant RV-PA coupling ratio.
In the continued evolution of managing severe tricuspid regurgitation, Emmanuel Teiger, Julien Dreyfus and colleagues discuss the first-in-human implantation of the new Topaz tricuspid valve for TTVR. With short term clinical improvement in TR, the novel device featured in this research correspondence shows promise for future use of TTVR when TEER is not possible for anatomical reasons.
Finally, do you say “TAVI” or “TAVR”? And if “TAVI”, why?
What better moment than in this issue, dedicated to PCR London Valves, to have this fascinating viewpoint by Philippe E. Gaspard. Where does the term “TAVI” come from? And how and why might you choose, instead, to “TAVR”. Let’s begin.