Abstract
Aims: To assess the clinical outcomes of patients where drug eluting stents (DES) were restricted to those at highest risks of restenosis, we compared three different strategies for stent implantation: bare metal stents (BMS) only, DES only and a group where DES use was restricted (RES).
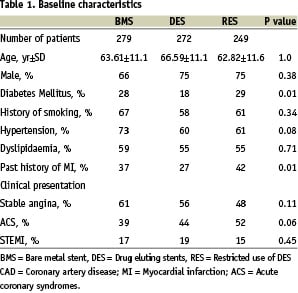
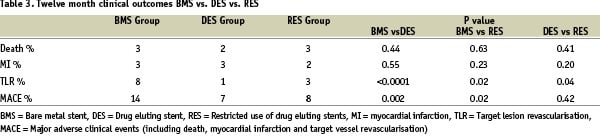
Method and results: Initial comparison was made between BMS only (279 patients, 316 lesions) and DES only (272 patients, 302 lesions). The endpoints of death, non-fatal myocardial infarction and target lesion revascularisation (TLR) [MACE] were assessed at 12 months. The incidence of MACE in the BMS only and DES only groups were 14% and 7% (p=0.002) and TLR was 8% and 1% (p<0.0001). Comparison was then made between these results and a third group where DES was restricted to patients at highest risk of restenosis. The restricted group (RES) comprised 249 patients (271 lesions) of which 53% received DES. RES remained significantly better than BMS, MACE (14% vs. 8%, p=0.02) and TLR (8% vs. 3%, p=0.02). When RES was compared with DES only, there was no significant difference in MACE (8% vs. 7% p=0.42), but there was a significantly lower TLR rate in the DES only group (1% vs. 3% p=0.04).
Conclusions: The overall incidence of events in patients where DES use was restricted to 53% of patients remains low and this may be an acceptable treatment strategy to reduce costs.
Introduction
Drug eluting stents (DES) have resulted in improved clinical outcomes for patients undergoing percutaneous coronary interventions (PCI)1. Several randomised controlled trials have shown the superiority of DES over bare metal stents (BMS)2,3. The improved outcome has occurred with reduced rates of restenosis and requirement for repeat target lesion revascularisation (TLR). The benefit is greater in patients with characteristics that are known to increase the risk of restenosis. Some patients achieve excellent results with BMS alone4-6 and the challenge is to identify those patients where DES offers the greatest advantage.
DES is significantly more expensive than BMS and economic constraints may limit the non-selective use of this new technology, particularly in the absence of proven cost effectiveness7,8. The low restenosis rates associated with DES will encourage the treatment of a broader spectrum of coronary artery disease, adding to the rising numbers of procedures in a growing and aging population9. The ideal would be to apply this more expensive treatment option to those who will achieve the greatest benefit.
We examined the hypothesis that restricting the use of DES in native coronary arteries to patients at highest risk of restenosis could achieve similar clinical outcomes to using DES in all.
Methodology
Patient population
To assess the clinical efficacy of restricting the availability of DES, three patient cohorts were studied and their outcomes compared. Each group consisted of consecutive patients who underwent stent implantation in native coronary arteries. All three groups were heterogeneous in terms of clinical presentation and included patients presenting with acute myocardial infarction.
Initial comparison was made between two patients groups who received either BMS exclusively or DES exclusively. The BMS group comprised 279 patients (316 lesions) who underwent PCI with stent implantation between August, 2002 and June, 2003 in a publicly funded hospital. DES was not available in this hospital during the initial study period due to economic constraints. The DES group consisted of 272 patients (302 lesions) who all received Sirolimus-eluting stents (Cypher, Cordis, Johnson and Johnson) during the same period in an adjoining institution where DES use was not restricted. The adjoining institution was attended by the same physicians. Access to DES was not restricted and utilisation was high. This fortuitously allowed the simultaneous comparison of like procedures with stent type being the major variable.
Subsequently the publicly funded hospital allowed restricted use of DES and this experience comprised the restricted DES (RES) group. The RES group consisted of 249 patients (271 lesions) who underwent PCI between February, 2004 and October, 2004 and were selected for DES by criteria that identified those at highest risk of restenosis. In this group, DES was used in 53% of patients and BMS in 47%. The BMS only and DES only results from the initial study were used as historical controls.
Criteria for selecting drug-eluting stents
The patients selected for DES in the RES group were determined by criteria that predicted a higher risk of restenosis and likely benefit from DES10-17. Patients were eligible for DES if they met at least one of the following criteria: (i) diabetes requiring medication; (ii) stent length > 20 mm; (iii) reference vessel diameter <2.5 mm; (iv) bifurcation lesions; (v) chronic totals occlusions; (vi) in-stent restenosis; (vii) ostial lesions.
Procedures
The same operators worked in both institutions and procedures were performed using standard techniques. Patients were given weight-adjusted heparin (100U/kg) prior to the procedure and maintained on dual antiplatelet therapy unless contra-indicated. Glycoprotein IIb-IIIa inhibitors were administered at the operator’s discretion, but were not used routinely. Patients receiving BMS were given clopidogrel for 1 month and those undergoing DES implantation were maintained on dual antiplatelet therapy for 12 months. Procedural success was defined as a residual stenosis < 50% with TIMI 3 flow.
Repeat angiography was not routinely performed and was only undertaken when indicated by recurrent symptoms or by demonstrable ischaemia on functional testing.
Data collection
Demographic and procedural data was obtained from the hospital database collected prospectively at the time of PCI. Clinical follow-up was performed at 12 months by telephone interview. The study was approved by the ethics committees of both hospitals. The clinical notes and procedural reports were reviewed for all reported major adverse clinical events (MACE).
Definitions and outcomes
The primary endpoint was the occurrence of MACE at 12 month follow-up, including in-hospital events. This included death, non-fatal myocardial infarction (MI) and target lesion revascularisation (TLR). Death included all cause mortality. MI was defined as a rise in creatinine kinase of more than twice the upper limit of normal. TLR was defined as a repeat intervention to treat a luminal stenosis within 5mm of the stent edges for recurrence of symptoms or demonstrable ischaemia on functional testing. Stent diameter was used as a surrogate measure of vessel diameter. No quantitative coronary angiography was performed.
Statistics
Epidemiological data was primarily analysed comparing the three groups together, using the 1-way ANOVA (continuous) or chi-squared (categorical) data. As indicated by the Chi values in Table 1, significant differences were identified for some of the epidemiological variables (ie Diabetes and Past history of MI).
Logistic multivariate regression was then used to confirm that these differences did not cause a material impact on the clinical outcomes and thus support the findings from the ANOVA/chi-squared analyses.
Clinical outcomes (Death, MI, TLR and MACE) were analysed using the Fisher exact test, which was appropriate for the small frequencies of the outcomes for each test condition. The resultant p-values (Table 3) were assessed according to the 95% confidence-interval.
P-values <0.05 were considered statistically significant for differences between treatment conditions.
Results
Baseline and procedural characteristics
Baseline demographic and procedural characteristics were comparable among the three groups for known predictors of restenosis with the exception of diabetes (Tables 1 and 2.).
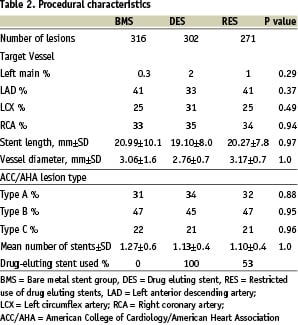
Diabetes was less prevalent in the DES only group. A significant difference was noted in the incidence of prior myocardial infarction. The number of patients presenting with acute coronary syndromes were comparable between the three groups. Multivessel PCI, accounting for the difference between patient and lesion numbers, was performed as staged procedures in most instances. Stent length, vessel diameter and number of stents per case were comparable between the three groups. 63% of patients in the RES cohort met criteria for DES use but only 53% received DES. This was largely due to clinical factors precluding DES use such as the need for imminent non cardiac surgery, deliverability and availability.
Clinical outcomes
Clinical follow-up was undertaken at 12-months in 86% of patients. Initial comparison was made between the BMS only and DES only strategies (Table 3). The primary outcome of MACE was significantly higher in the BMS only group than in the DES only groups (14% vs. 7%, p= 0.002, Figure 1).
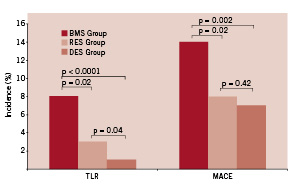
Figure 1. Twelve month clinical outcome of BMS vs. RES vs. DES. BMS = Bare metal stent, DES = Drug eluting stent, RES = Restricted use of drug eluting stents, TLR = Target lesion revascularisation, MACE = Major adverse clinical events (including death, myocardial infarction and target vessel revascularisation)
While there was no difference in death (3% vs. 2%, p=0.44) or MI (3% vs. 3%, p=0.55) between the two groups, there was a significantly lower incidence of TLR in the DES only group (8 % vs. 1%, p<0.0001, Figure 1).
The third treatment strategy, where DES use was restricted to those at highest risk of restenosis was then assessed and their outcomes compared with BMS only and DES only, using the results from this study as historical controls. A comparison between BMS only and restricted DES use (Table 3) showed a significant difference in MACE (14% vs. 8%, p=0.02) and TLR rates (8% vs. 3%, p=0.02, Figure 1).
Comparison was then made between the DES only group and the restricted DES group (Table 3). While there was no significant difference in MACE (7% vs. 8%, p=0.42), death (2% vs. 3%, p=0.41) or MI (3% vs. 2%, p=0.20), there was a significantly lower incidence of TLR in the DES only group (1% vs. 3%, p=0.04, Figure 1).
Discussion
This study examined the outcome of three different strategies of stent usage, BMS only, DES only, and a mixture of DES and BMS where the use of DES was restricted to patients selected because they were at highest risk of restenosis (RES group). We initially compared BMS only with DES only and confirmed the expected result that DES were superior to BMS. We then assessed a third group of patients where DES use was restricted to those at higher risk of restenosis. We found 53% of the patients met criteria and received DES, and compared the results of these patients with the results of the BMS only and DES only groups used as historical controls. The incidence of MACE in our BMS only and DES only arms were consistent with data published from the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) registry18. We found that restricted use of DES in only 53% of patients resulted in a superior outcome when compared to patients where BMS only was used, with lower MACE and TLR rates. When comparison was made between the restricted strategy and patients who received DES exclusively, no difference in MACE, death or MI rates was observed, but there was a significantly lower incidence of TLR in the group who received DES exclusively. The restricted group had 53% DES usage, a reduction of nearly half, which would result in significant cost savings at the time of the procedure. The three patient groups were well matched with the exception of diabetes, which was less prevalent in the DES only group, a finding that may bias the result in favor of DES only having a superior outcome.
This study tested the hypothesis that restricting the use of DES in native coronary arteries to patients at highest risk for restenosis would not compromise their clinical outcome when compared with patients who received DES exclusively. We chose the patients who selectively received DES (RES group) on the basis of characteristics that identified those most prone to restenosis. Diabetic patients, long lesions and small vessel size have an increased incidence of restenosis4-6. Other patient subgroups selected for high risk of restenosis included cases with complex anatomy (bifurcation and ostial lesions), chronic total occlusion and in-stent restenosis12-14.
Guidelines for DES usage from the European Society of Cardiology have also identified these groups as high risk and appropriate for DES19. We excluded patients at low risk of restenosis, such as those identified by Ellis et al with low risk of restenosis (4-10%) after undergoing BMS implantation20. These included non-diabetics, vessel diameter >3.5 mm and lesion length <10 mm.
The widespread use of stents in PCI has resulted in significantly better outcomes than balloon angioplasty, but in-stent restenosis and the requirement for repeat revascularisation have been a major limitation in the BMS era21. The application of DES technology has produced significant reductions in restenosis in randomised controlled trials1-3 and as a result a broader spectrum of coronary artery disease is now amenable to PCI. This is increasing the number of procedures performed and also the numbers of stents used per patient9.
Currently there is a threefold cost differential between DES and BMS and this difference is likely to remain despite the anticipated decline in the cost of each. Increased utilisation of DES results in a significant upfront increase in health care costs. Whilst the higher cost will be somewhat offset by a reduction in the need for repeat revascularisation procedures, unequivocal evidence of the cost effectiveness of non-selective DES use has not yet been produced22. Greenberg et al have suggested that the restricted use of DES may well be cost effective when applied to patients at high risk of restenosis23.
The results of the patient group that selectively received DES on the basis of criteria that identified those at highest risk of restenosis remains very good and is superior to BMS alone. The exclusive use of DES seems to have advantages in lower TLR rates, but in our study did not impact significantly on MACE rates. Whether this difference justifies the cost will be determined by larger studies and health economists.
The indiscriminate use of DES would result in unnecessary costs if there were no advantages to this strategy. Rationalising the use of this therapy is a desirable outcome but should not compromise clinical outcomes. As patients become aware of the clinical superiority of DES, their expectation of being offered the technology increases. Concerns about DES have arisen with the finding of late occlusive stent thrombosis in some patients that can be unpredictable and catastrophic24,25. In this setting, criteria for selecting patients for DES implantation would be a helpful aid to physicians to identify those patients most appropriate for their use.
This study has the inherent limitations of an observational study and is subject to recall bias. The small sample size may have not have allowed a true difference in MACE, death and MI rates between DES only (DES) and restricted DES use (RES) strategies to be detected.
The authors acknowledge the follow-up rate of 86% is a further significant limitation of the study. Our findings require validation by larger clinical trials that will identify with greater accuracy the patient subgroups that will benefit most from DES implantation.
These results suggest that the selective application of DES to patients who are most likely to benefit from the technology does not greatly compromise clinical outcome, while limiting use by nearly 50%. This suggests a possible more cost effective approach to the use of this expensive technology and would thus have implications for health care expenditure. Physicians will increasingly find that their clinical choices are constrained by economic factors and we need to identify areas where cost saving may reasonably be achieved without detriment to our patients.
Acknowledgments
We acknowledge our colleagues Drs. Black and Eccleston who performed some of the procedures. We are indebted to Dr. Peter Valentine for establishing the database in 1981 and encouraging our interest in research and to the Department of Epidemiology at Monash University.

