Abstract
Aims: A variety of endovascular technologies for valve repair for mitral regurgitation (MR) are under development. Endovascular Edge-to-Edge (E2E) approach recently entered the clinical trial phase. The aim of the present study was to determine the effectiveness of surgical isolated E2E repair without annuloplasty to predict the efficacy of the endovascular E2E approach.
Methods and results: Clinical and echocardiographic data of 29 patients with either degenerative or functional MR who had surgical E2E repair without annuloplasty, were retrospectively analysed. Mean age was 63.8±8.79 years, 45% were in NYHA class III or IV and 41% had a left ventricular ejection fraction less than 60%. Hospital mortality was 3.4% and overall survival after a mean follow-up of 6.8 year was 93%. At latest follow-up, 68% of patients were in NYHA class I, 28% in class II and 4% in class III; 86% of patients had MR < grade 2. Two patients with recurrent grade 4 MR underwent re-operation. The 5 years freedom from the combined end-point of recurrent MR>2+ and re-operation, was 90±5%.
Conclusions: Isolated surgical E2E mitral repair, intentionally performed without annuloplasty, has acceptable midterm results for degenerative and functional MR, comparable to conventional repair techniques with annuloplasty. These results encourage the evaluation of less invasive endovascular E2E repair approaches in a clinical setting.
Introduction
While surgical repair is effective for many patients with mitral regurgitation (MR) of different etiology and while clinical results have improved significantly over the years, the morbidity and mortality continue to be significant and limit its application. This is especially important for the patient with early disease and for the patient at higher surgical risk. The search for a therapy with an improved risk benefit ratio compared to contemporary therapy has led to the development of endovascular approaches.
In contemporary open heart surgery, the edge-to-edge (E2E) technique is one of the accepted repair techniques used to correct MR of various etiology by suture approximation of the edges of two opposing leaflet scallops at the site of regurgitation (Figures 1 and 2).
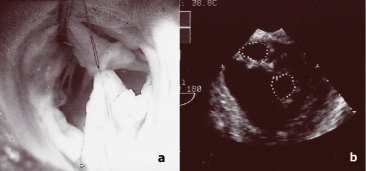
Figure 1. a. Intra-operative, surgical view from the left atriotomy. A 4-0 polypropylene suture has been used for E2E leaflet approximation in the middle portion of the valve. The two orifices are shown. b. Post-repair diastolic echo image in the transgastric short-axis TEE view. The two orifices are outlined by the dotted lines.
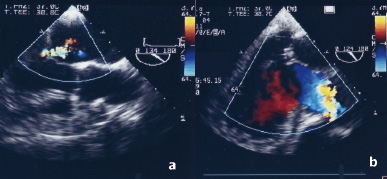
Figure 2. a. Preoperative transoesophageal echocardiography, two-chamber view, showing central mitral regurgitation due to restricted leaflet motion of both leaflets in a patient with ischaemic cardiomyopathy. b. Post-repair transoesophageal echocardiography image in the same view, demonstrating valve competence following the isolated edge-to-edge repair.
When the approximating suture is placed near the center, the repair creates a valve with a double orifice during diastole1. This technique, often used with ring annuloplasty, offers an expedited and simple method to treat mitral regurgitation caused by the most common etiologies (myxomatous degeneration, fibroelastic deficiency, ischaemic and idiopathic cardiomyopathy, rheumatic disease and endocarditis) and resulting from different mechanisms.
Operative results and follow-up data have been previously reported by several groups, documenting the safety, effectiveness and durability of the E2E repair, even for complex pathologies, including when E2E was used as the sole repair technique (Isolated E2E Repair)2,3.
The technical simplicity of the principle of leaflet approximation offers an opportunity to correct MR with devices in the closed and fully functional heart – without the aid of cardiopulmonary bypass – under echocardiographic and fluoroscopic guidance. The feasibility of the E2E technique in the closed beating heart through a left thoracotomy has been shown experimentally and, endovascular E2E repair was successfully carried out in pigs and sheep4,5. Initial clinical experience with a clip device (E-Valve, Redwood city, CA) has been recently reported6, and a suction and suture device (Edwards Lifesciences, Irvine, CA) is going to reach clinical application soon. Due to regulatory constraints, the initial experience with these devices will require an isolated implant without the addition of an annuloplasty device, differently from the habitual surgical combination.
To determine the potential clinical value of an endovascular E2E approach without annuloplasty, an understanding of the effectiveness of the surgical analogue is critically important. The subject of this retrospective report is the mid-term follow-up in a group of patients in whom degenerative or functional MR was surgically corrected, intentionally using the E2E technique as the sole leaflet repair technique, with central placement of the approximating suture and intentionally performed without annuloplasty.
Methods
From November 1993 through December 2001, 29 patients with central E2E repair in whom an annuloplasty was intentionally avoided, because annular anatomy and function were considered relatively preserved (limited annular dilatation and distortion) were retrospectively reviewed. These patients are a subgroup of a previously published cohort of patients2. Exclusion criteria for this analysis included: presence of annular calcification contraindicating annuloplasty, a minimally invasive robotic approach, an aetiology other than degenerative or functional, E2E repair used as a rescue procedure following a failed repair and concomitant other leaflet repair techniques. The study group represents a relatively homogeneous group of 29 patients who had E2E repair without annuloplasty to correct either degenerative or functional mitral regurgitation. There were 11 (38%) females and 18 (62%) males, with a mean age of 63.8±8.79 years. At admission, 13 patients (45%) were in New York Heart Association functional class III or IV, while 16 patients (55%) were in class I or II. Twelve patients (41%) had a left ventricular ejection fraction less than 60%. Twenty-four patients (83%) were in sinus rhythm and 5 patients had chronic atrial fibrillation. Degenerative disease with prolapse and/or flail was the cause of MR in 22 patients (76%). Nine patients had fibroelastic deficiency and 13 patients myxomatous disease. Seven patients (24%) had functional mitral regurgitation with restricted leaflet motion (ischaemic in 6 patients and secondary to idiopathic cardiomyopathy in one).
Preoperative assessment of mitral valve anatomy and function was performed by transoesophageal echo-Doppler examination (TEE) the day before the operation in all patients. Mitral regurgitation degree was determined by means of a combination of Colour Doppler (Colour flow jet area and vena contracta width) and pulmonary vein flow analysis. Mitral regurgitation (MR) was severe in most patients, with a mean grade of 3.5±0.56. In all cases colour Doppler examination showed a non-commissural MR origin. Both leaflets were involved in 14 patients, while single leaflet lesions were present in the remaining 15 patients (8 posterior leaflet lesions and 7 anterior leaflet lesions). Associated co-morbidities included: coronary artery disease in 10, left ventricular aneurysm in 3, aortic valve disease in 2, an ascending aorta aneurysm in 1, a patent foramen ovale in 1. One patient had previous coronary artery bypass surgery.
The surgical technique has been described in previous reports7-9. The approach to the valve was through a standard left atrial incision in 24 patients and through an aortotomy or left ventriculotomy in the remaining 5 patients. Valve inspection and segmental analysis was carried out in standard fashion. The E2E leaflet repair technique was selected because more conventional repair techniques were considered either not suitable or anticipated to be associated with a high risk of failure. The decision not to use an annuloplasty was based on direct inspection of the valve and on pre-operative echocardiographic evaluation of annular function and geometry. Repair was performed by suturing the mid-portion of the free edge of the middle leaflet scallops. A 4-0 polypropylene continuous suture without pledgets was used in most cases for leaflet approximation. After discontinuation of cardiopulmonary bypass, valve function and anatomy were assessed by intra-operative TEE.
A number of concomitant procedures were performed, including: coronary artery revascularisation (9 patients), aortic valve replacement (2 patients), left ventricular restoration (3 patients), radiofrequency ablation of atrial fibrillation (1 patients), Bentall procedure (1 patient), patent foramen ovale closure (1 patient).
All surviving patients had at least 3 year follow-up. Mean follow-up time was 6.6±2.1 years (maximum 12 years). Follow-up was completed in all patients (100%).
Data collection
In-hospital data was retrospectively collected through the hospital database and patients records. Follow-up data was obtained by outpatient visit, including TEE examination in 10 patients and by telephone interview with the patients and referring cardiologists in the remaining patients, collecting the latest echocardiographic findings. Last follow-up information was collected in February, 2006. Postoperative TEE examination focused on the presence and degree of residual MR (determined by means of a combination of Colour Doppler and pulmonary vein flow analysis) and on evaluation of mitral valve area (planimetry and Doppler-derived). Residual mitral stenosis was defined as the presence of a mean gradient higher than 5 mmHg or a valve area smaller than 2.5 cm2 (by planimetry in the short axis transgastric view).
Results
Hospital mortality was 3.4% (one patient with functional MR died within 30 days due to postoperative, low-cardiac output syndrome and multi-organ failure). Postoperative course was complicated in 9 patients (31%). The most frequent complication was atrial fibrillation (5 patients) followed by low cardiac output syndrome (3 patients), respiratory failure, transient junctional rhythm, tamponade and minor TIA in the early postoperative period (1 patient). Overall survival at latest follow-up was 93% (27/29 patients). There was one late death (sudden death 4 years after the operation) in a patient with functional MR and left ventricular dysfunction. Cause of death in this patient was not related to recurrent MR (trivial at the last examination before death).
During the follow-up period, 7 patients (24%) required at least one hospital readmission (6 for cardiac reasons). The most frequent cause was atrial fibrillation requiring hospitalisation (3 patients). Two patients had uneventful mitral valve replacement 4 years after isolated E2E repair because of recurrent MR. There was one readmission for heart failure in a patient who had E2E repair and left ventricular restoration. One patient required hospitalisation for acute myocardial infarction and one for surgical treatment of an abdominal aorta aneurysm. Heart rhythm data at follow-up was available for 24 patients, 21 had sinus rhythm, and 3 had atrial fibrillation. At latest follow-up, 19 patients (68%) were in NYHA class I, 8 (28%) in class II and one (4%) in class III. No patients were in NYHA class IV. Compared with baseline, 86% of patients had improvement of at least one functional class (Figure 3).
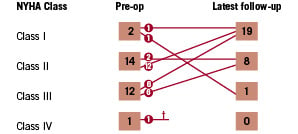
Figure 3. Pre- and post-procedural NYHA Class.
Echo-Doppler findings are listed in Figure 4.
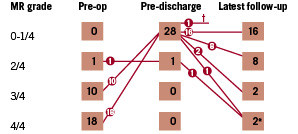
Figure 4. Pre- and post-repair mitral regurgitation (MR) grade.
At early post-operative assessment, 28 patients (97%) had at least a two grade MR reduction compared to baseline. In one patient (grade 2/4 ischaemic MR) MR was not reduced. In this case MR remained the same after repair and was stable during follow-up. The patient with the longest follow-up (12 years) showed trace MR at latest follow-up, similar to the pre-discharge MR severity. Compared with the pre-discharge echocardiographic examination, about one third of patients (11/28) showed a tendency of recurrence of MR over time. However, at latest follow-up only two patients (7%) had progressed to grade 3 MR and two (7%) to grade 4. The latter patients were re-operated. The two patients who had grade 3 MR at last follow-up, had concomitant left ventricular restoration at the time of E2E repair. At a median follow-up of 6.3 years, 86% (24/28) of patients were considered to have a successful or acceptable valve repair based on an MR grade < 2. Freedom from the combined end-point of re-operation and recurrence of MR>2+ was 90±5% at 5 years (Figure 5).
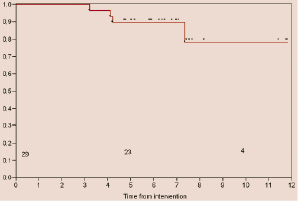
Figure 5. Freedom from re-operation and recurrence of MR>2+.
Discussion
In this retrospective analysis, 29 patients in whom annuloplasty was intentionally not added to isolated central E2E repair were followed using clinical and echocardiographic assessments. Patients with severe annular calcification were excluded because in this situation annuloplasty is technically very challenging or not feasible and therefore, was considered contraindicated10. The reason to exclude minimally invasive and robotic procedures is because those patients were part of the initial learning curve with such procedures. We also excluded patients with rheumatic valve disease, obstructive cardiomyopathy or endocarditis, in whom repair results would likely be influenced by the cause of the MR itself. Rheumatic patients have limited durability compared to patients with degenerative disease with any technique11. Patients whose valve was repaired using additional techniques (quadrangular resection and chordal implantation) were also excluded because of the difficulty in assessing the results of the E2E repair itself. For the same reason, patients were excluded if the E2E technique was used as a rescue following a failed conventional repair.
Patients continue to demand and search for less invasive approaches, not only because they desire reduced morbidity and mortality, but importantly also to improve what they consider to be important quality of life measures, which the medical community traditionally views more as safety related outcomes. These 29 surgical patients are the closest projection of candidates for intentional isolated, central E2E repair without annuloplasty, potentially treatable with an endovascular approach which is intended to create a similar area of leaflet coaptation (with one or more clips or sutures) in a similar position on the valve as with surgical E2E repair.
Because annuloplasty may increase durability of the repair, most surgical centres routinely perform annuloplasty. Annuloplasty is often added to stabilise the repair, even in the case of normal annular dimensions. Because morbidity and mortality of re-operation is substantially higher compared to those of a first operation, an annuloplasty may be added for this reason alone.
Similar to what has been reported for other commonly used repair techniques long-term results with surgical E2E repair have been most favourable when annuloplasty was performed as well1. Freedom from re-operation at 5 years was 92%±3.4% vs. 70%±15% in patients who received versus those who did not receive an annuloplasty, respectively. However, in multivariate analysis, the lack of annuloplasty was determined to not be a risk factor for re-operation. Considering the morbidity and mortality of re-operation, in patients with standard posterior leaflet degenerative MR, a freedom from re-operation of 70% at 5 years, would not be considered acceptable after surgical valve repair. It must however be noted, that a strong selection bias was present in that series of patients, specifically to offer them the known benefits of repair over valve replacement. In most of those cases a contraindication for annuloplasty was present, most frequently annular calcification. In the referenced series, the E2E technique was thus clearly used in patients with complex lesions such as anterior leaflet and bi-leaflet lesions, and restrictive leaflet motion caused by rheumatic or ischaemic disease, as well as patients with leaflet erosions due to active or healed endocarditis.
In the current series, where annuloplasty was intentionally avoided, results are satisfactory in spite of complex anatomy (e.g. 50% of patients had bi-leaflet lesions), with a 90±5% freedom from re-operation or recurrence of MR at 5 years. Durability of isolated E2E repair was particularly striking in some patients, as in the patient with the longest follow-up, whose early post-repair echocardiography showed mild regurgitation which stayed unchanged for at 12 years postoperatively. The vast majority of patients (86%) had MR < grade 2 at latest follow-up.
Most surgical reports of mitral valve repair measure clinical outcome based on in hospital mortality, long term survival and freedom from re-operation in survivors. Recurrence of MR is rarely reported in the surgical literature. Mitral regurgitation following repair was the subject of a recent investigation by Flameng et al in a series of 242 patients who underwent mitral repair with annuloplasty for degenerative disease (Table 1)12.
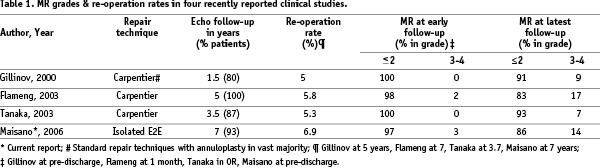
The linearised recurrence rate of non-trivial MR (>1/4) was 8.3% per year and of significant MR (grade 3/4) 3.7% per year. The authors suggested that recurrence of MR is more frequent when certain inadequate surgical techniques are used or when annuloplasty is not performed. However, recurrence of MR was shown to be partially independent from the repair technique and probably related to continued intrinsic degeneration of valve tissue, since even in absence of the above mentioned risk factors the linearised rate of recurrent MR grade 3-4 was 2.5% per year. Recurrence of significant MR after conventional repair with annuloplasty was also reported in a series of patients with primarily (73%) degenerative disease by Gillinov et al13. At a mean echocardiographic follow-up (in 80% of patients) of 18 months, 9% of patients had a MR grade 3/4, whereas immediately after surgery none of the patients has MR > grade 2 (Table 1). Tanaka et al also reported similar recurrence of MR in patients with isolated mitral valve repair with annuloplasty for myxomatous valve disease14.
The E2E repair is geometrically associated with a reduction of the effective orifice area of the mitral valve. However, no patient developed mitral stenosis. The healing process after leaflet approximation is also not associated with late development of stenosis9,15. Computer models showed that mitral valve haemodynamics were not influenced by the E2E repair and that diastolic flow velocity and pressure drops were not different to those observed in a single orifice valve with a surface area equal to the sum of the two areas of a double orifice mitral valve16. The E2E repaired mitral valve retains a functional reserve17. It has been demonstrated during exercise echocardiography that, as the cardiac output increases, the valve area increases accordingly, keeping the pressure gradients within normal limits and avoiding exercise-related pulmonary hypertension. Intra-operative assessments of valve area, under general anaesthesia, may lead to underestimations, because of haemodynamic conditions. The same findings have been described by Kinnaird et al in patients treated for functional mitral regurgitation18. These authors did not find significant mitral stenosis in a group of 17 patients with E2E repair and an undersized annuloplasty (using a small Duran ring size 25 or 27).
Limitations of the study
This study is based on a limited number of patients, retrospectively selected to focus specifically on patients who underwent central isolated central E2E mitral valve repair, intentionally without annuloplasty. They represent a minority of the population undergoing mitral repair at our institution: in the time frame of the study, edge-to-edge repair was performed in about 1/3 of the mitral repairs, and annuloplasty was not done in 20% of this subgroup of patients. The annuloplasty was usually avoided in patients undergoing complex procedures to shorten the operation time, and in patients with smaller annular dimensions. However the exact reason for avoiding annuloplasty was not available for all patients at the time of the data collection. Therefore selection biases could have affected the reported results.
Furthermore, several patients in the present series had concomitant procedures in addition to mitral repair which could have influenced the outcome. Finally, measurements of annular size, atrial and ventricular dimensions before and after treatment were not available to further analyse the efficacy of the selected treatment.
The lack of a core echocardiography lab and independent assessment are also a limitation of the present study.
Conclusions
The present study focused on patients who received isolated central E2E repair intentionally without annuloplasty. The findings in this report have proven the safety and the efficacy of this approach at midterm follow-up. The E2E repair has been widely applied and over 1000 patients have now been reported in the peer reviewed literature, with clinical demonstration of efficacy. It has been applied successfully in anterior leaflet disease, bi-leaflet disease in the context of the most severe forms of Barlow’s disease, in ischaemic and dilated cardiomyopathy, and in a variety of complex anatomical lesions including commissural prolapse, free margin healed endocarditis erosions and restricted leaflet motion1,3,8.
The reported results in this group of patients are acceptable at midterm follow-up and comparable to those reported by others using other surgical techniques in conjunction with annuloplasty.
Because of the potential risks of open heart surgery, patients referred to surgery are only a small subset of patients with mitral regurgitation. An endovascular approach will likely be very relevant for higher risk patients. The introduction of a non-invasive technique, if proven safe and effective may also result in a drastic revision of indications for correction of chronic MR, allowing earlier repair of failing mitral valves, before left ventricular remodelling and significant annular dysfunction occurs. Under such conditions, leaflet repair alone could potentially lead to better results than those obtained by current surgical approaches.

