Abstract
Aims: To determine whether women have an unfavorable outcome after coronary interventions compared with men, we evaluated patients undergoing revascularisation within the Arterial Revascularisation Therapies Study (ARTS).
Methods and results: We evaluated 1205 patients (23% women) with multivessel disease randomised to percutaneous or surgical coronary revascularisation. The in-hospital results, and clinical outcome at five years were evaluated. Women were older, with a higher prevalence of hypertension, hypercholesterolaemia, family history for coronary artery disease (all p<0.001), diabetes mellitus (p=0.05) and stable angina (p<0.05) than men, but had a lower incidence of history of myocardial infarction or smoking (both p<0.001). More major bleeding complications, even after adjusting for baseline clinical characteristics (OR 29.4, 95% CI: 5.3-500, p<0.005) were observed in women following percutaneous coronary intervention. During clinical follow-up freedom from major adverse cardiac and cerebrovascular events was similar in men and women, regardless of treatment strategy. Men assigned to bypass surgery had a better quality of life, but women reported more frequently angina.
Conclusion: The clinical outcome of women with multivessel disease undergoing coronary revascularisation was similar to that in men. However, women presented more bleeding complications before hospital discharge, and had less favourable assessment in specific domain of daily life at follow-up.
Introduction
Cardiovascular disease is the leading cause of death in both women and men. Although the number of cardiovascular deaths has declined in men, it has actually increased in women over the past decade. Previous studies reporting the outcome of coronary revascularisation performed with bypass surgery or percutaneous intervention have reported higher rates of mortality and major complications in women1-3. The reasons for this sex difference were attributed to a smaller surface area and smaller size of coronary arteries, advanced age, more risk factors (diabetes mellitus, arterial hypertension), greater burden of comorbidity, and more acute coronary artery disease at presentation in women4,5. However most of these studies were performed before the introduction of innovative transcatheter revascularisation techniques, such as coronary artery stenting. Furthermore, women are less likely to receive left internal mammary artery grafts and to achieve complete revascularisation.
The Arterial Revascularisation Therapies Study (ARTS) was designed to compare Coronary Artery Bypass Grafting (CABG) and Percutaneous Coronary Intervention combined with stent implantation (PCI) for the treatment of patients with multivessel disease6. Overall, at one year PCI is less expensive than CABG and offers the same degree of protection against death, stroke, and myocardial infarction, but is associated with a greater need for repeated revascularisation. At five years there was no difference in mortality between CABG and PCI, but major adverse cardiac and cerebrovascular events were higher in the PCI group, driven by the increased need for repeat revascularisation7. The aim of this study was to determine whether women enrolled in the ARTS study have an unfavourable in-hospital and long-term clinical outcome after PCI or CABG interventions compared with men.
Methods
Patients
Between April, 1997 and June, 1998, 1205 patients with multivessel disease were randomised to either CABG (n=605) or PCI (n=600). The protocol of this study has been previously described8. All patients had clinical follow-up visits including an ECG at one and six months, one, two, three and five years. Additional information was obtained by telephone interview or via the referring physician, when needed. An independent committee adjudicated clinical events and ECGs.
Euro-Qol questionnaire
Health related quality of life was assessed at one and six months, one, two, and three year clinical follow-up using the Euro-Qol questionnaire, which allows patients to grade their general health status9. The questionnaire includes a visual/analogue scale (Euro-Qol thermometer) for patients to use in rating their overall status from 0 (“worst” imaginable health) to 100 (“best” imaginable health). The questionnaire also comprises five items (mobility, self-help, usual activity, pain or discomfort, and anxiety or depression); these ratings were then summarised (Euro-Qol summary) after being weighted to account for differences in the importance of the various items to the patient.
Statistical analysis
Statistical analysis was performed with SAS 6.12 software (SAS Institute Inc., Chicago, Illinois). Data included baseline patients’ characteristics, information on coronary artery lesion characteristics, in-hospital results and outpatient clinical follow-up. The primary clinical analysis consisted of a comparison between the two groups according to gender. Categorical variables are presented as absolute numbers (percent) and were compared by the chi-square test or Fisher’s exact test as appropriated. Continuous data, expressed as mean ± SD, were compared with the Student’s t-test or Wilcoxon’s test. All analyses were based on per protocol principle. Event free survival rate was estimated by the Kaplan-Meier method, and differences were assessed by the log rank test. The test for proportionality showed that the hazard was non-proportional, so logistic regression instead of Cox regression was used. A series of univariable logistic regression models with in hospital outcome or major adverse cardiac and cerebrovascular events at five years as dependent variable and sex as the independent variable was used for estimation of the effect of gender. If the effect of gender was statistically significant, a multivariate logistic regression was undertaken with outcome as dependent variable and sex, diabetes, hypercholesterolaemia, hypertension, body mass index, family history, smoking, silent ischaemia, stable angina, previous myocardial infarction as independent variables. The coefficients of the terms for sex were used to calculate Odds Ratios (OR) and their 95% Confidence Intervals (CI) for in hospital outcome and five-year major adverse cardiac and cerebrovascular events of men compared to women. Statistical significance was considered at a p value <0.05 (2-tailed).
Results
Of the 1,205 randomised patients with multivessel disease, 283 (23%) were women (PCI: 138; CABG: 145) and 922 (77%) men (PCI: 462; CABG: 460).
Clinical and angiographic characteristics
The clinical and angiographic characteristics of the men and women are shown in Table 1.
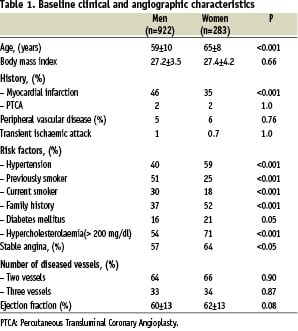
Women were older than men (p<0.001), and had a higher incidence of hypercholesterolaemia, hypertension, family history for coronary artery disease (all p<0.001), diabetes mellitus (p=0.05) and stable angina (p<0.05), but previous or current smoking and history of myocardial infarction were present in a lower rate (both p<0.001). Although women were shorter and weighed less, the body mass index was similar to that of men.
Procedural characteristics
In patients assigned to PCI there were no differences between men and women in the number of segments diseased, lesions treated, stents implanted/patient, or the duration of PCI procedure (Table 2).
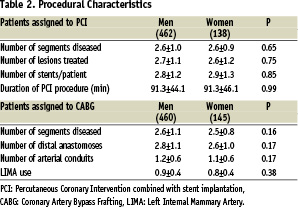
Similarly, in patients assigned to CABG the number of diseased segments, distal anastomoses, arterial conduits implanted, left internal mammary use, and the duration of surgical procedure were the same in men and women.
In-hospital outcome
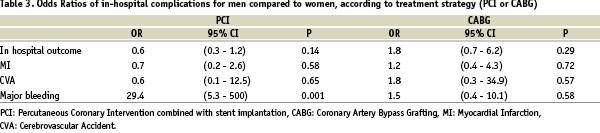
Women assigned to PCI had more bleeding complications than men (7.2% vs. 0.2%, p<0.001); however, no differences were observed in patients assigned to CABG treatment (2.8% in men vs. 1.4% in women, p=0.54). Bleeding complications remained higher in women even after adjusting for baseline clinical characteristics (OR 29.4, 95% CI 5.3 - 500, p<0.005). Sex adjusted OR for in hospital complications according to treatment strategy (PCI or CABG) is presented in Table 3.
Clinical follow-up
There was no effect of gender in the five-year’s clinical outcome, according to treatment strategy (Figure 1).
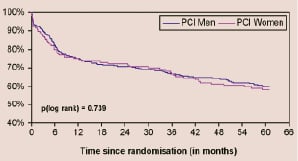
Figure 1 A. MACCE in PCI patients
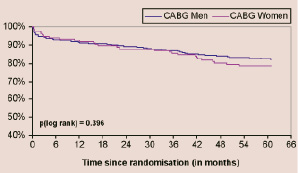
Figure 1 B. MACCE in CABG patients
Figure 1. Kaplan-Meier curves according to gender showing freedom from: (A) death/cerebrovascular accident/myocardial infarction or revascularisation in patients undergoing PCI; (B) death/cerebrovascular accident/myocardial infarction or revascularisation in patients undergoing CABG. PCI: percutaneous coronary intervention combined with stent implantation, CABG: coronary artery bypass grafting.
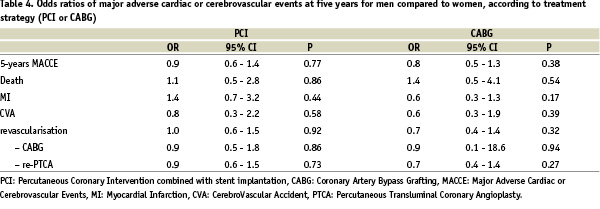
In patients assigned to CABG treatment the incidence of death was 10.1% in men and 7.2% in women (p= 0.48); in patients assigned to PCI 9.0% in men and 7.4% in women (p= 0.29). There were no differences in the incidence of major adverse cardiac and cerebrovascular events in men compared to women in patients assigned to CABG (OR 0.8, 95% CI 0.5-1.3, p= 0.38), or PCI (OR 0.9, 95% CI: 0.6 - 1.4, p=0.77). These results did not change when the hard end-points (death/myocardial infarction/cerebrovascular accident) were considered (CABG: OR 0.8, 95% CI 0.5-1.5, p= 0.57, PCI: OR 1.2, 95% CI 0.7-2.1, p= 0.57). However CABG was associated with a lower incidence of major adverse cardiac and cerebrovascular events at five years, compared to PCI in both sexes (p<0.005). The sex adjusted odds ratios for five years major adverse cardiac and cerebrovascular event, according to treatment strategy is presented in Table 4.
Anginal status
At five years follow-up in patients undergoing an initial strategy of CABG, 13% of men compared to 24% of women (p<0.01) reported angina symptoms; in patients assigned to PCI, there were no differences in the incidence of angina (21% of men compared to 23% of women p= 0.71).
Quality of life
There were some differences in quality of life at three years, as assessed by the self-rated Euro-Qol questionnaire, among men and women. Men showed better quality of life (higher score on the Euro-Qol thermometer) compared to women (p<0.05) and favourable assessment (lower score on the Euro-Qol domain) in specific items such as mobility (p<0.001), self-help (p<0.005) or usual activity (p<0.01). The differences in quality of life according to treatment strategy are shown in Table 5.
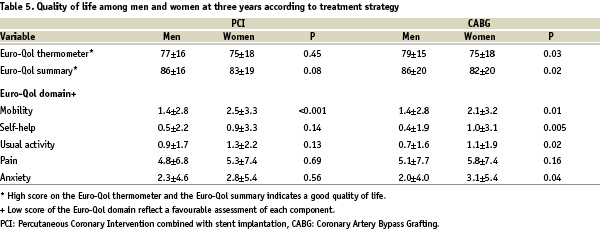
Men after CABG showed better quality of life and favourable assessment in specific domains such as “mobility” and “anxiety or depression” by three years. In patients allocated to PCI group the only difference was a favourable mobility in men compared to women.
Discussion
In the present study we analysed the in-hospital, and five-year clinical outcome, according to gender, in a large series of patients with multivessel disease undergoing after randomisation, PCI or CABG procedures in native coronary artery lesions. Women were older, had more risk factors for coronary artery disease, and were on stable angina; conversely, men had a higher incidence of history of myocardial infarction. Bleeding complications were significantly higher in women post-PCI (even after adjusting for baseline clinical characteristics), but there was no effect of gender at five year’s major adverse cardiac and cerebrovascular events independent of treatment strategy. In patients assigned to CABG women reported angina more frequently during follow-up and men had a better quality of life, as expressed by Euro-Qol questionnaire.
Gender and PCI
A number of previous studies have examined the influence of gender on in-hospital outcomes after PCI. Overall, these studies have shown higher in-hospital mortality in women than in men, especially in earlier series10-12. The higher incidence of in-hospital complications could be related to the fact that women were older, have smaller body mass index, and had higher prevalence of other co-morbid conditions. More recent studies have reported improved clinical outcomes for women who underwent elective PCI3,13, due to advances in technology and improvement in revascularisation techniques.
Although the mortalty difference between men and women was attenuated after accounting for differences in baseline clinical characteristics, gender remained an important risk factor for vascular complications. Previous studies have shown that women had more bleeding complications, mainly at the access site when anticoagulation was used14. The excess vascular complications among women, however, may represent a clinically modifiable risk; careful attention to sheath size, heparin dosing, and rapid sheath removal have been demonstrated to lower risks of vascular complications15.
The influence of gender on long-term clinical outcome following PCI has not been adequately assessed in previous studies. A pooled analysis of seven prospective stent trials including 7,171 patients (2,179 women and 4,992 men) with systematic angiographic and clinical follow-up demonstrated no differences in target vessel revascularisation one year after bare-metal stenting between men and women16. In the Dynamic Registry3 one-year mortality and combined end-point of death/myocardial infarction/CABG were higher in women than in men; however after controlling for other risk factors, gender was not a significant predictor of death or death plus myocardial infarction at one year. Very recently, Lansky et al17 reported higher unadjusted one-year rates of target vessel revascularisation in women compared to men treated with the paclitaxel-eluting stent in the TAXUS-IV trial, but in multivariate analysis, gender was not an independent predictor of revascularisation.
Gender and CABG
The frequency of CABG performed in women has increased over the past decade in association with a gradual ageing of the surgical population18. Many studies examining gender differences outcomes after CABG report a higher unadjusted post-operative mortality and morbidity for women compared with men. Edwards et al19 analysed the data from the Society of Thoracic Surgeons National Cardiac Surgery database; they reported that women were older, presented more commonly for non-elective procedures, and had a higher prevalence of pre-operative comorbid conditions, such as diabetes, hypertension, and peripheral vascular disease. Guru et al20 reported that women had a higher early mortality even in the current era with improved surgical techniques. Very recently Huynh et al21 presented the results of the ROSETTA-CABG registry, with one-year clinical follow-up; women had a nearly three times greater probability than men to present a composite clinical event (death, non-fatal myocardial infarction, or unstable angina), and four times to require PCI during follow-up. However female gender was not independently associated with adverse cardiac outcomes by multivariate regression analysis. In another study20 the risk-adjusted survival of women was worse than that of men in the first year after CABG, but their long-term mortality was similar to that of men. It has been reported that left internal mammary artery use and multiple arterial grafts were less frequently used in women during CABG19,22. However, when adjustments were made for left internal mammary artery graft use, it did not change the early or late mortality risk for women20.
Quality of life following revascularisation and gender
Relief of angina, and improvement in quality of life represent the main benefits for both CABG and PCI and constitute the main indication for these procedures in most patients. In the BARI trial, there was a better functional status at one year among the patients undergoing CABG, but this difference had diminished after four years23. In the SoS trial24 the relative benefits of CABG and PCI in the improvement of health status differ in men and women at one year after intervention. Although in men CABG was clearly superior to PCI in improving patients’ health status, in women both procedures showed equal benefit at one year. In another study25, in patients undergoing CABG the baseline and follow-up Duke Activity Status Index scores for women were significantly lower than those of men, even after correction for pre-operative risk factors. The explanation for the gender differences in recovery after revascularisation procedures could relate, in part, to the different social roles of women and men; women may feel greater disruption than men, when they cannot resume their roles upon returning home after CABG. Furthermore, women are more likely to be unmarried, to live alone, and to report a lower level of social support than men.
Study limitations
When interpreting our results a number of issues should be considered. The number of women studied was smaller compared to men, so the power to detect a significant difference was lower. This post-hoc analysis is based on a randomised clinical trial for which all patients had specific inclusion and exclusion criteria, potentially limiting generalisation. However, patients in a randomised clinical trial may be an ideal group for studying sex differences because the rigorous trial design ensures that the women and men are reasonably comparable. It must be recognised that Euro-Qol questionnaire was developed to estimate usefulness and may not be as sensitive as disease-specific instruments to analyse treatment results. Furthermore, because treatment group assignment was not blinded, the patients’ knowledge of the treatment may have influence responses to the Euro-Qol questionnaire.
Conclusions
Women enrolled in the ARTS study were older and had more risk factors compared to men. The in-hospital outcome has identified an increased risk of bleeding complications in women treated with PCI. At five-years there were no gender specific differences in the incidence of major adverse cardiac and cerebrovascular events regardless of treatment therapy (PCI or CABG). However, quality of life differences indicate a role for more effective rehabilitation in women. The influence of gender in the era of drug-eluting stents and closure devices following PCI has to be defined.
Acknowledgement
This study was supported by Cordis, a Johnson & Johnson company.

