Abstract
Aims: To facilitate OCT images acquisition we developed a novel, simplified, non-occlusive technique based on manual infusion of a viscous isosmolar solution. The aims of the present study was to address the safety and efficacy of non-occlusive OCT images acquisition modality in a patient population with complex coronary lesions, and in various clinical scenarios.
Methods and results: OCT assessment was performed with the LightLab OCT Imagewire™ in 64 patients. The imaging acquisition technique was aimed at target lesion and proximal and distal reference segments. OCT images were deemed of good quality if they allowed both an accurate measurement of luminal area and a qualitative classification of the superficial plaque components.
In 60 patients (93.7%), the procedure was successful. The mean images acquisition time was 5.3±1.4 minutes. No major complications such as death, myocardial infarction or major arrhythmias were recorded. The average length of imaged segments was 28.6±6.1 mm and 95.1% of the imaged segments were deemed of sufficient quality to evaluate luminal area and plaque morphology (intra-observer and inter-observer variability 0.71, p<0.0001 and 0.68, p<0.0001 respectively).
Conclusions. The non-occlusive modality of OCT image acquisition is safe and effective, and promises to simplify the complex current occlusive technique, leading to a marked reduction of procedural time.
Abbreviations list
OCT: Optical coherence tomography
ACS: Acute coronary syndrome
PCI: Percutaneous coronary intervention
Introduction
Optical coherence tomography (OCT) is a new high-resolution intravascular imaging modality based on infrared light emission that visualises superficial components of the atherosclerotic plaques, similar to histology1-5. The images obtained are quite detailed and very useful for diagnostic and research purposes. However the image acquisition process presently in use requires vessel occlusion by means of gentle balloon inflation plus vessel flushing with saline infusion. This technique is rather cumbersome and time consuming and does not encourage its routine use6. To overcome this limitation we have developed a simplified method for OCT acquisition that does not require vessel occlusion.
Methods
Patient population
The study was conducted in compliance with the San Giovanni-Addolorata Hospital Bioethics Committee and received its approval. Informed consent was obtained for every patient.
The non-occlusive modality of OCT images acquisition was attempted in 64 patients (64 lesions) referred for coronary angioplasty. In 12 patients, OCT was repeated after stent positioning.
A large number of patients had acute coronary syndrome (ACS) (Table 1).
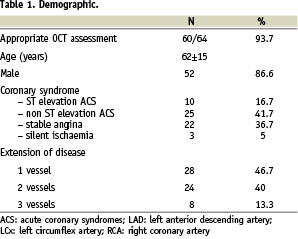
Table 2 shows the locations of the imaged lesions according to the coronary artery and its involved segment.
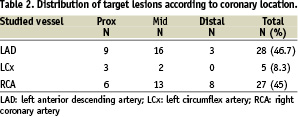
A complex-lesion population was studied; in fact 70% of the target lesions were type B or C according to the ACC classification7 (Table 3), and sub-occlusive lesions were a common finding (18 patients, 30%).
Quantitative coronary angiography (QCA) was routinely performed and measured the mean target lesion stenosis at 64.7±3% and the mean length at 15.1±3.2 mm.
Description of the technique
The M2 LightLab OCT wire (Imagewire™) has an outer diameter of 0.019”, and contains a 0.006” fibre-optic imaging core (less than 0.4 mm in diameter) and a distal radiopaque spring tip, similar to conventional guidewires. The system provides images at a longitudinal resolution of 15 µm. In our imaging protocol a 15.6 frames/sec. set-up was used.
OCT acquisition
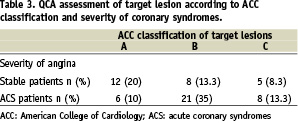
The OCT images acquisition was performed after coronary artery cannulation with 6Fr guiding catheter and administration of 50 U/Kg of e.v. heparin. A length of at least 25 mm, comprising target lesion and proximal and distal reference segments, is fundamental for a meaningful assessment of the coronary plaque. For safety reasons the target lesions were first crossed with the regular angioplasty wire, and then re-crossed with the OCT image wire. Once the image wire was positioned in the target vessel, it was pulled back at 2 mm/sec speed. Pull-back was then performed during simultaneous manual infusion of a viscous isosmolar infusion from the guiding catheter. The run-off of the coronary artery is dependent on its intrinsic anatomy and the clinical-pathological situation, and is important that the injection be gentle and controlled, thus making a manual injection preferable over an automated one. Our infusion protocol required a manual injection of a commercially available contrast (Iodixanol 320, Visipaque™, GE Health Care, Ireland), from the guiding catheter at an infusion rate between 1 and 3 cc/sec, based on the run-off of the artery and the online assessment of OCT image quality, while the blood is completely displaced from the artery during the whole acquisition period (Figure 1).
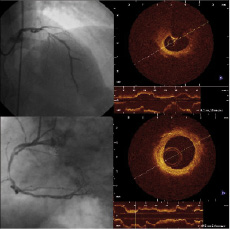
Figure 1. Examples of long OCT pull-back obtained with the non occlusive flushing technique. Severely diseased left anterior descending artery (angiography in the left upper panel) and right coronary artery (angiography in the left lower panel) were studied by OCT, using the non-occlusive flushing technique. Forty mm long segments, without artefacts, were studied in both arteries, as shown by the corresponding OCT longitudinal views, depicted in the right panels.
The infusion was interrupted in presence of marked ST elevation, QRS widening, and greater than 30% reduction of baseline heart rate. Also, the protocol limited the maximal amount of contrast solution to 35 cc per pull-back.
Because the LightLab image wire (Imagewire™) has been conceived with the OCT lens located at about 30 mm from the distal spring tip, the latter was placed 40 mm distal to the target lesion. This manoeuvre enabled the acquisition of a 10 mm long segment distal to the lesion.
In case the image wire could not engage the selected artery or negotiate the target lesion, the OCT probe was disconnected from the probe interface unit to improve image wire steerability and then reconnected after its adequate positioning.
The procedure was considered successful when the image wire was positioned at the level of the lesion, and images were of sufficient quality as to measure the vessel lumen and characterise the details of the atherosclerotic plaque at the target lesion and reference segments.
Qualitative and quantitative assessment of OCT images
All OCT frames were analysed off-line, in a validated core laboratory with specific expertise in intravascular imaging (Rome Heart Research, Italy). OCT images were deemed of good quality if they allowed both an accurate measurement of lumen area and a qualitative definition of the superficial plaque components.
Based on accepted criteria the following classification of atherosclerotic plaques was adopted: fibrotic, with calcific components, with lipid components and mixed with either lipid or calcific components1,2,3. Thrombus was defined as a mass protruding into the lumen; dissections as a rim of tissue clearly separated from the atherosclerotic plaque and floating into the lumen.
Quantitative measurements of lumen and plaque were obtained at the point of maximal narrowing. The minimal lumen diameter was calculated as a mean of two orthogonal measurements.
Statistics
Continuous variables were expressed as mean values±SD and compared by means of Student’s t-test; discrete variables were expressed as counts and percentages and compared by means of Fisher test. To assess intra and inter-observer variability, the results were compared using the K-test of concordance for categorical data. P value of <0.05 was considered significant.
Results
Safety and efficacy of OCT acquisition technique
Sixty-four patients underwent OCT evaluation and in 60 (93.7%) the procedure was successful (Figure 2).
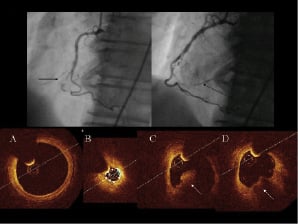
Figure 2. Example of very distal lesion, located in and thin right coronary artery (angiogram in the left upper panel), studied by OCT (arrow in the right upper panel indicates the OCT image wire) in a patient with acute inferior myocardial infarction. The simplification of the applied technique, which requires only a 0.19 inch image wire, enabled the assessment of OCT along the whole segment. In the bottom panels examples of OCT cross-sections are displayed. Panel A shows the proximal reference segment studied by OCT, panel B the site of maximal narrowing, having a lumen area of only 0.28 mm2, panel C reveals a large thrombotic formation (arrow) and panel D a superficial lipid pool, located just distal to the ruptured site.
The mean amount of contrast given for the basal OCT assessment was 30.5±3.3 ml (range 22 to 35 ml). In 12 additional patients a second contrast infusion of 28.8±6.2 ml was given to study the stented segments (range 18 to 35 ml). The mean time of OCT images acquisition (from the set up to the completion of the pull back) was 5.3±1.4 min. Four failures occurred: one was due to a non-coaxial engagement of the guiding catheter in the left main coronary artery. In three additional cases the limited trackability of the image wire did not allow to negotiate the culprit lesions.
No major complications and/or arrhythmias were recorded. One patient had a rise in CPK-MB enzymes, likely consequence of the percutaneous coronary intervention (PCI), rather than the OCT study.
During OCT images acquisition process ischaemic ECG changes occurred in 21 patients (35%), with ST depression in 17 (28.3%) and ST elevation in 4 (6.7%). Seven patients (11.7%) had angina. Ventricular ectopic beats were found in 6 patients (10%) while other major arrhythmias (ventricular tachycardia of fibrillation) were not observed. All electrocardiographic signs and patient’s symptoms resolved immediately at the completion of the image acquisition process.
Quality of OCT assessment along the longitudinal segment
The average length of imaged segments was 28.62±6.08 mm and, given the OCT frame rate of 15.6 / sec. and a 2 mm/sec pull-back speed, a total of 13,671 cross-sections were obtained in the 60 coronary segments. The cross-sections that were deemed inadequate for evaluation were 683 (4.9%), and did not differ according to the studied artery (5.0% for the LAD, 4.8% for the RCA and 5.6% for the LCx, p=NS). The length of the analysed segments differed significantly according to the target coronary artery (Figure 3).
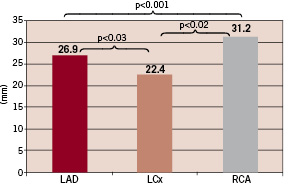
Figure 3. Comparison of lengths of optimal image acquisition in the right and left coronary arteries. In the right coronary artery (RCA) pull-backs were found to be significantly longer than in the left anterior descending (LAD) and left circumflex (LCx).
In all of them OCT imaging enabled the comparison of the lesion with a reference site.
Only 683 of 13,671 cross-sections (4.9%) were deemed of insufficient quality as to evaluate lumen area and plaque morphology. The test of concordance for identification of good-quality OCT images for repeated assessment by the same observer and by 2 two independent observers were 0.71 (p<0.0001) and 0.68 (p<0.0001) respectively. The unreadable cross sections were due to the non-optimal displacement of red blood cells by the solution.
Qualitative and quantitative assessment
The target lesions were predominantly fibrotic in 14 cases (23.3%), had lipid pools in 29 (48.3%), calcific components in 17 (28.3%). Albeit the predominant components of the plaques were considered, nine patients (15%) had mixed plaques (calcific and lipid pool). Complicated plaques with thrombotic formations were seen in 24 patients (40%). The minimal lumen diameter and area of the target lesions were 1.73±0.45 mm and 2.56±1.33 mm2, respectively. After stent deployment, OCT was capable of addressing the completeness of stent expansion in 10 of 12 cases (85%), by comparing in-stent minimal lumen area and lumen areas in reference segments. In the remaining two stented segments, OCT did not lead to a complete 360° assessment of all the stent cross sections along the stent. In two cases, an incomplete stent apposition to the vessel wall, requiring further expansion, was documented (Figure 4).
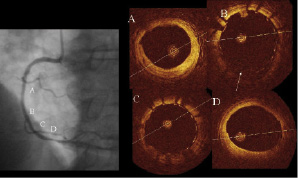
Figure 4. Assessment of stent deployment by OCT. A 3.0x28 mm Cypher stent was deployed in the mid-right coronary artery at 18 atm. After stent implantation angiography (left panel) revealed an optimal stent expansion but showed a luminal narrowing just distal to the stented segment (site D). OCT showed a stent minimal lumen area (panel C) larger than the reference ones (panel A and D) but revealed a site of malapposition (arrow in Panel B). Also at the site of lumen narrowing located just distal to the stent (panel D) OCT excluded dissections and confirmed the presence of a vessel spasm.
Discussion
A limitation of high-resolution intravascular imaging modalities is the need for a blood-free imaging zone, which in this study was achieved through continuous non-ionic contrast administration through the coronary guide catheter.
The physical and chemical properties of the solution used for this purpose are important: the viscosity of the contrast solution (several times higher then the blood) allowed blood displacement for a sufficient period of time as to be able to record OCT images of at least 25 mm segments of the coronary artery, while limiting the amount of solution used (total volume less than 30 cc); the balanced isosmolar solution did not interfere with the electrical and mechanical function of the myocytes. We consider this fact a significant improvement over the use of low viscosity, unbalanced solution, such as saline that requires short intermittent boluses and necessarily limits the assessment to a short target lesion spot. The limitation of the saline solution is significant also from the safety perspective. In fact, the injection of significant quantity of non-balanced electrolytic solution in the coronary circulation is associated with important electrocardiographic changes and potentially harmful effect on the myocardium, particularly in the setting of ACS.
The choice of an isosmolar contrast solution as the agent to displace red blood cells, derived from published data8 and experiments conducted from our group in an animal model (unpublished data). Many solutions were tested for their physical (viscosity, osmolarity) and chemical (electrolytes composition) characteristics, and the Visipaque™ presently gave the best safety and imaging acquisition quality. Based on these results a further research effort is being focused into the development of a solution with the same physical characteristics of Visipaque™ but without the iodine content and enriched with compounds that actually could be beneficial for the myocytes8.
The development of ad hoc solution designed for light-based intra-coronary imaging modalities and the introduction of new OCT platforms and optical probes, with a higher frame rate and acquisition speed, will further improve the length of analysed segments.
Advantages of a non-occlusive OCT technique
The technical ease of the OCT acquisition provides the opportunity to record images safely and quickly, also in the presence of complex anatomy in unstable patients with diffuse vessel narrowing. The limited amount of additional time (on average 5.3 minutes for image wire positioning and pull-back) required for the set-up and execution of the non-occlusive modality of OCT imaging, was of the utmost importance.
In a previous experience from our group4 we have used the technical solution currently applied by the LightLab (LightLab Imaging, USA), that requires balloon inflation and concomitant flushing. This approach was found to be less efficient and to cause more ischaemia (efficacy of 89%, ECG alteration in 68% and angina in 31% in a group of 19 patients studied). Also, the mean procedural time was significantly longer than that obtained with our non-occlusive approach (18.4±7.2 min vs. 5.3±1.4 min), however the mean length of analysed segments was found to be greater (41.2±11.3 mm vs. 28.62±6.08 mm) in the occlusive approach.
In the present study, the length of pull-back was influenced by the target coronary artery. The lower blood flow of the right coronary artery, as compared to the left coronary artery, enabled the acquisition of longer segments.
Although our group and other preliminary experiences indicated that the use of gentle vessel dilatation, as performed at low pressure through the Metricath balloon, does not lead to vessel wall and plaque distortion, the application of an occlusive modality of OCT images may induce an endothelial injury6, and certainly is more cumbersome and time consuming.
With its high resolution and unique characteristics, OCT is a powerful modality for detection of vulnerable coronary plaque. The most frequent variant of a vulnerable plaque is characterised by a lipid pool, a thin fibrous cap, and increased macrophage infiltration10,11. Quantitative analysis of these parameters over time may allow the monitoring of the effects of therapeutic interventions, particularly pharmacological therapy in the setting of secondary prevention. The simplified approach of OCT images acquisition promises to turn the technique into a valuable tool to address plaque composition in the search of plaque vulnerability in major coronary arteries, or to perform serial studies aimed at the quantitative changes in plaque components, such as superficial lipid pools.
This simplified technique will further the scope of OCT beyond its use as adjunct to PCI. Precise plaque characterisation optimises the choice and evaluation of the percutaneous interventional therapies; in addition, OCT is uniquely qualified to assess neointimal growth or hyperplasia in stented arterial sections12,13,14.
In the near future, the use of frequency domain OCT with its inherent high acquisition speed promises to reduce the amount of contrast to be given and OCT images may be obtained simply by infusing low quantity of isosmolar contrast through the guiding catheter.
Limitations
The incomplete visualisation of the whole circumference of lumen-plaque boundary is currently a draw-back of OCT and is exacerbated by the image wire non-coaxial location, a frequent finding with images obtained using the current version of the Imagewire™. The imaging technique with the occlusive balloon does not seem to overcome this technical problem, because the Imagewire™ is centred by the balloon only for a short coronary segment.
Conclusions
The non-occlusive modality of OCT image acquisition is safe and effective, and promises to simplify the complex current occlusive technique, leading to a marked reduction of procedural time.
Acknowledgments
We are indebted to Dr. Christopher Petersen, from LightLab Imaging for his technical review.
Supplementary data
To read the full content of this article, please download the PDF.
Vidéo 1

