A Plumber’s view: envy does not lead far
Double digit growth in procedures, a general agreement on the prognostic benefit of the implantation of ICDs and cardiac resynchronisation therapy in selected indications, a responsive industry heavily investing in the cardiology field with the fastest predicted growth; as interventionalists we have many reasons to be envious of our Electrophysiology (EP) colleagues who share with us the cathlab environment but are moving away from primitive X-ray tubes, introducing new and expensive technological gadgets for cardiac mapping which transforms their procedures into trendy computer games. This has become a further reason of division. In large hospitals the laboratories and often the technical and nursing personnel have become different, sometimes almost totally separated as a different nearly autonomous department competing for cathlab time and resources. The attitude of general cardiologists towards EP and interventions is very different. Sometimes we feel offended seeing patients with post-ischaemic left ventricular dysfunction rushed to receive ICDs and/or CRT, before having done a coronary angiography to establish the presence and extent of residual ischaemia and the potential to revert hibernation with myocardial revascularisation. We are upset seeing patients with atrial fibrillation happily referred for their second or third ablation procedure by the same clinicians who will advise medical therapy for patients with poorly controlled angina and chronic total occlusions.
Most often, if somebody achieves more than you do, it is because he deserved it and this is true also in this case. Electrophysiologists have carefully guarded the process of training, developed exams for certification and ensured close bonds within their community, presenting a unified position towards the rest of the cardiology and the medical community. Electrophysiologists have managed to force the industry to support sufficiently large trials with clinical endpoints in strict cooperation with heart failure specialists to have a Class I A indication for prognosis (mortality) approved for many indications. As a member of too many interview panels, I noticed that aspiring EP and imaging cardiology specialists often outperform interventional fellows in their previous curriculum and their performance at the interview, clearly showing that our smartest future colleagues have already perceived where the greatest growth and development is going to be.
The electrician’s response: perception and reality
Undoubtedly, invasive cardiology has significantly changed over time, and so have the perceptions and realities about the capabilities of the two key stakeholders of invasive cardiology,
the plumbers and the electricians. It was not a long time ago when implantation of pacemakers or the conduction of electrophysiological studies was considered a niche activity in the vast majority of academic and community hospitals. Professional attitudes, and the performance of a few physicians, who were later named electrophysiologists, more frequently resembled the creation of Frankenstein rather than a medical, eventually curative act. Until recently, there was an extensive perception that electrophysiologists were a second-class community within invasive cardiology. In contrast, the interventional cardiology community was considered, or at least perceived as, a group of rescuers and physicians who never made any mistakes. The electrophysiology community was, and remains today, stunned and somewhat annoyed by the communication skills of interventionalists, who continue feeding the public opinion that once you get a stent you are shielded against atrial fibrillation occurrence/recurrence, heart failure, and even sudden death. I am still impressed (and disappointed) to see patients who are electively admitted to hospital for the third or fourth coronary intervention presenting with a low ejection fraction, discharged home without mentioning that they should consider an implantable cardioverter-defibrillator given the risk of sudden cardiac death; or when a patient has had an overnight admission due to paroxysmal atrial fibrillation and atypical chest pain, present slightly elevated troponin levels and undergo coronary angiography with no-treatable coronary findings and who leave the hospital with antiarrhythmic drugs without being made aware of the potential curative effect of catheter ablation.
The recent impressive results of device therapy, including cardiac resynchronisation therapy and ICD, as well as the curative ability by catheter ablation of different cardiac arrhythmias, have taken away some of the attention from interventional cardiology in favour of electrophysiology. Moreover, in some geographic areas, the high density of invasive laboratories along with the difficulty to differentiate the quality of their proposed services, have given hospital administrations the incentive to invest in a rapidly growing, high-technology driven service, the electrophysiologic unit. Consequently, junior cardiologists are considering electrophysiology as a career opportunity, and allied professionals are growing intrigued by the possibility of getting involved in a long-lasting, yet intellectually challenging and curative procedures.
What looks like an expensive video game is in reality the highest level of integration of cutting-edge navigation technology, cardiac imaging and high professional skill in catheter manipulation. For someone like myself, who prefers performing electrophysiological interventions and device implantation, it is equally rewarding
to support the central interventional activity by performing primary angioplasty. I do not see myself as an exception or an outsider, there are indeed several European centres in which electrophysiologists are still performing cardiac interventions and vice-versa. The key is to have been exposed to both invasive and electrophysiological training, to have acquired equal skills and competence in both subspecialties. I greatly enjoyed my training in interventional cardiology, which 20 years after provides me with the level of confidence necessary in performing CRT implantations, a procedure significantly closer to PTCA than to electrophysiology.
A consensus view: how to grow together?
With increasing specialisation, shared practice and interaction has become more limited. We may scorn the idea that the care of a cardiac patientis split among many different consultants, but the good old days when the authority of a cardiologist issued a final verdict for diagnosis and treatment in all cardiac pathologies are long gone. Interaction and a team approach are the only remedy to super-specialisation. A patient in heart failure should not see his treatment limited to drugs when he visits an HF specialist; to defibrillators and/or CRT when he visits an electrophysiologist; to PCI or CABG when he is seen by an interventionalist or cardiac surgeon; to diet and rehabilitation when he seeks the advice of a prevention specialist; or to countless imaging investigations when he sees a specialist in cardiac imaging. All these tests and treatments might be helpful with a focussed approach targeted to the individual patient’s needs and not to the confidence the individual consultant has in one or the other technique.
Novel therapies, such as left atrial occlusion devices and percutaneous mitral valve repair, enlarge the grey zone between interventional cardiology and electrophysiology. Who will do a better implantation of a Watchman or a Mitraclip? An interventionalist who has specific experience of other structural interventions, or an electrophysiologist who is used to transseptal puncture and more often treats patients with atrial fibrillation or heart failure, the typical candidates for the two procedures?
Both the EAPCI and EHRA strive for the recognition of their respective subspecialties in European cardiology, a long needed action. At the same time, both scientific societies should ensure that common training and fellowship programs facilitate the dialogue between the two subspecialties, providing an optimal background for both subspecialists when they want to venture into new treatment modalities found in the “border zone”. Certification for new procedures should be based on specific expertise agreed by impartial expert panels, without preventing one or the other specialist to embark in these demanding procedures. Integration of invasive and noninvasive imaging modalities, pioneered in EP, is now expanding to other coronary and structural interventional procedures. Both Associations should also work together within the future Association of Cardiovascular Imaging to ensure that the noninvasive components of these techniques are not ring-fenced and only reserved to imaging subspecialists, and we should create opportunities for both trainees and older specialists to receive the clinical knowledge and level of certification required for successfully integrating them in their practice. Both Associations have an interest in ensuring that the European Society of Cardiology understands and promotes the central role of invasive cardiology. The upcoming 2011 ESC congress in Paris has a record number
of 10,836 submissions, more than in Barcelona in 2006 when the ESC congress was linked to the World Congress. Figure 1 reports the number of abstracts submitted for each subspecialty. Arrhythmias and interventions have a leading position with 1,381 and 1,280 abstracts submitted, respectively; a position which is certainly greater if you consider that many of the abstracts in three of the other leading topics (heart failure, valve disease and ischaemia) are also likely to be strictly linked to the results of invasive techniques applied in these conditions.
In short, we should look for cooperation rather than for competition which only generates insane jealousies and leads to no progress for anyone.
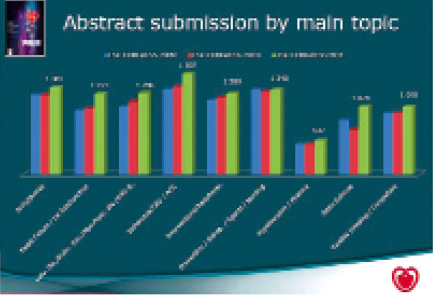
Figure 1. Abstract submission, by topic, to the last three ESC congresses.