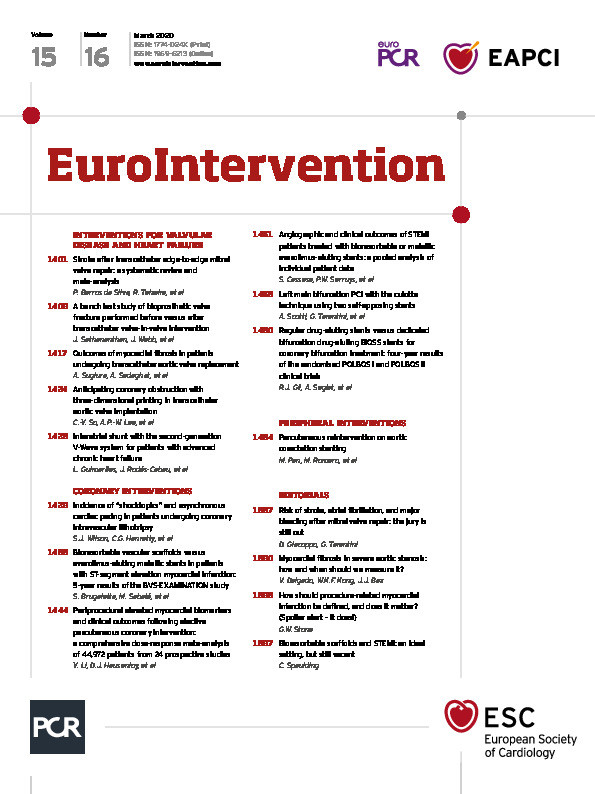
There are a few days to go before the virtual event of the American College of Cardiology, where – as always and despite current difficulties due to the COVID-19 pandemics – a line-up of late-breaking clinical trials will be presented. In the interventional cardiology field, some trials of antithrombotic pharmacotherapy are worthy of attention: TAILOR PCI (on genotyping guidance for antiplatelet therapy management after PCI), TICO (on early aspirin discontinuation in patients with acute coronary syndromes), VOYAGER PAD (on low-dose rivaroxaban after revascularisation of peripheral artery disease), and POPular-TAVI Cohort B (on antithrombotic strategies for TAVI patients on baseline oral anticoagulation). Also, the UK-TAVI trial will independently assess the merits of TAVI versus surgical aortic valve replacement, and the sham-controlled Spyral HTN-OFF MED trial will define the role of renal denervation in the absence of antihypertensive medications. These highly anticipated studies will inform clinical practice and probably fuel social media reactions in the next few months. Meanwhile, this March edition of EuroIntervention is ready for you with numerous new articles on a variety of topics.
In the section dedicated to coronary interventions, this issue features a comprehensive meta-analysis of 24 prospective studies and 44,972 patients from Yuehua Li, Derek J. Hausenloy and colleagues about one of the hottest topics at the start of 2020 – periprocedural myocardial infarction. The authors found a positive dose-response relationship between isolated cardiac troponin I and CK-MB and all-cause mortality for specific cut-offs above the 99th percentile upper reference limit. The need for further consensus on the definition of “clinically meaningful” periprocedural myocardial infarction is further discussed in an accompanying editorial by Gregg W. Stone.
Two studies and an accompanying editorial from Christian Spaulding expand on current knowledge surrounding a potential role of bioresorbable scaffolds in primary PCI. In the first study, Salvatore Cassese, Patrick W. Serruys and colleagues pooled two randomised trials comparing the bioresorbable scaffold and the everolimus-eluting stent, and reported on their angiographic and clinical outcomes at one year. Although the Absorb™ bioresorbable scaffold is no longer used, such comparisons remain of interest to understand the caveats and potential of this technology, and to define directions for new research avenues. The results of this pooled analysis are indeed encouraging on the midterm angiographic and clinical performance of the device in ST-segment elevation myocardial infarction, but the authors highlight the importance of long-term outcomes to ascertain fully the pros and cons of the technology. Indeed, in the second study, Salvatore Brugaletta, Manel Sabaté and colleagues report on the five-year results of EXAMINATION, a propensity-matched comparison of 235 pairs of patients with ST-segment elevation myocardial infarction treated with the bioresorbable scaffold or the everolimus-eluting stent. Here, with about 4% of scaffold thrombosis at five years, the study results imply that the road to reintroducing bioresorbable scaffolds in clinical practice, if anything, remains long and bumpy.
Coronary lithotripsy is gaining attention and popularity among interventionalists. As with any new procedure, we need to know more about its off-target effects. An interesting study from Simon J. Wilson, Colm G. Hanratty and colleagues characterises the role of intravascular lithotripsy to precipitate ventricular ectopics (what the authors refer to as “shocktopics”) and asynchronous cardiac pacing. In the study, the incidence of provoked ventricular capture was as high as 77.8%, with a higher prevalence in patients with a heart rate <65 bpm before the procedure. The authors further describe the morphology of such “shocktopics” and their dependence on target lesion location. Although there were no associated clinical events, further systematic evaluation of this phenomenon is likely to happen in future investigations. Finally, a study from Robert J. Gil, Agnieska Segiet and colleagues reports on the 4-year results from early clinical trials on a dedicated stent for bifurcation lesions.
In the section dedicated to interventions for valvular heart disease and heart failure, Janarthanan Sathananthan, John Webb and colleagues add new information on bioprosthetic valve fracture, a procedure that is increasingly performed to improve the outcomes of transcatheter aortic valve-in-valve interventions. An open question is when this procedure is most useful – before or after the implantation of the second valve? Using an experimental model of hydrodynamic testing, the authors assessed three commercially available valve designs, implanted inside a bioprosthetic surgical valve. Each valve was tested in conditions of no fracture, fracture “before” valve-in-valve implantation and fracture “after” valve-in-valve implantation. I invite you to look at the results and decide whether they will eventually make a change to or corroborate your practice. This elegant experimental study highlights that the timing of fracture actually plays a role in valve expansion and modifies the post-procedural gradient of at least two of the tested bioprostheses. In another study of TAVI patients, Atsushi Sugiura, Alexander Sedaghat and colleagues investigated the impact of myocardial fibrosis, assessed by means of a recently developed risk score, on left ventricular reverse remodelling and prognosis. Interestingly, although myocardial fibrosis has been predicated as an important factor for poor prognosis in patients with aortic stenosis, the study disputes this hypothesis, suggesting a limited impact of myocardial fibrosis on clinical outcomes. Enjoy the accompanying Editorial by Victoria Delgado for more insights on this topic.
Patricia Barros da Silva, Rogerio Teixeira and colleagues looked at the risk of stroke after transcatheter mitral valve repair with the MitraClip® system. Stroke is a devastating outcome, but typically single-digit, which makes comparisons across techniques challenging, and sets the rationale for a meta-analysis. Indeed, the haemodynamic profile of patients undergoing the MitraClip procedure may result in blood stasis and an increased risk of atrial thrombosis and thromboembolism. Atrial fibrillation is frequent in patients with mitral regurgitation and may act as an additional contributing factor. The meta-analysis includes a total of 1,881 patients and 61 events from 10 – mostly observational – studies (7 using surgical mitral valve repair as control, 3 using optimal medical therapy as control). The authors recognise that the paucity of randomised trials included and the low number of events for direct comparisons versus surgery are important limitations of their approach. However, in a data-free zone, these results are informative and may guide the design of future investigations of antithrombotic strategies to reduce the risk of stroke after MitraClip therapy. An accompanying Editorial by Daniele Giacoppo and Giuseppe Tarantini will help the reader to interpret and put this meta-analysis into perspective.
Entering the MitraClip area somehow leads us to heart failure. In another study, Leonardo Guimarães, Josep Rodés-Cabau and colleagues report the results of their initial in-human experience with a device for left atrial decompression, which creates an interatrial shunt to improve the functional status and quality of life of patients with advanced chronic heart failure. This report is about the second generation of the V-Wave device, implementing modifications to improve late patency. In the prior iteration, the presence of a valve led to early degeneration and shunt narrowing or occlusion. Device success was obtained in 90% of cases. Symptoms, quality of life, exercise capacity and echocardiographic parameters were reported for patients who were alive at one year.
Finally, in the section on peripheral interventions, on the topic of aorta narrowing, Manuel Pan, Miguel Romero and colleagues assessed the efficacy and safety of percutaneous reintervention in patients with aortic coarctation stenting performed at an early age. Interestingly, the study corroborates the understanding that patients with aortic coarctation treated with stent placement at an early age can be successfully re-treated after the completion of their somatic growth.
That’s it for the March issue of EuroIntervention. Please do not hesitate to share your comments and feedback. Waiting for the news from the scientific sessions of the American College of Cardiology, the Editorial Board hopes that you will find this issue a pleasant read and a useful aid to your practice.
Supplementary data
To read the full content of this article, please download the PDF.