Abstract
Aims: The aim of this study was to review all percutaneous coronary interventions (PCI) performed in our department for chronic total occlusions (CTO) over the last three years, and analyse the success rate and complications.
Methods and results: We retrospectively studied all PCIs for total occlusions of more than four weeks duration, performed between 2004 and 2006, after excluding multivessel PCI, venous grafts and in-stent restenosis (n=106 cases). The in-hospital complications were recorded; periprocedural myocardial infarction (MI) was defined as elevation of troponin I more than 3 times the upper reference limit. Procedural success was defined as angiographic success and absence of major adverse cardiac events (MACE: death, large MI, emergency bypass). Logistic regression analysis was used to determine predictors of success and complications. The procedural success was 77%, and was mainly associated with duration of occlusion less than three months (OR 4.17, 95% CI 1.23-14.28, p=0.02), preprocedural TIMI 1 coronary flow (OR 3.29, 95% CI 1.00-10.82, p=0.05) and absence of ipsilateral collaterals (OR 4.54, 95% CI 1.35-16.67, p=0.01). Periprocedural MI occurred in 12 cases (12%), while MACE occurred in 3 (3%). The only parameter significantly associated with periprocedural MI was the obstruction of side-branches (with diameter >1 mm) within 5 mm of the CTO (OR 10.00, 95% CI 1.76-56.67, p<0.01).
Conclusions: In our CTO cohort the success rate was 77%, with a low complication rate. Periprocedural MI was mainly due to obstruction of side-branches.
Introduction
Chronic total occlusion (CTO) of one or more coronary arteries is the most common cause of incomplete revascularisation by percutaneous coronary interventions (PCI) and a common cause of referral for bypass surgery. Performing a successful PCI in a CTO has been shown to relieve symptoms of ischaemia, to reduce the need for surgical revascularisation and, in some observational studies, to prolong survival1-4. Indeed, recanalisation of a CTO increases hyperaemic and resting myocardial blood flow, as well as regional myocardial contractility5. Despite these favourable data, CTOs comprise a minority (<10%) of the PCIs performed in most centres, due to low success rates and risk of complications1. PCI in a CTO demands advanced technical skills, and sometimes use of specific equipment. The duration of the procedure is longer, necessitating prolonged fluoroscopy time and large amounts of contrast dye, that increase the risk for both the patient and the catheterisation laboratory personnel6. The technical success of angioplasty in a CTO is about 70% (60% to 90% in different reports), far inferior from that of a non-occlusive lesion, which exceeds 95%1-3,7-8. The complications of such a procedure are not very well studied, but in most series, the major adverse cardiac events were not different between CTO and non-CTO lesions3,9. In a recent report from the Mayo Clinic, the rate of complications has considerably declined during the last years, due to the use of stents and the growing experience of the operators8. In the present study, we retrospectively analysed all PCIs for CTOs that were performed in our department in the last three years. We examined the angiographic and procedural success, the in-hospital complications, and the factors that influenced success and complications.
Methods
Study population and design
We studied retrospectively all PCIs performed in our department from January 2004 until February 2007. A chronic total occlusion was defined as one having TIMI 0 or 1 coronary flow and duration more than four weeks2,9. The duration of the occlusion was estimated by previous angiography, history of acute coronary syndrome, or the duration of symptoms. PCIs for in-stent restenosis and PCIs in venous grafts were excluded. We also excluded interventions in more than one artery at the same time (e.g. CTO in right coronary artery and non-CTO in left anterior descending), since this could cause difficulty in trying to explain cardiac biomarker elevation after PCI.
The diagnostic and interventional digital image archives of these patients were reviewed using quantitative coronary analysis (QCA) and the following parameters were recorded: occluded vessel, TIMI flow, morphology of occlusion, vessel diameter, length of occlusion, vessel tortuosity, vessel calcification, presence of side-branches within 5 mm of the occlusion, and collateral circulation. The length of the occlusion was determined by detection of the distal vessel either by collaterals or by antegrade flow after crossing and initial opening of the lesion, but this has been impossible in two unsuccessful cases. We classified coronary side-branches as small (<1 mm diameter), medium (1-2 mm diameter) or large (>2 mm diameter)10. Collaterals were characterised by: a) their main anatomic pathway (septal, atrial, epicardial or bridging)11,12, b) the filling of the recipient artery according to Rentrop et al (grade 0, 1, 2 or 3)13 and c) their size according to the classification by Werner et al (CC0: no continuous connection, CC1: continuous connection ≤0.3 mm, or CC2: continuous connection ≥0.4 mm)14. We also classified collaterals as ipsilateral (originating from the proximal segment of the occluded artery) or contralateral (originating from another artery). The extent of coronary artery disease and the ejection fraction of the left ventricle were assessed. We also recorded the duration of fluoroscopy and the amount of contrast dye used during PCI.
Angiographic success was defined as <20% residual stenosis after stent implantation, with TIMI 3 flow15. As angiographic complications we considered: obstructive dissection of the vessel, perforation of the vessel, no-reflow, and obstruction of side-branches with diameter >1 mm. Side-branch compromise was defined as worsening of ostial side-branch disease resulting in >70% stenosis with TIMI 2 or 3 flow. Side-branch occlusion was defined as TIMI flow 0 or 1 in a side-branch that was not occluded before PCI.
The patients’ medical records were reviewed regarding the following parameters: demographic data, risk factors, history of the patient, cardiovascular medication, duration of the coronary occlusion and in-hospital complications. The duration of CTO was classified as <3 months, >3 months or undetermined (when there was no certainty about the exact duration of the CTO, but it was certainly >4 weeks). The maximum values of creatine kinase-MB (CK-MB) and troponin I (TnI) post-PCI were recorded (measurement took place six hours after the procedure and the following day, but a complete set of cardiac enzymes was lacking in five patients). CK-MB and TnI were measured by enzymatic immunoassay, and the upper reference limits (URL) in our laboratory are 5 ng/ml for CK-MB and 0.2 ng/ml for TnI.
As clinical complications we considered the following: vascular (complications from the arterial access necessitating repair, blood transfusion, or prolonged hospitalisation), periprocedural myocardial infarction, cerebrovascular event, acute renal failure (necessitating dialysis), serious contrast allergy (systemic allergic reaction with bronchospasm and/or haemodynamic compromise) and cardiac tamponade. Periprocedural myocardial infarction was defined as elevation of TnI more than three times the URL (TnI >0.6 ng/ml), according to the new universal definition of myocardial infarction16. As major adverse cardiac events (MACE) we considered: death, large myocardial infarction (TnI >5 ng/ml), and emergent bypass surgery. We defined procedural success as angiographic success and absence of MACE15.
PCI technique
The interventions were performed by four different operators. The clinical decision to attempt treatment of a CTO was based on patient’s symptoms and/or inducible ischaemia or myocardial viability from functional tests. The intervention was performed via the femoral approach, using 6 Fr or 7 Fr guiding catheters. A variety of angioplasty guidewires were used in order to cross the CTO (soft-tip, intermediate-tip, stiff, tapered-tip, hydrophilic-coated) with the majority of the lesions being crossed by moderately stiff wires. An over-the-wire balloon was often used to increase the support of the guidewire, verify intraluminar position with contrast injection and permit the exchange with a softer wire after crossing the occlusion. The parallel wire technique was used in some cases to help enter the true lumen of the vessel. In cases of uncertainty about the position of the wire, angiography of the contralateral coronary artery was performed, in order to visualise collateral circulation (three cases). The retrograde technique to cross the occlusion (using collaterals from the contralateral artery) was not used. Dedicated CTO techniques such as Tornus catheters, laser catheters or vibrational PCI were not performed. After crossing the lesion with the guidewire, dilatation with progressively larger balloons was performed before stent implantation. The mean number of stents per intervention was 1.6±0.8, while the mean number of balloon dilatations was 5.8±3.4. Drug-eluting stents were implanted in 91% of the successful cases.
All patients were pretreated with aspirin. Sixty-five percent (65%) of patients were pretreated with clopidogrel, while the rest were given a loading dose of 300-600 mg followed by 75 mg daily. Thirteen percent (13%) of patients were treated with a glycoprotein IIb/IIIa inhibitor, after the successful intervention. Heparin 60-100 IU/kg was given intravenously to all patients at the beginning of the procedure.
Statistics
Quantitative data are presented as mean value±standard deviation. Categorical data are presented as frequencies. Some quantitative parameters (duration of CTO, TnI) were stratified and converted to categorical, in order to facilitate the statistical analysis. We applied univariate and then logistic regression analysis to examine which parameters are associated with procedural success and complications. A p value of less than 0.05 was considered statistically significant. All calculations were done using the statistical software SPSS for Windows.
Results
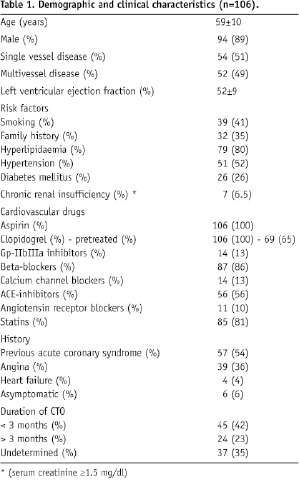
Among 3,122 patients who underwent PCI during the study period, 253 (8%) had a total coronary occlusion, and 106 (3%) met the inclusion criteria. The demographic and clinical data of the study population are shown in Table 1.
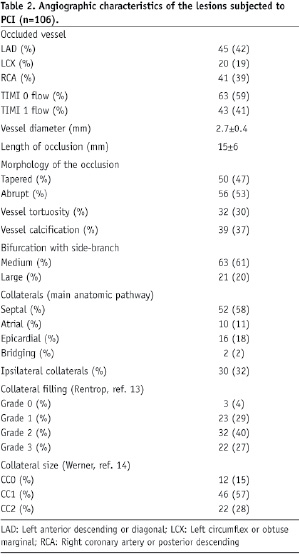
The angiographic characteristics of the lesions subjected to PCI are shown in Table 2.
The CTO was successfully recanalised in 85 of 106 patients (angiographic success = 80%). In 21 cases the intervention was unsuccessful, due to: a) failure to cross the CTO with the wire (17 patients) or the balloon (two patients), b) failure to dilate the lesion (one patient), or c) dissection of the coronary artery proximal to the obstruction (one patient). The mean x-ray time was 17±9 min, and the mean contrast volume used was 452±135 ml. The observed complications are shown in Table 3.
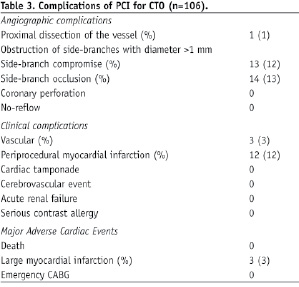
MACE occurred in three patients (3%). Therefore procedural success was achieved in 82 patients (77%).
Table 4 shows the univariate analysis of the most important clinical and angiographic parameters associated with procedural success.
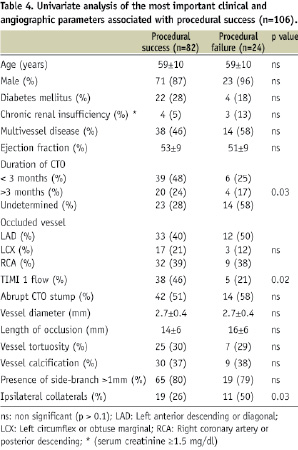
Logistic regression analysis showed that absence of ipsilateral collaterals, short duration of occlusion, and pre-procedural TIMI 1 flow independently predicted procedural success (Table 5).
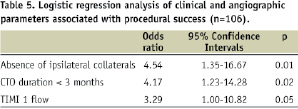
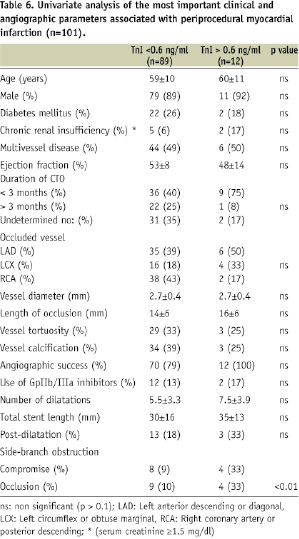
Table 6 shows the univariate analysis of the most important clinical and angiographic parameters associated with periprocedural myocardial infarction.
Logistic regression analysis showed that obstruction of side-branches (>1 mm in diameter) during PCI, was the only parameter that predicted this complication (OR 10.00, 95% CI 1.76-56.67, p<0.01). The odds ratio was 8.87 for side-branch compromise (95% CI 1.85-42.52, p<0.01) and 7.89 for side-branch occlusion (95% CI 1.67-37.16, p<0.01). As shown in Figure 1, TnI levels after PCI increase in a linear association with side-branch compromise or occlusion.
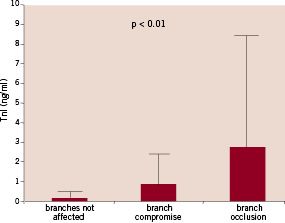
Figure 1. Mean TnI values after PCI, in association with the patency of side-branches (with diameter > 1 mm) within 5 mm of the CTO.
All cases with MACE (three large myocardial infarctions) had side-branches affected by the intervention (two occlusions and one compromise), but the number was too small to be statistically relevant. In some cases, significant side-branches appeared after opening the occlusion, but troponin elevation was only associated with obstruction of side-branches that were patent before PCI. Interestingly, occlusion of acute marginal (right ventricular) branches of the right coronary artery was never accompanied by cardiac biomarker elevation (n=5 cases). Figure 2 shows the angiograms of an angiographically successful PCI in a CTO of the right coronary artery, complicated by obstruction of a large posterolateral branch and myocardial infarction (CK-MB= 47.7 ng/ml, TnI=6.61 ng/ml).
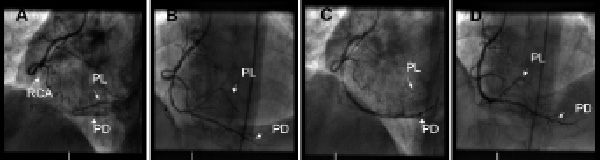
Figure 2. A: Angiogram before PCI showing total occlusion of the mid right coronary artery (RCA) and filling of the posterior descending (PD) and the posterolateral (PL) branches via ipsilateral collaterals; B: Recanalisation of the total occlusion after balloon inflations; C: Loss of the PL branch (1.8 mm diameter) after stent implantation in RCA to PD; D: Final angiogram showing successful recanalisation of the RCA occlusion after stenting, but significant ostial stenosis of the PL branch with TIMI 2 flow; the ipsilateral collaterals are also compromised.
Discussion
In this single-centre observational study, we examined the outcomes after PCI for CTOs, over the last three years (2004-2007). Contemporary PCI technique was used and drug-eluting stents were implanted in the majority of patients. All patients received dual antiplatelet therapy and 81% were taking statins. The enrolled cases (n=106) were a small minority (3%) of all PCIs performed during the same period, mainly due to strict inclusion criteria. Angiographic and procedural success was 80% and 77% respectively. The main cause of failure was inability to cross the lesion with the wire or the balloon. These findings are in accordance with previous series, where the success rate is 60-90%, and failure is mainly caused by inability to pass the wire across the lesion into the true lumen of the distal vessel2-3,7-8. Predictors of success have been delineated in previous studies, where the most important parameters associated with procedural failure are: long duration of the occlusion, small vessel diameter, long lesion, abrupt CTO stump, excessive tortuosity and calcification of the lesion, and presence of bridging collaterals17,18. Very recently, Barlis et al reported that indeterminate occlusion duration predicts procedural failure in the recanalisation of CTOs19. In the present study, we also found that long or undetermined duration of occlusion, and preprocedural TIMI 0 flow are inversely associated with procedural success. We also showed, for the first time, that the presence of ipsilateral collaterals (collaterals originating from the proximal segment of the occluded artery) is associated with procedural failure.
MACE occurred at a rate of 3%, and consisted of three patients with large periprocedural infarctions (TnI >5 ng/ml), all associated with obstruction of previously patent side-branches during PCI. Periprocedural myocardial infarction (TnI >0.6 ng/ml) was observed in 12% of cases. Using logistic regression analysis, we found that the only parameter associated with troponin elevation was the compromise or occlusion of side-branches during PCI. This rate of ischaemic complications is considered low, in comparison with that of non-occlusive lesions. Indeed, the rate of periprocedural myocardial infarction in 886 consecutive patients undergoing PCI for stable non-occlusive lesions during 2006, in our department, was 26% (p=0.02 compared to 12% in our CTO cohort). The rate of MACE was not different between these two groups (3.5% and 3% respectively, p>0.1). Bahrmann et al, in a prospective study, also found a low incidence of cardiac biomarker elevation following PCI for CTO (14% troponin elevation versus 20% in non-CTO lesions)9.
Elevation of cardiac biomarkers after PCI reflects myocardial necrosis and has been linked to increased risk for future cardiac events20-22. It is a common phenomenon, caused by a number of periprocedural events that may act alone or in combination, such as ischaemia due to prolonged balloon inflations, occlusion of side-branches, disruption of the collateral circulation, obstructive coronary dissection, coronary spasm, coronary perforation, and embolisation of atherothrombotic material16,23. The presence of intracoronary thrombus, as in acute coronary syndromes, increases the risk of the intervention, and can result in no-reflow phenomenon24,25. Such embolic complications have decreased with the use of stents, dual antiplatelet therapy, and glycoprotein IIb/IIIa inhibitors. However, microembolisation cannot be entirely prevented and is considered as the main cause of mild cardiac biomarker elevation26,27. In the CTO lesions, despite the high atheromatous load, the thrombotic material is well organised, thus possibly minimising the effect of microembolisation28. According to Bahrmann et al, this is the most likely explanation for the observed low incidence of cardiac biomarker elevation after PCI for CTOs9. In our study, there was no evidence of intracoronary thrombus, embolisation, or no-reflow during interventions for CTOs. More recent occlusions (<3 months) had a higher incidence of periprocedural myocardial infarction (20%) – though not statistically significant – suggesting a possible role of microembolisation from these softer plaques. There was also a trend for higher incidence of biomarker elevation with more balloon dilatations, longer total stent length and post-dilatation (Table 6). This suggests that ischaemia from balloon inflations could also play a role. Finally we found a strong association between troponin elevation and obstruction of side-branches, which was statistically significant.
CTOs are usually long lesions and a high incidence of side branch involvement may be expected. In the present study, side-branches with diameter >1 mm were present in 81% of cases, within 5 mm of the CTO (Table 2). Operators should try to preserve important side-branches that are patent before PCI, in order to reduce ischaemic complications. After crossing successfully the CTO with the wire, a large side-branch or a branch that perfuses an important myocardial territory can be protected with a second wire and then treated in the same way as a non-occlusive bifurcation lesion.
Study limitations
The study population was small (106 patients), due to the strictly defined criteria. Many patients during the study period were subjected to PCI for CTO and non-CTO lesions at the same time. These cases were excluded, in order to be able to analyse cardiac biomarker elevation after PCI. In a considerable number of cases the duration of the occlusion was less than three months and the coronary flow was TIMI 1, which are more likely to be soft lesions. Various definitions of CTO are found in different papers, so some would not consider these as true CTO lesions. The rate of complications was also small (12 cases with periprocedural myocardial infarction), which may hamper robust statistical analysis. Dedicated CTO techniques or devices were not used. This may have improved success rate, but also possibly adversely affect ischaemic complications and increase x-ray time, contrast amount and cost.
Conclusion
Successful recanalisation of a CTO can relieve symptoms of ischaemia, reduce the need for surgical revascularisation and may prolong survival. PCI in a CTO is technically a highly demanding procedure, with a success rate about 70% in most studies. The MACE rate is similar to PCI in non-occlusive lesions. The incidence of troponin elevation is lower than in PCI for non-CTO lesions, possibly due to less microembolisation of thrombotic material. Elevation of cardiac biomarkers after an intervention for CTO is mainly due to compromise or occlusion of side-branches that are often involved.
Acknowledgements
Ioannis Paizis is recipient of a scholarship from “Hellenic Heart Foundation” (ELICAR).

