Bifurcation coronary lesions are commonplace, but present a difficult challenge to the interventional cardiologist, with a high complication rate in both the long and short term1. Major adverse cardiac events (MACE) are significantly higher in bifurcation versus non-bifurcation lesions2 and this is chiefly attributable to target vessel revascularisation rather than death or myocardial infarction3.
The first meeting of the European Bifurcation Club took place on 15th to 16th of September, 2005 in Bordeaux and was organised by Drs. Thierry Lefèvre, Yves Louvard, Remo Albiero, Olivier Darremont, Manuel Pan and Goran Stankovic. The aim was to bring together an invited faculty of European cardiologists involved in this field to discuss optimal strategies for treating bifurcation coronary artery disease and also to interact with the industry. After 36 hours of discussions an attempt was made to reach a consensus view, and this manuscript reflects the results of these discussions.
The following topics were considered:
– Definitions
– Pharmacology
– Imaging and QCA of bifurcation lesions
– Plaque modification
– Technique
– Lesion location
– Philosophy
– Physiology
– Dedicated bifurcation devices
Definitions
Definition and classification of bifurcation coronary disease is not straightforward. A general consensus exists that if a branch vessel is large enough to be stented, then the coronary division merits the term “bifurcation”. This does not take account of any difference in relative size of the two vessels in question, but does have the advantage of uniformity. In practice, therefore, divisions where branch vessels of > 2.25 mm diameter emerge are considered to represent bifurcations. The pattern of disease at the bifurcation may be further classified into “true” bifurcations (where the lesion involves both the main and side vessels to a significant degree – ICPS types 1 and 4) and “false” bifurcations (where only the main or side vessel is significantly involved – ICPS types 2, 3, 4a, 4b) at a bifurcation. The relative value of distinguishing between true and false bifurcations has not been established.
There are several eponymous classification systems in use, but none has gained full acceptance. The most widely used is the ICPS classification4. This however is not a particularly “intuitive” classification and can be difficult to remember in clinical practice. The MEDINA classification5 was considered to be the most simple to understand and use and was adopted by everybody (Figure 1).
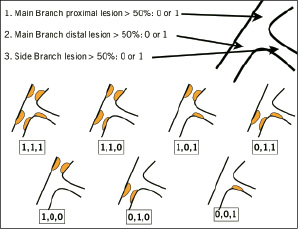
Figure 1.
Bifurcation site
Not all bifurcations are the same, and this is particularly the case for distal Left Main Stem disease – the “big bifurcation”. Whereas branch vessels can be considered of subsidiary importance, the left main stem subtends the circumflex and left anterior descending coronary arteries, neither of which can be ignored or sacrificed with impunity (with the exception of vestigial non-dominant circumflex vessels) Therefore the left main stem has “special status” within bifurcations. Important data on the treatment of left main stem disease, including the interventional treatment of distal bifurcation disease will be available from the SYNTAX trial which is well into the recruitment phase.
Pharmacology
Preloading with clopidogrel and aspirin is routine for coronary interventions and this applies equally to bifurcation disease. Additional elective use of glycoprotein IIb/IIIa inhibitors is currently considered the optimal pharmacological approach, but use of these drugs is decreasing, and further data from the ISAR REACT study series6 could potentially influence activity further.
One of the main concerns with bifurcation stenting, particularly if a double stent technique is used (either deliberately or as the final phase of a provisional T-stent strategy) is of SubAcute stent Thrombosis (SAT). Using drug-eluting stents, SAT may be more common with complex stenting techniques, as it was in the BMS era7. There is a suggestion from the “Research” and “T-search” Registries8,9 that routine use of Gp2b3a inhibitors with complex bifurcation stenting may reduce the rate of SAT. However there is no data showing that late stent thrombosis after complex stenting is reduced by the adjunctive use of antiplatelet treatment10.
It is not likely that any randomised trials will be performed with a primary end-point of SAT. It could be that large “real world” registries (such as the Medtronic “E5” using the Endeavor™ stent and the Boston Scientific “Olympia” registry using the Taxus Liberte™ stent) could at least provide the incidence of SAT with the use of DES in bifurcation disease.
Imaging and QCA of bifurcation lesion
Imaging of bifurcation coronary disease remains problematic. Multiple 2D imaging planes may be required before a clear image of the bifurcation is achieved, and in some cases, optimal imaging of the bifurcation is never truly achieved due to poor ostiale visualisation of the side branch and/or foreshortening of the vessel. Recently, Ludwig et al have been experimenting with novel 3D reconstruction software, to offer superior anatomical assessment of the bifurcation lesion, and also to calculate the optimal caudal/cranial and left/right angulation required to best visualise the bifurcation. This technology (Paieon Medical Ltd, Israel) was enthusiastically received at the meeting. Intravascular ultrasound has taught us the importance of kissing balloon inflations following complex bifurcation stenting11, but is not itself considered necessary for the correct undertaking of bifurcation angioplasty. The importance of understanding the Murray’s law12 was clearly pointed out by Gérard Finet from Lyon, France who confirmed in vivo the mathematical relationship between the diameter of both branches (MB and SB) of the bifurcation and the Proximal Branch (PB): PB (mm) = (MB+SB) x 0.67 (in a constant flow model this ratio is 0.71).This formula can be very useful for evaluating the correct proximal reference diameter in a bifurcation lesion, especially for distal left main. It can be used also to determine the reference diameter of the side branch when diseased (knowing the proximal and distal main branch reference diameter). This rule is now used in a new experimental QCA software which was presented by General Electric. Medis has also developed a new software dedicated to analysis of bifurcation lesions.
Plaque modification
One of the major problems during percutaneous treatment of bifurcations is plaque shift. There is therefore a theoretical advantage to including plaque modification in the strategy. There are proponents of various techniques, including use of the cutting balloon13, rotablation14 and atherectomy15. None, however, has clearly been shown to be beneficial in any randomised trial of technique, and there remains no consensus about the value of these ancillary techniques.
Technique
There are many described techniques for the treatment of bifurcation lesions. These include; main-vessel-only stenting, provisional side branch T-stenting; T-stenting, modified T-stenting, culotte, crush, V-stenting, shotgun and simultaneous kissing stents16. Many of these techniques are minor variations on a theme and provisional techniques may still end up with complex stenting17. An attempt to classify these treatments into types A-D has been made16. Randomised trials are difficult to do: each patient’s anatomy may favour a particular technique, but trial patients overall will be heterogeneous. During the first European Bifurcation Club meeting the following comments were made by experts in the field:
“It may be impossible to do randomised trials: every patient needs an individual treatment.”
“Every technique is potentially provisional when using type B treatment (first stenting the main branch), we can do a provisional culotte, provisional T, provisional crush...”
In the era of bare metal stents, consensus would appear to favour the “simple” (attempted single stent) approach, compared to the complex (planned double stent) approach. No randomised data is available, but several registries appear to favour the “provisional” T stenting approach2-15. Difficulties with these registries include:
– They are often not assessed with an intention to treat manner.
– Side branch stents are often placed as a result of poor results or complications. Therefore a systematic bias favours the single stent patients, as they have “easier” lesions with better initial outcomes.
– The techniques used for double stenting vary from registry to registry. Even the names of the techniques, as well.
– The classification of the bifurcation types and treatment is not always clear.
Despite these shortcomings, the recurring theme of these registries is that for bare metal stents, deliberate double stent techniques are not superior, and may be inferior, to attempted single stent techniques involving provisional treatment of the side branch. In the era of drug-eluting stents however, given the very low rates of restenosis of these stents, it will be important to re-examine this issue.
Data so far for the more complex techniques employing drug-eluting stents are limited. The Colombo trial utilising sirolimus-eluting stents is difficult to interpret, as there was a very high crossover rate from single to dual vessel stenting. Per-protocol angiographic restenosis (>50% in either vessel) was seen in 28% of the stent-stent versus 18% of the provisional stent group18. In the randomised study of Pan et al19, a very low rate of cross-over was observed but the trend was the same: a higher rate of restenosis, TVR and MACE in the 2 stents group.
If a complex strategy is employed, kissing balloon angioplasty is an important final part of the procedure20,21 both to reduce restenosis at the ostium of the side branch, and possibly to facilitate future access to the side branch. However, recrossing a stent crush is not always possible.
If a simple technique is employed, immediate patency of the side branch is more easily achieved with a wire jail than without22. Certainly, the 2nd wire favourably modifies the angle between the 2 vessels23, and is a good marker of the side branch should it occlude during stenting of the parent vessel. There are no data, however, to establish clearly whether a kissing inflation is necessary with the provisional T-stent strategy if there is good flow in the side branch after initial deployment of the stent in the main vessel.
How can this field be moved forward from “anecdotalism” to clinical science?
There are a number of options for clinical trials which will allow the delineation of the optimal treatment of bifurcation coronary disease:
Philosophical
There are two potential areas where a philosophical approach in bifurcation disease could be tested. The first would be a trial of percutaneous intervention versus coronary artery bypass grafting. However, as percutaneous intervention has advanced, so it has become more difficult to randomise patients into this type of trial, and although there are several ongoing trials randomising patients to either an interventional or a surgical management of their coronary disease, it is doubtful that a randomised trial of surgical versus interventional management of LAD/diagonal bifurcation coronary disease could successfully take place.
The second potential for a “philosophical” trial would be one comparing “flow” versus “anatomy”. The most simple approach to a bifurcation lesion is to stent the main vessel and only intervene on the side branch if the flow in the side-branch is compromised. This could be compared to a strategy requiring angiographic anatomical optimisation, such that no stenosis of >50% could be left untreated “per protocol”. Two such studies are currently being performed, each at differing levels of completion. The Nordic Bifurcation Study has enrolled 400 patients with bifurcation disease. Randomisation is between a simple (provisional side branch T-stenting) and a complex strategy (crush, culotte or T stenting with final kissing balloon inflation) using the Cypher stent. The primary endpoint is a composite of death, myocardial infarction, and target vessel revascularisation, at 6 months, with an additional angiogram at 8 months. This nice design allows clinical endpoints to take priority, while also providing subsequent angiographic data. The BBC ONE study is being performed in the UK. This will compare simple (provisional T with final kissing) and complex strategies (crush or culotte with final kissing) in 500 patients using the Taxus stent. The primary end-point in this study is a composite of death, myocardial infarction and target vessel failure at 9 months. Between them therefore, these 2 studies will include nearly 1,000 patients randomised to simple or complex strategies, and are sufficiently similar to allow possible meta-analysis. Hopefully, this will give a clear answer as to the correct baseline strategy for bifurcation coronary disease, and indeed may hint as to whether one drug-eluting stent has an advantage over another.
Physiological
The alternative approach would be to assess the physiological significance of any residual or “new” lesion in the side branch, following plaque shift, using pressure wire derived Fractional Flow Reserve (FFR). This might present technical difficulties manipulating the pressure wire through the parent vessel stent. Also, immediate pressure-wire derived assessment may not be representative of the physiology of the side branch ostium over time – pressure wire data were initially derived from chronic stable anatomy, and the anatomy of a recently stented bifurcation does not conform to this. Some data, however, has been presented with this technique, “jailing” the pressure wire during the procedure, and suggests that angiography alone is unreliable in assessing the functional severity of jailed side branches – many side branches with a >75% angiographic stenosis had an FFR >0.75 suggesting that no further intervention was required24. To try to answer this question a prospective randomised study will be designed.
New devices
Dedicated bifurcation devices have had only moderate success so far25 in bare metal format, but may yet prove useful, particularly for the left main stem when the DES format is available. One device currently being assessed is the Devax stent (Axxess Plus study), a unique self expanding stent which is deployed in the parent vessel (carena device), followed by distal stenting in the main and/or the side branch as required. Preliminary data with this device are very promising and a First-in-Man study with a Devax left main DES carena device is now ongoing.
A number of dedicated stent designs in DES format are in development (dedicated provisional T approach devices: Twin-Rail, Frontier, Petal, sidekick, Nile; Side branch stents: Capella, Tryton; and carena devices: Axxess plus). When mature, they may offer an advance in bifurcation treatment options, particularly with respect to the left main stem. Randomised trials of these devices appear unlikely and we may well have to rely on registry data to decide on the relative merit of each new device.
Conclusions
Randomised trials in bifurcation coronary disease are difficult because of the heterogeneous nature of the anatomy of bifurcations. A consensus view of the definition of bifurcation anatomy would be very useful and the MEDINA classification would appear to provide this. Registry data may be required to assess complication rates such as subacute or late stent thrombosis. Randomised trials of a “simple” versus a “complex” approach are, however, possible and two such trials are currently under way. In the absence of randomised data to the contrary, a “simple” approach to bifurcation lesions would seem to be reasonable. If one technique is shown to be superior to the other, then subsequent new devices could be assessed in a registry format against this gold standard. The left main stem presents a particular challenge to the interventional cardiologist. The SYNTAX trial should offer a baseline for interventional therapies in this area – this cohort could then, again, be tested against new devices using the SYNTAX group or the Bifurcation group of patients included in ARTS II26 as historical controls.
Much work remains to be done in percutaneous treatment of coronary bifurcation lesions. However, gradually some consensus appears to be emerging in this difficult field and we are hopeful that a standard approach will emerge over the next 3-5 years.
Consensus was reached on the following issues
– The MEDINA classification should be more widely adopted (see Figure 1)
– With bare metal stents, a stepwise provisional T-stent strategy is the gold standard
– With bare metal stents, deliberate double-stenting may be an inferior technique
– With drug-eluting stents, the optimal strategy is under development, and two ongoing trials (Nordic and BBC1) will help define this.
– After complex stenting, kissing balloon inflations should be routinely performed.
There is still debate
– A precise, simple and easy to retain definition of treatments is still necessary.
– In bifurcation lesions with no significant side branch involvement should we end always with a kissing or jail the side branch?
– Is the answer different for distal left main?
In true bifurcation lesions with relatively long side branch lesion (> 3 to 5 mm in length), there is a consensus for the use of 2 stents but what is the best treatment with 2 stents: T stenting, minicrush, crush, culotte?
Maybe the answer will come, not only from randomised studies, but also from bench testing?

