Abstract
Aims: During coronary angiography and percutaneous coronary interventions (PCI) only the lumen of the coronary vessel is imaged. The complete pathology of the vessel wall – namely the extent of calcification, structure of non-calcified plaque and lesion length – cannot be accurately determined. These can be imaged using coronary CT angiography (CTCA). We aimed to investigate the accuracy, feasibility, safety and value of a novel hybrid method encapsulating real-time registration of CTCA to coronary angiography images. The method is designed to seamlessly integrate into the routine catheterisation procedures and provide information to assist in decision making during the interventional procedure.
Methods and results: Phantoms simulating the coronary tree were used to test the accuracy and potential of co-registration of information. Precision of the imaging system was tested using radio-opaque markers and distance between bifurcations. We included patients who underwent CTCA and also underwent cardiac catheterisation. Analysis and feasibility was performed offline in the first twenty patients and online in the following 19 patients. The online CTCA and angiography co-registration was performed by the AngioCt software program. The registration result was displayed on a separate screen in the catheterisation laboratory as a three-dimensional coronary tree and a curved multi-planar reformat (MPR) view.
Preclinical validation showed that the co-registration of the coronary tree is feasible, and measurements of length and diameter are precise for all standard working angulations during coronary angiography. Real-time registration was successful in all cases and aided in selection of the view that will provide the least foreshortening and no vessel overlapping, the length of balloons and stent to use and assisted in crossing chronic total occlusions (CTO).
Conclusions: This is the first report of a novel method for online real-time hybrid CTCA and angiography registration. In this pilot study we found that this method is feasible, accurate, and easy to use. It can be used for selecting the best working angulations for minimising foreshortening and vessel overlapping, determining stent size and location, and providing a reference vessel path and structure in cases of CTO.
Abbreviations list
PCI: Percutaneous coronary intervention
CT: Computerised tomography
MDCT: Multi-detector computerised tomography
CTO: Chronic total occlusion
CTCA: coronary CT angiography
MPR: Multi-planar reformat
IVUS: Intravascular ultrasound
QCA: Quantitative coronary angiography
PACS: Picture Archiving and Communication Systems
Introduction
Currently, radiology and cardiovascular interventional procedures that are based primarily on lumen appearance are the standard method-of-care. The vessel wall composition – calcified, non-calcified plaque and lesion length – cannot be accurately determined with angiography1-4. Multi-detector computerised tomography (MDCT) is increasingly used for the diagnosis of coronary disease5-8 and can provide additional information on plaque distribution that may not be appreciated on angiography9-13. We sought to further improve the information that can be obtained during an interventional procedure by combining in a fast, user-friendly and accurate method, information obtained from the MDCT coronary angiography (CTCA) with angiography information into the catheterisation laboratory.
We present the accuracy, feasibility and safety of a novel method of real-time hybrid CTCA and angiography image registration with preliminary clinical experience.
Methods
The study was approved by the local Institutional Review Board committee for human studies. Angiography was performed on a Siemens AXIOM Artis dTC CathLab.
The computerised tomography (CT) scanners used in this study were either a Philips Brilliance 64-channel CT (n=30) or a GE LightSpeed VCT 64 slice CT (n=9). The scanning parameters used were: detector collimation 64 x 0.625 mm; rotation time 380 ms; tube voltage 120-140 kV at 400-500 mA. Dose modulation was used when appropriate. The spatial resolution was 0.5 mm. Contrast enhanced datasets were acquired after injection of 80-90 ml of non-ionic iodinated contrast material (Iopamiro® 370 mg/100 cc) at a rate of 4-5 ml/sec using a power injector. An automated bolus tracking system was used to synchronise the arrival of the contrast agent in the descending aorta (2 cm after the subclavian artery) with the initiation of the scan. All scans were performed during an 8-12 seconds breath-hold. Beta blockers (IV Metoprolol 5-10 mg) were used when the heart rate was above 70/min. The median heart rate during this study was 62 (range 40-82).
Axial datasets were reconstructed retrospectively from ECG-gated raw-data at up to 10 phases of RR-interval (slice thickness and increment: 0.9/0.45 or 0.67/0.33 mm), the best phase (usually 60% or 75%) was transferred via network connection from the picture archiving and communication systems (PACS) to a remote workstation (CardioCt, Shina Systems, Caesarea, Israel) for further processing and analysis. The CardioCt application reconstructs the coronary tree by marking the vessel centrelines and vessel walls, which are the basis for displaying the three-dimensional (3D) coronary tree and a curved multi-planar reformat (MPR) of each coronary artery. The algorithms for reconstructing the coronary tree have been clinically validated and verified.
Given a CT dataset, success of registration was defined by three criteria:
a. Software-level compatibility of CT data with the angio data is a basic requirement to actually combining the two datasets (ECG, same patient, saved segmentation is available).
b. The software is able to overlay the registration lines over the angio image; as the software relies on coordinates placed by the user to construct an optimal registration, there is a minimum threshold of accurate point placement, beneath which it is impossible for the software to perform registration and overlay.
c. The subjective judgement of the user, based on the user’s knowledge of the patient’s anatomy. The user may fine-tune the initial registration until satisfactorily performed.
Work scheme
AngioCt (Shina Systems, Caesarea, Israel), introduces a novel approach of integrating angiography and CT data. The software is designed to be integrated into regular catheterisation procedures. The patient has to undergo cardiac CT before the angiography. The system collects the CT data and 3D images are then constructed and displayed as discussed above. This data is initially stored on the PACS. If there is a network connection between the AngioCt workstation and the PACS, the data maybe loaded via the network. Otherwise it may be transported on portable media to be used for registration at the time of the coronary invasive angiography. AngioCt is dependent upon a pre-processing program to convert the CT data into a 3D model built from the centreline and the vessel wall data, which is the basis for software’s function.
After suitable angiographic images are recorded as a cine, a still frame out of the cine is selected in the same phase as in the CT scan – usually in diastole (phase at about 60%-75%), where the coronary arteries are relatively relaxed, and the target vessel is best demonstrated. The designated angiogram is displayed on a separate screen. The CT-derived 3D images of the same artery are displayed on a split screen in the same orientation as the angiographic image (Figure 1A).
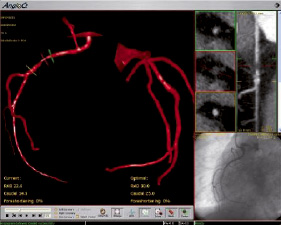
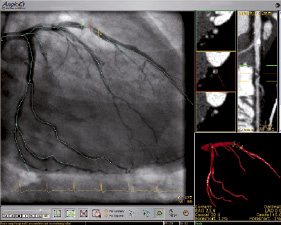
Figure 1. Appearance of the images on the separate computer screen for integrated visualisation of CTCA and angiography data and its co-registration. A. The CT 3D appearance. B. The registration is done on a separate screen and by using markers, the operator can “scroll” along the vessel. The CT image of the vessel can be seen on the right-hand side of the screen as long axis or short axis (IVUS like) images.
Reference points are then marked on both the CT and the angiographic images to facilitate identification and orientation. Once successfully oriented, the CT data is projected over the angiographic data (Figure 1B) as vessel centrelines. The overlay of the CT data still frame is done on a still frame reference image of conventional angiography and not on the live fluoroscopy image.
The operator can then scroll along the angiographic image of the vessel and see the lumen wall composition on the corresponding MPR reformatted view of the CTCA of the same vessel. The operator can follow the occluded vessel segment in cases of a total occlusion and can determine the best C-arm working angulations for least foreshortening and for the best view of the lesion without vessel overlap. Acceptable foreshortening was defined arbitrary as less than 10%. The entire registration process takes typically less than 30 seconds.
Phantom studies
Phantoms (n=2) that simulated a representative coronary network with different tube diameters filled with diluted iodinated contrast and several radio-opaque markers at defined locations were used for proof of concept and accuracy experiments. The phantoms had several bifurcations whose distances from each other were known. Both phantoms were static.
The phantoms underwent both CT scans and fluoroscopy using catheterisation laboratory table. Cine-angiography images from 10 frequently used angulations during diagnostic coronary angiography were collected. The diameter of the tubes and distance between the markers and bifurcations using CT and angiography were compared. Feasibility to integrate information was tested for accuracy and precision.
Registration studies
Registration studies were initially performed offline, and after obtaining data on feasibility, they were performed online at the time of catheterisation. Data from 20 patients who underwent CTCA was used to test the system. Their corresponding angiograms were taken. The feasibility was analysed by choosing a single angiographic run, marking the reference points and allowing the CT data registration and overlay on the corresponding computer monitor.
The registration was performed by two experienced interventional cardiologists to test the time and accuracy it takes to create the overlay.
Real-time registration
After testing the system ex vivo, we examined it online in the catheterisation laboratory. Connecting with the AngioCt system was done using an extra data output port of the Siemens AXIOM Artis dTC DICOM output data channel. The connection was done in parallel to the normal work flow of the system, and did not influence the normal data collection and the archiving of the clinical catheterisation laboratory and its routine work. The connection enabled direct access to archived images for display in the examination room, thereby facilitating diagnoses during procedures.
Study population included consecutive patients who were referred for coronary angiography and who underwent clinically guided CTCA scans. Each participant gave their signed informed consent. We report here on the results that were obtained from the first 19 patients with online registration which was done using the above-described methodology.
Statistical analysis
Categorical data are presented with absolute frequencies and percentages. Simple student T Test analysis was performed to test the agreement between the modalities. Values of P < 0.05 were considered to reveal significant statistical differences. All tests were performed with the SPSS 12.0 (SPSS Inc., Chicago, ILL, USA) statistical software.
Results
Phantom studies
The CT images of the phantoms obtained using the AngioCt software were able to correctly detect the representative coronary network with different tube diameters filled with diluted iodinated contrast. The phantom images showed accuracy that was similar to the spatial resolution of the CT. The diameter of the phantom’s vessel measured on CT was equal to the actual diameter in the phantom (2.0±0.03 mm Vs 2.0±0.05 mm and 3.0±0.05 mm Vs 3.0±0.04 mm p=NS). For length, error of the measurement (n=29) of the radio-opaque markers and the distance between the bifurcations were less than 4% of the actual distance (25.0±0.05 mm vs. 25.4±0.03 mm p=NS).
Registration studies in patients
Offline analysis on data from 20 patients who underwent both CTCA studies and invasive coronary angiography revealed that the system is feasible and easy to use. The registration was performed by two experienced interventional cardiologists. Both registrations were accurate. Registration time was less than 30 seconds for all cases (average 25±3 and 24±5 seconds, p=NS).
Real-time registration
Real-time registration was performed as described in the methods section of this paper. The interval between the CT scan and coronary angiography was 6-21 days. The CT data was reconstructed offline using CardioCt before catheterisation. The data was displayed on a separate screen and did not influence the normal work flow of the catheterisation procedure. The registration process took less than 30 seconds in all 19 cases, during which, the operator could continue with the procedure. Upon registration, the 3D reformatted coronary tree was derived from the CTCA facilitated choice of working angulations without overlapping of segments and in order to choose the best separation of coronary artery bifurcations (Figures 1, 2).
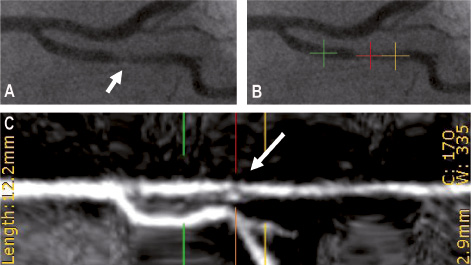
Figure 2. Stent size and location planning using the hybrid registration system. A. High-power image of the region of interest (ROI) of the original angiography image (white arrow). B. CTCA-to-angiography registration allows AngioCt to provide a recommendation on stent size and location of its placement during the catheterisation procedure. The operator may scroll along the vessel. The red marker is the centre reference marker, while distance is measured between the green and yellow markers. C. Investigation of the selected ROI on the CT image (white arrow). By looking at the CT image, one can identify the real composition of the stenosis and the type, location and size of the plaque that caused the stenosis.
For the purpose of this article, there were five cases of CTO: One short lesion with non- calcified plaque, and four mixed plaque sites. The registration was successful in all cases. The registered images were used for determining the best angulations for visualising the path and composition of the missing segment and as a reference for orientating the wire direction. Successful recanalisation was achieved in three cases and failure occurred in two cases due to heavy calcification and long totally occluded segments (Figures 3 and 4).
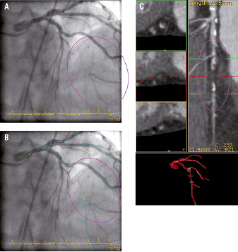
Figure 3. CTO - Path and composition A. Original angiography image in which significant stenosis can be seen. B. Composition of the CTO, in which only non-calcified plaque bulk with minor calcifications is seen. C. As a result of CTCA-to-angiography registration, AngioCt projects a 3D image of the coronary tree onto a 2D angiographic image. The generated projection shows the nob visible direction of the vessel and may serve as a guide for treating CTOs.
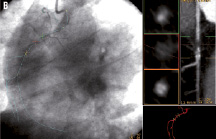

Figure 4. CTO – Planning and guidance. A. Original angiographic image in which significant stenosis can be seen. B. As a result of CTCA-to-Angiography registration AngioCt projects a 3D image of the coronary tree onto a 2D angiography image. The generated projection shows the non visible direction of the vessel and may serve as guidance roadmap for CTO treatment. C. The result of a successful catheterisation using the AngioCt software.
Foreshortening and stent implantation
Offline analysis found that 10 stents (50%) were placed under high foreshortening C-arm orientation (>10%). This information was used for the online registration in which the original angulation, which had been planned for the procedure by the interventional cardiologist, was changed to a different C-arm position with less foreshortening in 6/19 (31%) cases (Figure 1A).
Plaque coverage and stent misplacement
In the offline analysis, we observed that only part of the plaque as seen by CT was covered by the implanted stent in several cases and left a diseased portion of the artery uncovered. There were 11 non-calcified plaque sites, out of which four were partially covered (~36%), while in three sites, the stent was placed more than 4 mm from the end of the plaque, i.e. possibly covering healthy segments (~27%). There were nine composite (calcified & non-calcified) plaques, where one non-calcified plaque site (~11%) and three additional calcified plaque sites (~33%) were partially covered. In the online registration, all stents implanted covered the plaque.
Technical failure
There were three additional patients with low quality CT scans. In these patients plaque composition in the suspected coronary vessel could not be determined, due to movement artefact (n=2) or calcifications (n=1); therefore the registration was not performed, and they were not included in the online study. In one of the 19 online patients, the CT missed the diagnosis of a 2 mm short ruptured plaque which had been diagnosed as a heavily calcified plaque from the CT images.
Discussion
This report describes a novel method for real time hybrid CTCA and angiography registration during coronary interventional procedure in the catheterisation laboratory. In this pilot study, we found that this imaging system is feasible, simple to use and accurate. It can be used for selecting the best working angulations for minimising foreshortening and vessel masking, determining stent dimensions and positioning.
MDCT can often give a more complete view of coronary vessel pathology because it includes evaluation of the lumen and can determine the amount of non-calcified, plaque and the calcified plaque burden in the coronary vasculature2-14. In cases of CTO, the system assists procedure planning by providing a reference vessel path and suggesting composition of plaque13.
The correct measurement of length of the coronary lesion during fluoroscopy depends on the C-arm angulation, which affects the projected view of the target vessel. Thus, arteries are almost always foreshortened to some degree when view angiographically. In CT, however, the exact length of the lesion can be measured accurately. We show that foreshortening can be improved by the software’s optimal C-arm orientation recommendation. Also, stent misplacement can be reduced to minimum, thus enhancing the potential clinical benefit of stent therapy.
Several angiography systems have the ability for two-dimension-to-3D reconstruction methods that allow creation of 3D coronary tree model during catheterisation procedure. Construction of 3D images from 2D images methods are the basis of novel 3D QCA systems9,10 and these systems are successfully used today around the world as complementary systems for angiography. The 3D model allows measurement of stenosis area length, but is reported to have significant accuracy error (up to 10%)11,12. These systems can not be used in cases of CTO and do not visualise plaque sites.
CTCA is an offline method of data collection and processing and can be successfully used for offline diagnosis. The advantage of the real-time CTCA-to-angiography registration is that the operator can visualise the lumen appearance and scroll along the vessel in 3D. The online real-time imaging capabilities of CTCA-to-angiography registration during the catheterisation procedure add important data.
“IVUS-like” views of the vessel from CT data can be obtained. Such an image can also be obtained for a completely occluded segment of the coronary artery, whereas IVUS cannot contribute unless the occluded segment was already crossed with a wire and with the IVUS catheter.
Chronic total occlusions
Among other decision factors, the software provides integrated information about the CTO area such as the vessel path and the CTO composition. Therefore, this can serve as an important tool to assess the feasibility of crossing the lesion and guide the decision whether to intervene. In cases of a heavily calcified lesion, or very long segments, one might decide not to intervene (Figure 3). In cases where only non-calcified plaque is present in the occluded segment, the operator can use this data to help in deciding which equipment to use during the procedure (Figure 4). The method provides a priority knowledge about the length and direction of the occluded vessel segment, can help guide the wire through a tortuous segment of the occluded artery and may improve the confidence level of the cardiologist when approaching the treatment of CTO.
Limitations
Only patients with previous CT images of high quality can be included and are eligible to benefit from this novel imaging modality. The system has the absence of live overlays. Due to CT reconstruction only diastolic images can be used. Low quality CT images, where the plaque composition or the vessel anatomy is not clearly defined, cannot be used. CT is associated with prior exposure to X-radiation which poses a limitation to its use. However, if CT was performed for any reason prior to the intervention, it can be used in the catheterisation laboratory and by combining it with the system presented here, it may reduce radiation in the catheterisation laboratory and contrast injections, the overall duration of the procedure and enhance the precision of interventions.
Future directions
The CT scanners that are being currently developed are becoming extremely fast, with lower radiation by using only diastolic phase sampling. Future developments in technology will include larger detector arrays, such as 256-detector arrays or so-called “flat panel” scanners, all of which will have increased spatial resolution. They would theoretically be able to image the entire coronary tree during a single heartbeat.
Future directions of the hybrid registration technology will include a CT next or in the catheterisation laboratory. Ultimately, real-time moving image registration will need to be developed. The whole system will be linked to navigational tools in three dimensions. By doing this, it should be possible to more efficiently pass wires and other equipment through complete occlusions and in tortuous vascular segments. Other applications may include peripheral interventions and carotid stenting.
Summary
During regular catheterisation procedures, the cardiologist has very limited information regarding the vessel wall. AngioCt performs registration of CT angiography vascular 3D data with a coronary angiography (CT-to-angiography registration). The registration image provides the cardiologist information for performing coronary vessel catheterisation, such as optimal C-arm orientation angles for minimising foreshortening and vessel overlap, stent size and location, and vessel road map and composition in cases of CTO. It enables the cardiologist to “see” beyond the lumen and to understand the 3D nature of the vessel and the stenoses. Furthermore, it enables to precisely identify the location of the stenotic plaque on the angiographic image.
Acknowledgements
The authors thank Shina Systems Ltd. for providing AngioCt and CardioCt software products for clinical evaluation and research.
Ariel Roguin is supported by the Morasha program of the Israel Science Foundation (Grant 1831/07), the Mallat family award for biomedical research, the Samuel Mendel Chodowsky Fund, and the Chief Scientist’s Office of the Ministry of Health, Israel.

