Abstract
The aims of this study were firstly to evaluate the relations between N-terminal pro-brain natriuretic peptide (NT-proBNP) concentration after ST-segment elevation myocardial infarction (STEMI) and reperfusion injury, and secondly to assess the prognostic value of NT-proBNP.
Methods and results: We evaluated 202 consecutive patients with STEMI treated with facilitated angioplasty (PCI). TIMI flow, TIMI myocardial perfusion grade (TMPG) and ST-segment elevation resolution (iST) were assessed before O and 30 minutes (O30) after PCI. Enzymatic injury was expressed as an area under the curve of CK-MB release (AUC, [Uxh]). 48 hours after PCI, the concentration of NT-proBNP ([pg/ml]) and echocardiography-determined left ventricle ejection fraction (LVEF, [%]) were assessed. Death and heart failure (HF) requiring hospitalisation were recorded during a 1-year follow-up and defined as a composite endpoint. NT-proBNP concentration 48 hours after PCI was correlated with iST-O (p<0,001; r=0,48), iST-O30 (p<0,001; r=0,57), AUC (p<0,001; r=0,54) and LVEF (p<0,001; r=-0,5). Increasing quartiles of NT-proBNP were related to mortality (p=0,0012) as well as to composite endpoint (p=0,0012) at 1 year. 4th-quartile of NT-proBNP was independently associated with a composite endpoint at a 1-year follow-up.
Conclusions: NT-proBNP level after STEMI was moderately correlated with the degree of microvascular reperfusion and myocardial injury and function. NT-proBNP was independently associated with the frequency of death and HF requiring hospitalisation.
Introduction
The precise assessment of coronary and tissue reperfusion during myocardial infarction is crucial in predicting infarct size1, left ventricular injury2 and function1,2 as well as short- and long-term clinical outcome2-4. The current position of various diagnostic techniques in the assessment of reperfusion therapy efficiency, including ST-segment elevation resolution (STR)5,6, cardiac necrotic markers7,8, angiographic methods (TIMI flow scale9, TIMI myocardial perfusion scale3, myocardial blush scale10), is well established.
B-type natriuretic peptide (BNP) is produced as a prohormone (proBNP) and is predominantly synthesised in, and secreted from, cardiac ventricles in response to volume overload and increased cardiac filling pressure11,12. Circulating proBNP is cleaved into an active fragment and N-terminal pro-brain natriuretic peptide (NT-proBNP)13,14. The value of BNP is well established in the diagnosis, risk stratification and prognosis of patients with heart failure15-18. Recently, the measurement of BNP has also been proved to constitute a useful prognostic tool in patients with acute coronary syndromes including ST-segment elevation myocardial infarction (STEMI) population19-22. Nevertheless, the relation of coronary recanalisation, tissue reperfusion, left ventricular injury and function to brain natriuretic peptide level has not been investigated in the setting of STEMI.
The aims of this study were firstly to evaluate the relations between N-terminal pro-brain natriuretic peptide (NT-proBNP) concentration after STEMI treated with facilitated angioplasty (PCI) and microvascular and myocardial reperfusion injury, and secondly to compare the prognostic value of NT-proBNP to another reperfusion parameters.
Methods
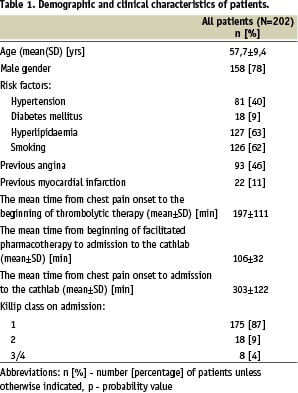
The study group consisted of 202 consecutive patients (mean age 57,7±9,4 years, 44 women) with STEMI who underwent facilitated PCI at our institution. Patients were enrolled to this study if they were under 75 years, with chest pain onset within 12 hours and with ST-segment elevation of > 1 mm in > 2 contiguous leads or with recent LBBB. The expected transport time from a local hospital to the cathlab had to be more than 90 minutes. Patients were excluded in cases of lack of patient’s consent, absence of femoral or radial pulse, cardiogenic shock, aortic dissection, acute mitral regurgitation, disruption of interventricular septum, single reliable measurement of SBP>180 mmHg or DBP>110 mmHg, known prior history of stroke, transient ischemic attack, active bleeding or history of haemorrhagic diathesis or surgery prior 4 weeks.
All included patients with STEMI received 300 mg aspirin in a local hospital, a weight adjusted bolus of UFH in a dose 50 U/kg, and underwent the lytic therapy which consisted of a bolus 15 mg of actylise followed by an infusion of 35 mg per 1 hour and abciximab in a dose of 0,25 mg/kg in a bolus i.v. followed by an infusion of 0,125 µg/kg/min per 12 hours. The mean time from the chest pain onset to beginning of the lytic therapy was 197±111 min. After the beginning of the lytic therapy all the patients were transferred to the cathlab. Immediately after an admission coronary angiography was performed in all the patients. Out of 201 patients 25 did not required angioplasty because of TIMI-3 blood flow in all epicardial arteries. In 21 cases there were no significant stenosis and in 5 there were multivessel disease requiring coronary artery bypass grafting. Coronary artery stent implantation was performed in 90 (51,1%) patients. After stent placement the patients received clopidogrel (300 mg) followed by ticlopidine (250 mg b.d. for four weeks). All the patients were put on a statin. Beta-blockers and angiotensin-converting enzyme inhibitors were started as soon as the haemodynamic status permitted, usually within the first 24 hours.
Angiographic assessment of coronary blood flow and myocardial perfusion
Epicardial blood flow in infarct related artery (IRA) was evaluated by means of the TIMI (Thrombolysis in Myocardial Infarction) scale9 and myocardial perfusion was assessed by means of the TIMI Myocardial Perfusion Grades (TMPG)5. In addition, angiograms were analysed for the presence of flow-limiting lesions in non-IRA. A detailed evaluation was performed in two contralateral projections for each artery before and after angioplasty. Two experienced investigators reviewed each coronary angiogram in a blinded fashion. In case of a lack of agreement between the two investigators, a third one was sought, and a conclusion was achieved (Table 3).
ECG
Standard 12-lead ECGs were obtained before angioplasty [B] and 30 minutes after the opening of IRA [O30]. The sum of ST segment elevations in all leads (ΣST) was measured 20 ms after the J point by a single investigator blinded to the clinical and angiographic findings. The percent reduction of ST-segment elevation from baseline ([B] - before the beginning of a combined pharmacotherapy) to an admission to the cathlab (iST-O) and to 30 minutes [O30] after facilitated angioplasty (iST-O30) was calculated according to the formula: iST-O=ΣSTO/ΣSTB and iST-O30=ΣSTO30/ΣSTB. Moreover, the percentage of patients with complete ST resolution (> 70%), partial ST resolution (30-70%), and no ST resolution (< 30%) was assessed according to Schröder’s 3-component definition5,6.
Measurement of NT-proBNP plasma levels
Blood samples were collected 48 hours after angioplasty in EDTA-containing tubes. The samples were then spun at 3000 rpm for 10 min at 0°C. The plasma level was then extracted and frozen in aliquots at –140°C until an analysis. NT-proBNP was measured using an electrochemiluminescence immunoassay kit (Roche Diagnostics) on an Elecsys 2010 analyser. The clinicians involved with in the patients’ care were blinded as to the NT-proBNP values obtained23.
Biochemical injury
Blood samples were collected on admission, every 6 hours in the first 24 hours and then after 36 and 48 hours. Biochemical injury was calculated as the area under the curve of CK-MB release in the first 48 hours (AUC [U/l x h])7,8.
Assessment of cardiac function
Two-dimensional echocardiography was performed 48 hours after coronary angioplasty at rest, for the evaluation of left ventricular ejection fraction (LVEF [%]) according to the biplane Simpson’s rule. The analysis was carried out by one observer blinded to the clinical and angiographic data.
Long-term follow-up
Patients were examined 1, 3, 6 and 12 months at the outpatient clinic. Follow-up clinical data included: death, recurrent MI, repeated PCI or cardiac surgery and heart failure (HF) requiring hospitalisation. The cardiac function of the survivors was assessed after 12 months according to the New York Heart Association functional scale. Death and HF requiring hospitalisation were defined as composite endpoint.
Statistical analysis
Statistical analyses were performed with the Statistica 6 (StatSoft, Inc). All continuous variables were expressed as the mean±SD, whereas categorical variables were given as absolute values, percentages, or both. ANOVA and post-hoc analysis with Scheffe correction were used to compare the differences between NT-proBNP concentration in relation to STR, TIMI flow and TIMI myocardial perfusion grade. Categorical variables were compared by 2 test or Fisher’s exact test. A single and multiple regression models were used for the elevation of correlations between NT-proBNP concentration and microvascular and myocardial reperfusion injury. A multivariate logistic regression analysis was performed to determine independent predictors of a long-term composite endpoint. Odds ratios and 95% confidential intervals were calculated. A p value less than 0.05 was considered statistically significant.
Results
202 patients with STEMI who were admitted to the local community hospitals without an on-site catheterisation laboratory were enrolled in this study (Table 1).
The time from the beginning of a facilitated pharmacotherapy to the admission to the cathlab ranged from 50 to 270 min, with a median of 100 min. During transport one patient with anterior STEMI died due to cardiac rupture (confirmed in autopsy), three patients developed pulmonary edema and five patients developed cardiogenic shock. The angiographic and procedural characteristics of patients with angioplasty is shown in table 2.
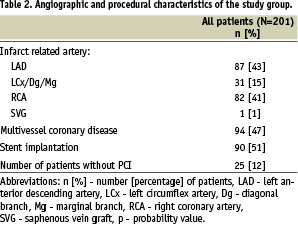
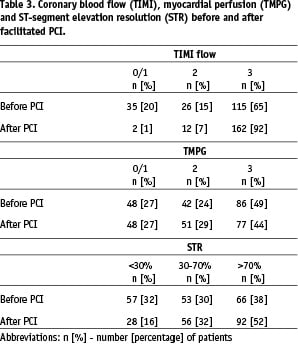
Reperfusion with facilitated angioplasty
Combined pre-cathlab pharmacotherapy restored TIMI-3 infarct related artery (IRA) flow in 140 (69,7%) patients. In patients with angioplasty TIMI-3 flow before PCI was observed in 115 (65,3%) and TMPG-3 perfusion was detected in 86 (48,9%) patients (Table 3). Final IRA opening (TIMI 2/3) was achieved in 552 (98,9%) patients. After PCI TMPG-3 was restored in 77 (43,7%) patients and the complete STR was noted in 66 (37,5%) before and 92 (52,2%) patients after PCI (Table 3).
The secretion of NT-proBNP after reperfusion
The level of NT-proBNP measured 48 hours after angioplasty decreased significantly with the improvement of TMPG before (p=0,0015) as well as after (p<0,001) angioplasty (Figure 1).
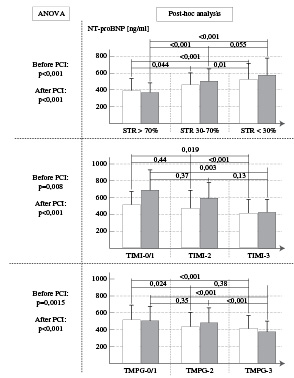
Figure 1. The NT-proBNP value in relation to STR, TIMI flow and TIMI myocardial perfusion grade.
Similar correspondence was observed in relation to TIMI epicardial flow and STR before and after angioplasty.
NT-proBNP concentration 48 hours after PCI was moderately correlated with the reduction of ST-segment elevation before PCI (p<0,001; r=0,48), with the reduction of ST-segment elevation after PCI (p<0,001; r=0,57), with enzymatic injury expressed as the area under the curve of CK-MB release in the first 48 hours (p<0,001; r=0,54) and with left ventricle ejection fraction 48 hours after PCI (p<0,001; r=-0,5) (Figure 2) in a single regression model.
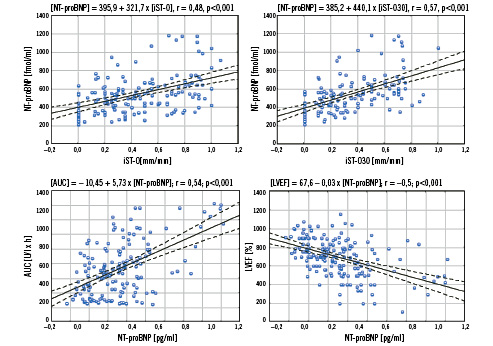
Figure 2. The correlation between NT-proBNP concentration and the reduction of ST-segment elevation after pharmacotherapy [iST-O], the reduction of ST-segment elevation 30 min after an angioplasty [iST-O30], CK-MB release in the first 48 hours [AUC] and left ventricular ejection fraction [LVEF].
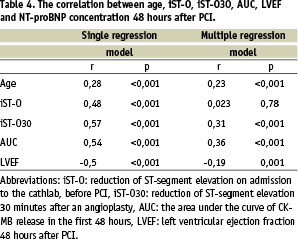
NT-proBNP concentration 48 hours after PCI was correlated with age, iST-O30, AUC and LVEF in a multiple regression model (Table 4).
Prognostic value of NT-proBNP
All values of NT-proBNP were divided according to quartiles. The upper limit for the first quartile was 340 pg/ml (n=43), for the second 430 pg/ml (n=43) and for the third 530 pg/ml (n=44).
The total one-year mortality rate was 4,5% (8/176). The unadjusted mortality rate after a 1-year follow-up increased directly across quartiles of NT-proBNP (p=0,0012) (Figure 3).
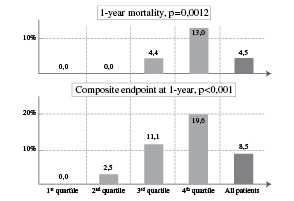
Figure 3. Mortality rate and composite endpoint defined as the frequency of death and HF requiring hospitalisation at a 1-year follow-up according to the NT-proBNP quartile.
During one-year follow-up 8 patients required hospitalisation due to symptoms of HF. The increasing quartiles of NT-proBNP were related also to a composite endpoint that reached 0,0%; 2,5%; 11,1% and 19,6% (p<0,001) respectively at 1 year (Figure 3).
Table 5 shows the multivariate predictors of a 1-year composite endpoint.
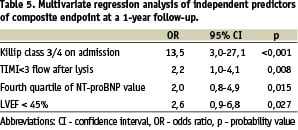
In the logistic regression model Killip class 3/4 on admission, the fourth quartile of NT-proBNP, TIMI<3 flow after the lytic therapy and LVEF<45% were independently associated with a composite endpoint at a 1-year follow-up.
Discussion
The main finding of our study is that the plasma level of N-terminal pro-brain natriuretic peptide measured after an acute myocardial infarction (MI) moderately correlates with a degree of microvascular reperfusion evaluated by ECG and angiography, with myocardial injury expressed as necrotic enzyme release and with echocardiography determined left ventricle function. While the description of the third correlation has already been presented in the studies, a detailed description of the first two correlations has been presented for the first time in literature in this study. NT-proBNP measured 48 hours after an infarct, strongly correlated with early perfusion parameters, also in our study maintains its prognostic clinical value being an independent predictor of a long-term mortality and of the frequency of HF. Obviously, at this stage, unlike in ECG or angiography, the cut-off value of NT-proBNP, which could signify successful or failed tissue reperfusion, cannot be given.
Reperfusion with facilitated angioplasty
Facilitated PCI refers to a strategy of planned immediate PCI after an initial pharmacological regimen such as full-dose fibrinolysis, half-dose fibrinolysis, a GP IIb/IIIa inhibitor, or a combination of reduced-dose fibrinolytic therapy and a platelet GP IIb/IIIa inhibitor in order to enhance reperfusion or to reduce the risk of reocclusion. Clear recommendation criteria for this kind of reperfusion strategy have never been established24,25. Several randomised trials of facilitated PCI with a variety of pharmacological regimens are in progress. Presented study is an analysis based on the data from the registry of 202 consecutive patients treated with facilitated angioplasty in south-eastern Poland. This facilitated therapy was addressed to non-shock STEMI patients with expected transport time from a local hospital to the cathlab of more than 90 minutes.
It occurred that a combination therapy of reduced-dose of t-PA and an abciximab restored TIMI-3 flow in 65% of patients. Additional PCI, which was performed in the case of TIMI less than 3 flow or in the presence of significant stenosis even with TIMI-3 flow, enabled the achievement of a final TIMI-3 in 92% of patients. The complete resolution of ST-segment elevation was achieved only in 38% of patients due to a combined therapy and in 52% after an additional angioplasty. An interesting observation was made concerning TMPG in which the grades 2/3 were achieved in 73% of patients at the first pharmacological stage and an additional PCI did not improve this result.
NT-proBNP and reperfusion
What could be a potential mechanism accounting for a direct relation between the amount of NT-pro-BNP released during an infarct and the degree of restored epicardial blood flow and tissue-level perfusion? On the basis of many well documented experimental and clinical studies on HF it is known that the amount of BNP produced mainly by a myocardium depends largely on the cardiac chamber wall stretch and pressure overload. In a chronic HF the expression of ventricular BNP gene occurs and de novo peptide production is related to haemodynamic stress26.
Where does BNP released during acute ischaemia or an infarct come from? During an infarct the level of BNP may reflect not only the degree of cardiac filling pressure but also the size of necrosis or the severity of ischaemia. Within hours from the onset of MI the plasma level of BNP increased rapidly and markedly (100 times more than the normal level) as compared to that of ANP. The plasma BNP level did not correlate with a pulmonary capillary wedge pressure but is inversely correlated with a cardiac index27. From Sabatine et al study28 we know that BNP rises rapidly and transiently during an exercise test in patients with coronary artery disease, and the BNP amount increase was proportional to the size of an ischemic territory. In patients with non-ST elevation myocardial infarction, despite a complete pharmacological treatment, a refractory ischemia (but not recurrent MI) was associated with a repeated increase of NT-proBNP level29. It has also been shown previously that BNP level increased after an angioplasty, even when cardiac filling pressures remain unchanged30,31. Plasma BNP levels returned to the baseline values shortly after the end of the procedure31.
Summing up, during MI BNP can first be released immediately [in minutes] in response to ischaemia from the cardiomyocytes storage in a peri-infarct and an infarct areas. The second mechanism of BNP release starts with a delay resulting from the time needed to start de novo BNP synthesis in response to the increasing ventricle filling pressure. This hypothesis is supported by an observation in which a biphasic pattern of plasma BNP or N-terminal pro-brain natriuretic peptide is seen after MI with peaks at 14-48 and 121-192 hours32,33. Moreover, BNP level on admission was almost 40 times higher in patients with an infarct in comparison to the control group32, and remained elevated at 2 weeks after MI, also exhibiting a high level at the time of 4 weeks34. The time relation between the first BNP peak and the maximum of enzymatic myocardium damage cannot remain unnoticed. The second BNP peak most certainly reflects the start of post-infarcted remodeling process, the subsequent left ventricle enlargement and the filling pressure increase as a result29.
In the presented study epicardial reperfusion was assessed by TIMI scale and the degree of tissue-level reperfusion was evaluated indirectly by means of ST-segment elevation resolution and TMPG. The TMP grades rely heavily on the presence of the myocardial opacification as well as on the dye clearance rate during the washout phase3. It was previously confirmed that infarct size measured by means of a single photon emission computed tomography is related to TMP grades. Infarct sizes were significantly larger with TMPG-0/1 than with TMPG-2/335. In turn, the resolution of the sum of ST-segment elevation after reperfusion therapy either by fibrinolysis or primary angioplasty is applied to evaluate an infarct size, left ventricular function, epicardial vessel patency, tissue perfusion and to predict the clinical outcome5,36-38.
As it has been shown, the degree of epicardial and tissue reperfusion achieved after both a combined therapy alone as well as after the whole procedure was strongly associated with NT-proBNP level measured 48 hours after an angioplasty. In the only study presented so far it was shown that increased concentrations of BNP at initial presentation of patients with STEMI were associated with impaired coronary flow and an incomplete ST-resolution after fibrinolysis39.
Moreover myocardial injury measured by CK-MB release during the first 48 hours after an angioplasty was positively correlated with NT-proBNP. LV function expressed as ejection fraction was negatively correlated with NT-proBNP concentration. In Horio et al34 study plasma BNP levels on the first day or the 14th and 28th day were inversely correlated with LV ejection fraction obtained by left ventricle angiography at the acute or chronic phase, respectively. Additionally, the BNP concentrations on days 14 and 28 were positively correlated with the maximal myosin light chain I level as an indicator of an infarct size.
In conclusion, the reduction of ST-segment elevation, enzymatic injury and LVEF were correlated in a multiple regression analysis with NT-proBNP level. Above mentioned results show that NT-proBNP could be an early, valuable biochemical endpoint assessing the microvasculature well-being and myocardial injury and function after MI.
Prognostic value of NT-proBNP
Recently, it has been shown that the measurements of BNP and NT-proBNP are useful prognostic tools in the population of both NSTEMI as well as STEMI patients20-22,29,36. The measurement of NT-proBNP on admission improves the early risk stratification of patients across the whole spectrum of acute coronary syndromes (ACS), suggesting the need for the development of targeted therapeutic strategies20. Elevated NT-proBNP of patients with STEMI29 or BNP of patients with STEMI39 at initial presentation were associated with higher short-term risk of mortality. Moreover a single measurement of B-type natriuretic peptide, obtained in the first few days after the onset of ischaemic symptoms, provides powerful information for use in risk stratification across the spectrum of acute coronary syndromes, suggesting that cardiac neurohormonal activation may be a unifying feature among patients at high risk of death after ACS22. In our study increasing quartiles of NT-proBNP were related to mortality (p=0,0012) as well as to a composite endpoint (p=0,0012) in a long-term follow-up.
The multivariate analysis performed in the presented study displayed that the fourth quartile of NT-proBNP obtained 48 hours after an angioplasty was a significant independent predictor of the occurrence of a composite endpoint during a 1-year follow-up. One may conclude from the previous study that the NT-proBNP measured on admission or within 3 days after an admission in patients with the whole spectrum of ACS was independently associated with both 30-day mortality rate and the frequency of severe HF24 as well as with a long-term mortality21. Moreover, in this study Killip class 3/4 on admission, incomplete epicardial flow (TIMI<3) after a combined therapy and LVEF<45% measured 48 hours after PCI were associated with a higher rate of a composite endpoint.
Limitations
The present study is a prospective analysis of angiographic and clinical data in a large cohort of consecutive patients. Subjective angiographic assessment of TMPG represents a major limitation of the presented study. In order to make an objective myocardial perfusion evaluation, at least two experienced investigators reviewed each coronary angiogram in a blinded fashion. In the case of a lack of agreement between the two investigators, a third one was sought, and the conclusions were drawn. As patients with cardiogenic shock on presentation were excluded from this treatment protocol the enrolled population was a relatively low-risk one. So, the total, both in-hospital as well as 1-year mortality rate, was relatively low. That is why in a multivariate analysis the independent predictors of a composite endpoint defined as death and HF requiring hospitalisation were marked.
Conclusions
Our data show that NT-proBNP level measured after an STEMI was associated with a degree of microvascular reperfusion, myocardial injury and left ventricle function. Moreover, NT-proBNP is independently associated with a mortality rate or the frequency of HF requiring hospitalisation in a one-year follow-up. Our data indicate that the evaluation of NT-proBNP after STEMI could be used not only as a predictive biochemical indicator of long-term clinical outcomes but may be an early, valuable parameter describing reperfusive well-being of left ventricle microvasculature and cardiomyocytes.

