Abstract
Background and objectives: After a percutaneous coronary intervention (PCI) creatine kinase-MB fraction (CK-MB) elevation is observed in 5 to 30% of the cases. The often long and diffuse lesions of chronic total coronary occlusions (CTO) could represent a high risk group. However, there is no systematic data available on the incidence of elevation of cardiac troponin I (cTNI) after recanalisation of CTOs.
Methods: In 201 patients a CTO was successfully recanalised with stenting of all lesions and the regional wall motion (WMSI) was assessed at baseline and follow-up. For comparison we analysed 111 stable angina patients with stenting of single non-occlusive lesions. Over a period of 24 hours after PCI, CK-MB and cTNI were measured.
Results: CK-MB elevation after recanalisation of CTOs was observed in only 6% of patients with CTOs. The incidence of cardiac biomarker elevation was similar in patients with normal and severely impaired regional function, indicating that the low incidence was not due to a high prevalence of non-vital myocardium. In comparison CK-MB elevation after stenting of single non-occlusive lesions was observed in 13% of patients. In 14% of patients with CTOs and in 20% of patients with a single non-occlusive lesions cTNI increased after PCI.
Conclusions: Despite the high plaque load of organised thrombotic material in CTOs, the incidence of cardiac biomarker elevation after recanalisation of CTOs was similar to that after stenting of single non-occlusive lesions. A specific adjunctive medical or interventional therapy may not be warranted during recanalisation of CTOs.
Introduction
Creatine kinase-MB fraction (CK-MB) elevation as an indicator of distal microembolisation is observed in 5 to 30% after stent implantation for non-occlusive lesions1-4. While some studies reported a linear relationship between elevation of CK-MB levels and cardiac mortality3,5,6, others found a non-linear relationship, with an excess risk being limited to the patients showing CK-MB levels of more than five to eight times the ULN4,7. Platelet reactivity plays a key role in the pathogenesis of CK-MB elevation after percutaneous coronary interventions (PCI)8. Consequently adjunctive therapies such as platelet glycoprotein IIb/IIIa receptor inhibitors are applied, and distal protection devices are approved for specific types of lesions9-11.
In view of the often long and diffuse lesions of chronic total coronary occlusions (CTO) with their large plaque load of organised thrombotic material these lesions could represent a high risk lesion group which might require adjunctive therapies12. In the TOSCA study, periprocedural elevation of CK-MB occurred in 6.9% of patients after recanalisation of CTOs13. However, systematic data on the incidence of elevation of cardiac troponin I (cTNI) for these patients is not available. To determine how often periprocedural myocardial infarction during PCI occurred, we measured cardiac biomarker elevation in 201 patients after recanalisation of CTOs and in 111 patients after stent implantation of single non-occlusive lesions. We also evaluated whether the incidence of cardiac biomarker elevation could be related to the extent of regional myocardial dysfunction and the recovery of regional and global left ventricular (LV) function in patients with CTOs.
Methods
Study population
In 201 prospectively recruited patients (age 63±10 years; 159 men, 42 women) a CTO (duration > 2 weeks, median 5 months) was successfully recanalised with stent implantation in all lesions between January, 1999 and December, 2004. Inclusion criteria were (A) duration of the occlusion > 4 weeks, (B) TIMI 0 or I coronary flow, (C) evidence of ischaemia by a non-invasive test related to the occluded vessel or (D) viable myocardium in an akinetic segment assessed by stress echocardiography or nuclear imaging techniques. All diagnostic angiograms showed collateral flow grade 2 (partial epicardial filling of the occluded artery) or 3 (complete epicardial filling)14. All patients with successfully recanalised CTOs were scheduled for a repeat angiography after 4 to 6 months.
For comparison, 111 prospectively selected patients (age 62±9 years; 81 men, 30 women) who received a stent implantation for a single non-occlusive lesion were evaluated. Exclusion criteria for all patients were cardiac biomarker elevation at baseline.
The study had been approved by the institutional review board. All patients gave written informed consent for the coronary procedure.
Patients with CTOs
The recanalisation was performed via the femoral approach using 6F or 7F guiding catheters as described before15,16. The interventional strategy was to use stents in all patients to cover the lesion site with a balloon/artery ratio of at least 1.117. Angiographic success was defined as a final angiographic residual stenosis of <20% by visual estimation.
All patients took regularly 100 mg aspirin per day. During the intervention, a bolus of 100 IU/kg intravenous heparin was given. Immediately after the intervention all patients received clopidogrel 300 mg as loading dose, and subsequently 75 mg per day for 4 weeks. All other medications were given at the discretion of the attending physician. Platelet glycoprotein IIb/IIIa receptor inhibitors were not used in this study.
All patients were prospectively observed regarding periprocedural complications (Q-wave-myocardial infarction, death or need for urgent revascularisation) during hospitalisation.
Quantitative left ventriculography
Biplane left ventricular angiograms were obtained in patients with CTOs at the time of the baseline diagnostic angiography before PCI and repeated at follow-up. The LV function was analysed using a standard software program (Left Ventricular Analysis 4.0, Pie Medical Imaging, Maastricht, The Netherlands). The centreline method was used to assess regional LV function in the territory of the recanalised artery by the regional wall motion severity index (WMSI [SD/chord]) and the extent of wall motion abnormalities (number of chords)18.
Patients with CTOs were divided into 88 patients with either a normal or moderately impaired regional function (sub-group N: WMSI > – 2 SD/chord) and in 103 patients with a severely impaired regional function (sub-group A: WMSI < – 2 SD/chord). No left ventricular angiogram was available in 10 patients (2%) at the time of the baseline diagnostic angiography before PCI.
For the follow-up analysis, patients were subdivided according to the change of WMSI with an improvement of > 1 indicating a significant change. No follow-up angiography was available in 31 patients (15%).
Patients with single non-occlusive lesions
The group was chosen to represent a low risk group of patients with stable angina pectoris and lesions with low complexity. It consisted of 111 prospectively selected patients with significant coronary artery disease (reduction of the lumen diameter of > 70%) and evidence of ischaemia by a non-invasive test related to the stenotic vessel.
Exclusion criteria were (A) elevation of cardiac biomarker before PCI, (B) AMI during the last 4 weeks before PCI, (C) terminal renal insufficiency, hypothyroidism, or skeletal muscle injury, (D) chronic occlusion, bifurcation lesion, or in-stent restenosis, (E) multivessel intervention, (F) side-branch occlusion or prolonged vasospasm, (G) contraindication for antiplatelet medications, and (H) administration of glycoprotein IIb/IIIa receptor antagonists.
All interventions were performed via the femoral approach with standard technique. Procedural success was defined as a reduction of stenosis to <20% residual narrowing. Periprocedural medication was identical to patients with PCI for CTO.
Cardiac biomarker
Venous blood samples were taken before and over a period of 24 hours after PCI: the first immediately before the beginning of PCI (baseline), and the second and third at 8-12 and 18-24 h, respectively. Creatine kinase (CK), CK-MB and cTNI were analysed in these samples. The maximum value of the second or third measurement was used for further analysis. CK (ULN for women 2.78 µmol/L/sec, for men 3.17 µmol/L/sec) and CK-MB (ULN 0.2 µmol/L/sec) were enzymatically determined at 37° Celsius (synchronic LX-system, Beckman Coulter, USA). Troponin I (cTNI) was measured by a two-site immunoenzymatic (sandwich) immunoassay (Access AccuTnI Troponin I Assay, Beckman Coulter, USA). The 99th percentile of the cTNI level in a reference population was below the lower limit of detection of 0.04 ng/mL. The variation coefficient as measure of the precision within the lower concentration range was below 10%19. The cTNI threshold of 0.2 ng/mL was used to determinate periprocedural myocardial infarction. This cut-off value had a sensitivity of 97% and a specificity of 90%. The personnel, that carried out and analysed all biochemical measurements, did not have any knowledge of the procedural results.
Statistical analysis
Continuous numerical data are given as mean value ± standard deviation. Categorical data are represented as percent. In order to analyse differences between groups, we used the Whitney U test for steady numerical data and Fisher exact test for data in categories. A logistic regression analysis was done to assess determinants of cardiac biomarker elevation.
A two-sided p-value <0.05 was considered to indicate a significant difference. All calculations were done using the statistical software SPSS for Windows (Version 12.0.1, SPSS, USA).
Results
Clinical and angiographic data
Both groups were similar with regard to age, sex, cardiovascular risk factors, medical therapy, clinical symptoms and target vessel of the lesion at the time of PCI (Table 1, 2).
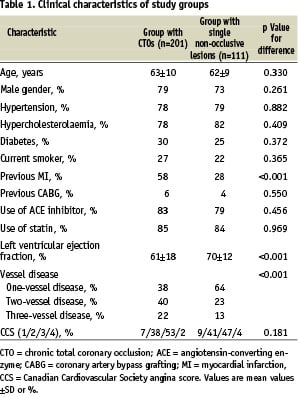
The prevalence of multivessel disease and previous myocardial infarction was significantly higher in patients with CTOs than in patients with single non-occlusive lesions. The left ventricular ejection fraction (LVEF) was significantly lower in patients with CTOs at the time of PCI (Table 1).
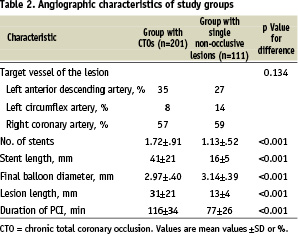
Number of stents used, the lesion and stent length were significantly higher in patients with CTOs than in patients with single non-occlusive lesions. The stent diameter was significantly lower and the duration of PCI was significantly longer (Table 2).
The duration of CTOs ranged from 1 to 153 months (median 5 months). 72% of all patients with CTOs had true occlusions (TIMI 0) and 28% had functional occlusions (TIMI 1). 35% of CTOs were located in the proximal or medial segments of the left anterior descending artery, 8% in the proximal segment of the left circumflex artery and 57% in segments proximal to the crux cordis of the right coronary artery (Table 2).
Clinical events
One patient with CTO had angiographic evidence of distal microembolisation and a no-reflow phenomenon. An angiographic evidence of intravascular thrombi which resolved with stenting appeared only in one patient with CTO. All but one patient with CTO had normal TIMI 3 flow at procedure completion. Angiographic evidence of distal microembolisation, no-reflow, coronary spasm or intravascular thrombi did not occur in patients with single non-occlusive lesions. In-hospital periprocedural complications did not happen in both groups within 24 hours after PCI.
Cardiac biomarker
The incidence of postprocedural elevation of cardiac biomarker was not significantly different in both groups. CK-MB and cTNI elevation after stent implantation for single non-occlusive lesions in patients with stable angina tended to be even higher than those found after recanalisation of CTOs. The incidence of CK-MB elevation was 6% after recanalisation of CTOs and 13% after stenting of single non-occlusive lesions (Figure 1).
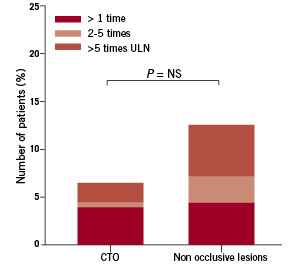
Figure 1. Incidence of postprocedural increase of creatine kinase-MB fraction >1, 2 to 5, and >5 times above upper normal limit (P=NS).
In 14% of patients with CTOs and in 20% of patients with a single non-occlusive lesions cTNI increased after PCI (Figure 2).
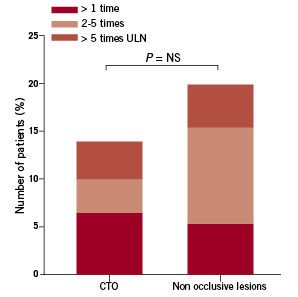
Figure 2. Incidence of postprocedural increase of troponin I >1, 2 to 5, and >5 times above upper normal limit (P=NS).
The cumulative incidences of peak levels of CK-MB and cTNI were similar in both groups (Figures 3,4).
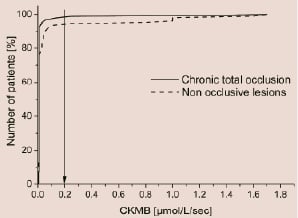
Figure 3. Cumulative amount of peak levels of creatine kinase-MB fraction in CTOs vs single non-occlusive lesions group.
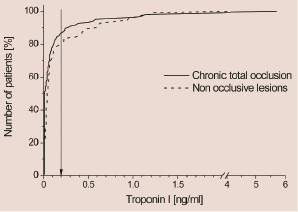
Figure 4. Cumulative amount of peak levels of troponin I in CTOs vs single non-occlusive lesions group.
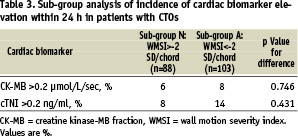
The sub-group analysis of CTOs did not reveal a significant difference for the incidence of CK-MB or cTNI elevation in patients with or without impaired regional LV function (Table 3).
38% of patients showed a significant improvement of regional LV function (WMSI increase > 1), whereas 62% showed no change with follow-up angiography. LVEF improved by about 6% during follow-up from 61±18 to 67±17% (P<0.001). In a logistic regression analysis to determine predictors of cardiac biomarker elevation, we included the improvement of regional and global LV function as parameters. Neither improvement of regional LV function (r2=0.036, P=0.641) nor the improvement of global LV function (r2=0.083, P=0.337) were significantly associated with cardiac biomarker elevation.
Discussion
In this study, we showed that the incidence of cardiac biomarker elevation after recanalisation of CTOs was similar to that after stent implantation in stable angina pectoris patients with single non-occlusive lesions. This was not due to the prevalence of nonvital myocardium in patients with CTOs.
Earlier studies found an elevation of CK-MB levels in 5 to 30%1-4, and an elevation of cTNI levels in 17 to 44% of patients after PCI of single non-occlusive lesions6,20-22. The TOSCA and MAJIC studies reported an elevation of CK-MB levels in 6.9 to 16% of patients after PCI of CTOs13,23. The values in our study were in the lower range of the reported incidence rates. CK-MB and cTNI elevation after stent implantation for single non-occlusive lesions in patients with stable angina representing a low risk group tended to be even more frequent than after recanalisation of CTOs. Despite the lack of complementary clinical evidence the criteria for a periprocedural myocardial infarction were fulfilled in accordance with the recent guidelines24.
Mechanism of cardiac biomarker elevation
The exact mechanism of cardiac biomarker elevation is not well-known. Mehran et al. found that postprocedural CK-MB elevation reflected the magnitude and the extent of atherosclerosis25. Other authors assumed that postprocedural CK-MB elevation was related mainly to ischaemia and prolonged balloon inflation or to vessel complications3,26. In approximately one third of cases, occlusions of small side branches during PCI were held responsible for postprocedural CK-MB elevation. Other causes were angiographic proof of clots, coronary dissection, coronary spasm and distal microembolisation2,27-29.
Two recent studies showed that the extent of myocardial necrosis measured by magnetic resonance imaging directly correlated to CK-MB and cTNI elevation30,31. In these studies the majority of patients showed new myocardial necrosis in a previously normal area distal from the inserted stent. Microembolisation was the most likely explanation for the myocardial necrosis. We recently demonstrated that high-intensity transient signals as indicators of embolic particles can be detected by intracoronary Doppler ultrasound occurring frequently during PCI, especially after stent implantation32.
We did not record side branch occlusions in our study. But other complications that explained cardiac biomarker elevation were rare in patients with CTO or did not occur in patients with single non-occlusive lesions. Therefore, we may assume that microembolisation during PCI most likely accounted for the cardiac biomarker elevation. Due to the low incidence of microembolisation, patients with CTOs might not benefit from platelet glycoprotein IIb/IIIa receptor inhibitors or distal protection during PCI.
Risk factors for cardiac biomarker elevation
Several factors could have contributed to the fact that we found such a low incidence of periprocedural cardiac biomarker elevation. First we had excluded venous bypass vessels or multiple coronary interventions at the same time, and we had not performed additional ablative procedures such as rotablation or atherectomy.
In previous studies it was observed that the plaque composition rather than the plaque size had an influence on the rate of periprocedural cardiac biomarker elevation. Especially patients with unstable lesions had greater plaque debris in filter baskets after PCI than patients with stable lesions33. The majority of the often long and diffuse lesions of CTOs were older than 4 weeks and consisted most likely of organised thrombotic material12. Thus, the danger of peripheral microembolisation was obviously small despite a longer procedure and more and longer stents per lesion in the CTOs of our study.
It would also be possible that no periprocedural cardiac biomarker elevation were observed because of a non viable myocardium. However, there was no difference between CTOs subtending an akinetic area and those with normo- or hypokinetic myocardium regarding the incidence of cardiac biomarker elevation. Furthermore, periprocedural cardiac biomarker elevation could depend on the presence of myocardium with preserved potential for functional recovery, that is, preserved viability. But neither the improvement of regional nor of global LV function were related or influenced by the cardiac biomarker elevation.
Finally, the ARMYDA study showed that treatment with atorvastatin before PCI in patients with stable angina significantly reduced periprocedural myocardial infarction and improved outcome34. Another study by Briguori et al confirmed the beneficial role of preprocedural statin administration on lowering the rate of periprocedural myocardial infarction35. Thus, the low rate of periprocedural myocardial infarction in this study may also be influenced by the high frequency of pretreatment with statins.
Limitations
The incidence of postprocedural CK-MB and cTNI elevation might have been even lower if patients in both groups received a loading dose of 300 mg clopidogrel prior to instead of on the day of PCI. The ARMYDA-2 study showed that a 600 mg loading dose of clopidogrel resulted in a 46 and 41% reduction of postprocedural CK-MB and cTNI elevation respectively compared with a 300 mg loading dose given 4 to 8 hours prior to PCI36. Otherwise, van den Heijden et al could not find any difference in the incidence of postprocedural elevation of either CK-MB or cTNI elevation relating to the initiation of clopidogrel treatment 3 days prior to or on the day of PCI37.
The primary focus of our study was analysing the incidence rate of peri-procedural myocardial infarction in patients with single non-occlusive lesions in comparison to high risk patients with CTOs. Therefore, we chose groups with similar comorbidities but different risk profile. However, minor differences in clinical characteristics should not result in a relevant study bias.
Conclusion
In summary, we have shown that the incidence of cardiac biomarker elevation after recanalisation of CTOs is similar to that after stent implantation for single non-occlusive lesions. Despite the high plaque load of organised thrombotic material in CTOs a specific adjunctive medical or interventional therapy appears to be not required during recanalisation of CTOs, unlike in acute coronary occlusions where a beneficial effect of these adjunctive therapies was shown38.

