Abstract
Aims: To evaluate the long-term follow-up of drug-eluting stents (DES) in the treatment of unprotected left main coronary artery (ULMCA).
Methods and results: One hundred and forty-eight patients (mean age 71±10 years) with ULMCA stenoses underwent percutaneous coronary intervention (PCI) with DES. Mean ejection fraction (EF) was 63±13% and distal ULMCA was involved in 63.5% of cases. In-hospital outcome showed one intra-procedural death, no stent thrombosis and 2% non Q-wave myocardial infarction (MI). Clinical follow-up was available in all patients (874±382 days): 10.1% of them had died, 8.8% had target lesion revascularisation (TLR) and 4.1% experienced MI. Major adverse cardiac events (MACE) occurred in 20.3%. Mortality predictors were EF≤55% (OR 3.6, 95%-C.I. 1.3-10.1, p=0.016) and EuroSCORE>6 (OR 3.9, 95%-CI 1.1-14.1, p=0.037). TLR predictors were distal lesion (OR 8.5, 95%-CI 1.1-15, p=0.041) and age<64 years (OR 3.1, 95%-CI 1-9, p=0.042). MACE predictor was EF<55% (OR 2.4, 95%-CI 1.1-5.2, p=0.027).
Conclusions: ULMCA stenting with DES is safe, with favourable in-hospital outcome. Long-term results are acceptable with a mortality rate of 10%, a TLR rate of 9%, and a MACE rate of 20%. Low EF and high EuroSCORE predict mortality, while younger age and distal lesions predict TLR. Low EF also predicts MACE.
Introduction
Significant unprotected left main coronary artery (ULMCA) disease occurs in 5-7% of patients undergoing coronary angiography1,2 and patients with ULMCA disease treated medically have a three-year mortality rate of 50%3,4. Coronary artery bypass graft (CABG) is the cornerstone of treatment for these patients5,6. Clinical trials in patients with significant narrowing of the left main demonstrated that CABG substantially reduces the three-year mortality seen with medical therapy7. Several studies have demonstrated the safety and feasibility of ULMCA intervention using bare metal stents8-15 but in-stent restenosis (ISR) limits the long-term efficacy and may be associated with increased long-term mortality12. The advent of drug eluting stents (DES) pushed the rate of restenosis below 5% for most lesion types16,17. Interesting results have been reported with DES implantation in ULMCA, with a 1-year mortality rate between 0% and 4%18-21. What remains unclear is whether such favourable outcomes will be maintained at a long-term follow-up. The aim of this study was to evaluate the safety of ULMCA percutaneous coronary intervention (PCI) with DES and its long-term clinical outcomes. The main events analysed were death, myocardial infarction (MI) and target lesion revascularisation (TLR).
Methods
The present study included all the patients with de novo ULMCA stenoses, electively treated between September 2002 and September 2006 with PCI and sirolimus-eluting (Cypher, Cordis, Johnson & Johnson, Warren, NJ, USA), paclitaxel-eluting (Taxus, Boston Scientific, Natick, MA, USA) or zotarolimus-eluting stents (Endeavor, Medtronic, Minneapolis, MN,USA) in one single centre (Clinique Pasteur, Toulouse, France). All patients had symptomatic coronary disease or documented ischaemia and angiographic evidence of ≥ 50% stenosis of the ULMCA.
Patient selection
Patients were jointly evaluated by cardiac surgeons and interventional cardiologists and the decision to perform PCI instead of surgery was considered on the basis of a suitable anatomy for stenting, the technical feasibility of the procedure, the presence of comorbidities, a high surgical risk and the patient’s preference.
PCI technique
PCI was performed using mostly the transradial approach. An intra-procedural bolus of unfractionated heparin (70 IU/kg) was administered. Glycoprotein IIb/IIIa inhibitors were used at the discretion of the operator. Lesions involving the ostium or body of the ULMCA were treated with a single stent, while distal ULMCA stenoses were treated either with single or double stent technique. The choice of the single or double stent technique was made on the basis of the anatomy of the lesion, in particular the diameter of the side branch, the angulation of the bifurcation, the presence of disease on the ostium of the side branch, the length of the lesion on the side branch, the presence of a calcific lesion and the result after the deployment of the first stent. Culotte technique was preferred if the two vessels had similar diameter, V stenting if the angulation was favourable (<60°), T stenting for different vessel diameters with an angulation >60° and crush technique in all other cases. High-pressure stent deployment followed by post-dilatation with non-compliant balloons was systematically performed. Minimal lumen diameter, reference vessel diameter and percent diameter stenosis were measured. Antiplatelet therapy was started at least 24 hours before the procedure with aspirin (100 mg/day) and a loading dose of 300-600 mg of clopidogrel. After the procedure, all patients were prescribed lifelong aspirin (75-100 mg/day) and prolonged (at least 12 months) dual antiplatelet therapy of aspirin+clopidogrel or aspirin+ticlopidine was recommended.
Follow-up
Clinical follow-up of at least one year was performed for all patients by office visit or direct telephone call. A stress test was systematically performed at four months. An angiographic follow-up was suggested between six and nine months after the procedure.
Definitions
Procedural success was defined as successful percutaneous ULMCA angioplasty with residual stenosis <30% by quantitative coronary analysis (QCA) after stent deployment and without death, MI, or emergency CABG before discharge. Deaths were classified as either cardiac or non-cardiac. Sudden deaths or death of unknown cause were adjudicated as cardiac. Non Q-wave MI was defined as elevation of serum creatine kinase MB (CPK-MB) that was three times the upper limit, without pathological Q waves. CPK-MB levels were systematically checked three, six and 12 hours after the procedure. TLR was defined as any revascularisation (PCI or CABG) performed to treat a >50% luminal narrowing at the stent site or in the 5-mm distal or proximal segments adjacent to the stent. Cerebrovascular events were defined as stroke, transient ischaemic attacks, and reversible ischaemic neurological deficits adjudicated by a neurologist and confirmed by CT scanning. Renal failure was defined as a creatinine clearance < 60 mL/min (Cockroft-Gault formula). Major adverse cardiac events (MACE) were defined as a composite of death, MI, and TLR.
The additive EuroSCORE was used to assess the cardiac surgical mortality risk at 30 days22,23. EuroSCORE>6 defined high risk patients.
Statistical analysis
Data are presented as frequencies with percentages and mean±SD. Differences between groups were assessed using chi-square for categorical variables and Student t-test for continuous ones. Event-free survival curves were generated by the Kaplan-Meier method, and the differences were assessed by the log-rank test. A multivariable Cox proportional hazard model was created to identify independent predictors of mortality, TLR and MACE. All the variables that showed, at the univariate analysis, a significant difference between groups, with a p-value <0.1, were entered in the Cox regression model, to evaluate their independent role in predicting events during the follow-up. Results were reported as odds ratios (OR), together with associated 95% confidence intervals (CI). Statistical analyses were performed using SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics
One hundred and forty-eight patients underwent PCI of the ULMCA with DES. In the same period, at our institution, 257 patients with ULMCA underwent surgical treatment. The mean age was 71±10 years, 120 patients (81.1%) were males and 40 (27%) were diabetic. Sixty-two patients (41.9%) had renal failure. Twenty-four patients (16.2%) had a previous MI and 42 (28.4%) a previous PCI. Mean ejection fraction (EF) was 63±13% and 36 patients (24.3%) had an EF <55%. A distal lesion was present in 94 patients (63.5%) and single or multiple associated non-ULMCA stenoses in 113 (76.4%). High-risk patients were 69 (46.6%). Fifty-one patients (34.5%) presented as acute coronary syndrome (ACS). Clinical and angiographic baseline characteristics are summarised in Table 1.
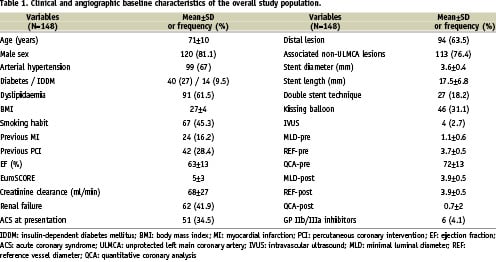
Procedural characteristics and in-hospital follow-up
Radial approach was used in 109 patients (73.6%). Eighty-five patients (57.4%) were treated with sirolimus-eluting stents, 58 (39.2%) with paclitaxel-eluting stents and five (3.4%) with zotarolimus-eluting stents. Distal lesions were mostly treated with one-stent technique (67/94, 71.3%). Intraprocedural glycoprotein IIb/IIIa inhibitors were used in 6 patients (4.1%). Prophylactic intra-aortic balloon pump (IABP) support was never used. Procedural success was achieved in 147 patients (99.3%). Intra-procedural complications presented in two patients (1.4%): one coronary perforation and one cardiogenic shock needing rescue IABP, leading to the only intraprocedural death. During hospitalisation there were no additional deaths, no patient experienced stent thrombosis and three patients (2%) had non-Q wave MI.
Follow-up
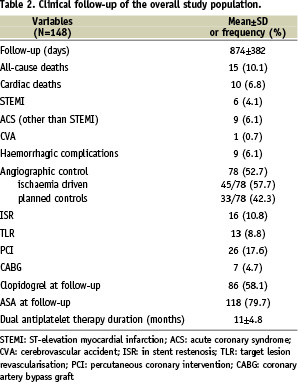
Clinical follow-up was available for 100% of patients over a mean of 874±382 days. At follow-up, 15 patients (10.1%) had died, 10 (6.8%) of them for cardiovascular causes. Of the 78 coronary angiograms performed during follow-up, 45 (57.7%) were ischaemia driven (13 of them by silent ischaemia and 32 by anginal symptoms) and 33 (42.3%) were planned angiographic controls. Younger patients (<64 years) had 20/37 (54.1%) angiograms and 12 of them were ischaemia driven; older patients (>64 years) had 58/111 (52.2%) angiograms (33 of them ischaemia driven). Sixteen patients (10.8%) had restenosis. Three patients, presenting with isolated ostial LCx intermediate stenosis, were oriented to medical treatment. Thirteen patients (8.8%) had TLR: 6 repeated PCIs and 7 CABGs. Among the 6 patients that had repeated PCI, one presented with ACS, 3 with silent ischaemia, and 2 were angiographic controls. Among the 7 patients that had CABG, 4 presented with ACS, 2 had silent ischaemia, and one was an angiographic control. Six patients (4.1%) experienced out-of-hospital MI. MACE occurred in 30 patients (20.3%). Among the 46 asymptomatic patients that had an angiogram, 6/46 (13%) had restenosis and 4/46 (8.7%) had TLR. Among the 33 planned angiographic controls, 2/33 (6.1%) had restenosis and TLR. Clopidogrel therapy was stopped after a mean period of 11±4.9 months and haemorrhagic complications occurred in 9 cases (6.1%). Clinical follow-up of the overall study population is summarised in Table 2.
Mortality
Mortality was significantly associated with an EF <55% (53.3% vs 21.1%, p=0.006), renal failure (66.7% vs 39.1%, p=0.04) and a higher EuroSCORE (7±3 vs 4.8±3, p<0.05). Independent predictors of mortality were EF <55% (OR 3.6, 95%-CI 1.3 - 10.1, p=0.016) and EuroSCORE >6 (OR 3.9 95%-CI 1.1-14.1, p=0.037). Figure 1 and Figure 2 show the cumulative survival in relation to EuroSCORE and EF.
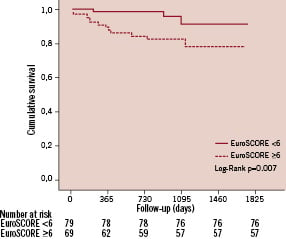
Figure 1. Kaplan-Meier survival curve according to EuroSCORE.
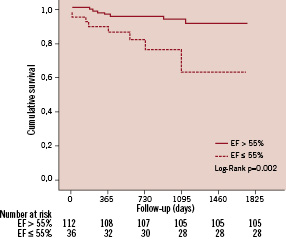
Figure 2. Kaplan-Meier survival curve according to EF.
ISR and TLR
Among the 16 restenosis, the angiographic pattern was diffuse in two cases and focal in 14 (87.5%). Nine ISR involved only the ostium of the side branch (LCx). Ostial LAD alone was involved in one case. ULMCA was involved in six cases: three in the bifurcation and three in the mid-shaft. Patients who had TLR, compared to TLR-free patients, were younger (64.8±12.6 vs. 71.6±9.6 years, p<0.05), had a higher prevalence of distal stenoses (92.3% vs. 60.7%, p=0.024), and had longer stents (22±8 vs. 17±7 mm, p<0.05). After subdivision in quartiles of age, we found a higher TLR rate in patients belonging to the 1st quartile (age < 64 years), compared to the other quartiles: 16.2% vs. 6.3% respectively, p=0.065. Independent predictors of TLR were age < 64 years (OR 3.1, 95%-CI 1-9.3, p=0.042) and the presence of a distal ULMCA stenosis (OR 8.5, 95% CI 1.1-15, p=0.041). The length of the stent was included in the multivariate model as a categorical variable with a cut-off value of 18 mm (median value) but it had no predictive role on TLR. Figure 3 shows the TLR-free survival in relation to the site of the stenosis.
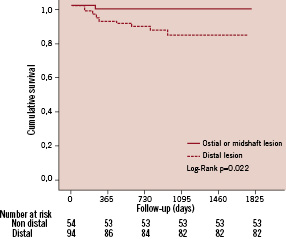
Figure 3. Kaplan-Meier TLR-free survival curve according to the lesion site.
MACE
Six patients (4.1%) had MI at follow-up. MACE rate was 20.3%. Table 3 shows MACE rate at different time interval, during follow-up. Patients who experienced a MACE had a low EF (58±14 vs. 64±13, p=0.037) and a trend towards a higher prevalence of distal lesion (76.7% vs. 60.2%, p=0.09). At multivariate analysis, EF < 55% was the only independent predictor of MACE (OR 2.4, 95%-CI 1.1-5.2, p=0.027).
Table 4 summarises the results of the multivariate Cox analysis, showing predictors of mortality, TLR and MACE. Figure 4 shows the cumulative survival for all-cause mortality.
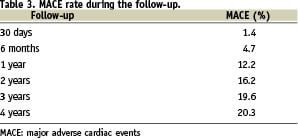
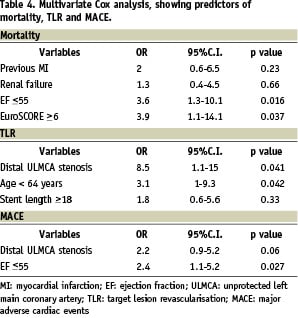
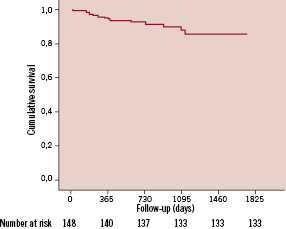
Figure 4. Kaplan-Meier survival curve for all-cause mortality.
Discussion
Procedural and in-hospital outcomes
Similar to other series18,20,21, our study showed that the treatment of ULMCA with DES appears safe, with high procedural success and low procedure-related complication rate. Our experience shows favourable in-hospital outcomes, particularly a low rate of non Q-wave MI and no stent thrombosis. These observations are relevant in a population where 47% of patients were at high risk, according to EuroSCORE. Reported in-hospital complication rates vary among previous series, depending on the heterogeneity of risk profile, and range from 1 in low-risk patients to 13% in patients who had contraindications for surgery or were in critical conditions8,24.
Long-term follow-up
1. MORTALITY
Mortality at one year was 4.7% and it is consistent with other reports showing a 1-year mortality of 0% to 5%20,25,26.
Long-term follow-up, at an average of 874 days, shows that the initially favourable results are followed by acceptable outcomes, with a mortality of 10%. These are quite interesting data, since few results are available for an average follow-up longer than two years24. Although a mortality rate of 10% is not negligible, it is in step with what observed in larger series of ULMCA patients treated surgically, even with bilateral mammary artery grafting27-31. Classical risk markers such as low EF, renal impairment and a high EuroSCORE were associated with a poor survival rate: patients with all these three characteristics had a mortality of 37.5% (6/16), while those having a normal EF, normal renal function and a low EuroSCORE showed a mortality of 5.6% (3/54). Low EF and EuroSCORE were also independent predictors of death. These results are coherent with another study where the observed in-hospital and one-year mortality was tightly linked to the presence of critical conditions, being 78% in patients with poor left ventricular function and ACS, and 3.4% in patients without such characteristics10. Interestingly, the mortality rate seen at 2.4 years is more than twice that the one observed at one year (10 vs. 4.7%). This finding supports the need for longer follow-ups in ULMCA patients treated with DES. ACS, differently from other series10, did not show any association with mortality, probably due to the absence of very critical patients (cardiogenic shock or ST segment-elevation MI). These observations stress the importance of patients’ selection and confirm that high-risk patients with an expected unfavourable surgical outcome have also a poor outcome after PCI. In our series, each patient with an anatomy suitable for PCI had been collegially evaluated for both treatment options. On account of our previous experience10, patients with a low EF were preferably addressed to surgery. CABG was also preferred for complicated distal ULMCA lesions, particularly in younger patients.
2. ISR AND TLR
In our study, all the patients had a functional evaluation with a stress test at four months and an angiographic control at 6-8 months was only suggested. Most of the coronary angiograms performed at follow-up were therefore ischaemia driven. Fifty-two percent of our patients underwent coronary angiogram during follow-up, with an overall ISR rate of 10.8%. Differently, in a series where serial angiographic follow-up was performed, ISR was more frequent, affecting 42% of patients32: in the same study 94% of treated lesions involved the distal ULMCA, which is known to be more frequently associated to ISR, especially when treated with the two-stent technique18,20,21. In our population distal bifurcation lesions were 63%. As usually seen in DES, the main pattern of ISR found in our patients was focal16,18,20. It involved mostly the side-branch (LCx) ostium, as in most series where it accounts for about one-half of the restenosis cases18,20,21, often with a lesion of intermediate degree, sometimes allowing medical therapy alone.
TLR rate at follow-up resulted to be 8.8%, which is consistent with previous observations where TLR varied from 0% to 14%20,21,25,26. Distal ULMCA stenosis was found to be an independent predictor of TLR. This is a relevant finding for two reasons: (1) the majority of left main lesions are located in the distal bifurcation and (2) we still do not know the ideal stenting approach for distal ULMCA33.
In our series, we did not find any difference in outcome, namely TLR rate, between single- and double-stent techniques. Our usual approach was provisional stenting, explaining the low rate of double stenting (18.2%). Strikingly, as in other series evaluating DES restenosis34, younger patients showed a higher TLR frequency, and an age less than 64 years was an independent predictor of TLR. Whether a higher prevalence of TLR in younger patients is related to biological or social factors, such as a stricter medical assistance or a higher attention to angina-like symptoms, remains nevertheless unclear. On a biological basis, one possible explanation of may be attributed to a more active endothelial proliferation at the PCI site in the younger patient population as compared with the older patients.
3. MACE
MI at follow-up occurred in 4% of the patients. The observed MACE rate of 20% is similar to that observed in two recent series35,36 and its only independent predictor was EF <55%. A low EF identifies those patients with a higher risk profile, explaining its role in predicting a worse outcome.
The availability of all these observational data at a mean follow up of 2.4 years should help us in understanding the present role of ULMCA treatment with PCI and DES. Although surgical treatment is considered the gold standard for ULMCA revascularisation, it carries a not negligible in-hospital mortality rate (from 1.7% to 7%) and a 1-year mortality rate of 6% to 14% as reported in some retrospective studies27-30. Our study and several series about DES use in ULMCA showed comparable results in terms of mortality at one year18,21,35,36. What seems far from equalling the results observed with surgery is the rate of TLR: this has dramatically lowered with the advent of DES, but remains still higher if compared to surgical series. Nonetheless, ISRs can often be treated by re-PCI and ULMCA stenting neither precludes nor augments the risk of an eventual CABG during follow-up.
The longer follow-ups available for CABG studies strengthen the position of surgery over PCI, and our finding of a two-fold mortality rate at 2.4 years in comparison to that seen at one year underlines the need for longer follow-ups in PCI patients. At present it seems however reasonable to consider the two treatment strategies as complementary options. It is still impossible to define exactly which would be the best choice to propose to every single patient, but some characteristics that could help us in patients’ selection are being outlined. Ideal cases for stenting are low-risk patients with good LV function, non distal and non calcified left main stenosis: PCI could be considered in case of small LCx, elderly patients, high surgical risk (EuroSCORE), distal coronary disease unfavourable to CABG, relevant comorbidities (namely chronic obstructive lung disease) or emergency clinical situation as acute ULMCA occlusion. Surgery is preferable in the presence of heavy calcified ULMCA disease or reduced LV function. Good candidates for surgery are patients with distal bifurcation lesion and reduced LV function, with distal bifurcation lesion and occluded right coronary artery or with multivessel disease suitable for CABG or with additional complex coronary artery lesions.
Conclusions
PCI of ULMCA with DES implantation appeared relatively safe. Long-term clinical follow-up showed a mortality rate of 10%, a MACE rate of 20% and a TLR rate of 9%.
Low EF defines the group with the highest MACE rate. Mortality is tightly linked to low EF and EuroSCORE, while TLR is predicted by younger age and distal ULMCA lesion.
Study limitations
This is a retrospective study and the small number of selected patients may have influenced the results. Nevertheless, there are not many studies with an average follow-up longer than two years and the small number of patients can be partly explained by the low occurrence of this lesion in the general population.

