Abstract
Aims: The purpose of this study was to examine the long-term results of the sleeve technique, which is a modification of the crush technique and capable of increasing the success of final kissing balloon inflation (FKB) in the treatment of non-left-main coronary bifurcation lesions.
Methods and results: Forty-five patients with 45 non-left-main coronary bifurcation stenoses were treated with drug-eluting stents (DES) using the sleeve technique and prospectively evaluated. Follow-up angiography was performed on 41 patients (91%) at nine months.
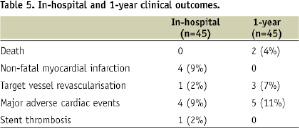
The mean age of patient was 65 years with predominance of male (73%); FKB was successfully performed in all patients. Post-procedure myocardial infarction was observed in four patients, leading to an in-hospital major adverse cardiac event (MACE) rate of 9%. At angiographic follow-up, the late loss in the main vessel and side-branch was 0.18±0.26 mm and 0.29±0.27 mm, respectively. Binary angiographic restenosis was seen in two patients (4.7%) at main vessel and one patient (2.4%) at side-branch. At 1-year follow-up, there were two non-cardiac deaths and three patients needed revascularisation.
Conclusions: The use of the sleeve technique and DES in the treatment of non-left-main coronary bifurcation lesions is associated with a low angiographic restenosis, particularly at side branch ostium, and long-term safety.
Introduction
The introduction of drug-eluting stents (DES) has revolutionised the treatment of coronary bifurcation lesions compared with bare-metal stents1. Coronary bifurcation lesions remain a high-risk subset because of its association with worse clinical outcomes compared with non-bifurcation lesions, even in the present DES era2. Currently, 1-stent technique with provisional side-branch (SB) stenting is still the gold standard treatment strategy3. Two-stent technique (T-stenting) has not been shown to be superior to the former approach in randomised trials4 because of incomplete SB ostium coverage4,5. The crush technique is one of those techniques devised to overcome this pitfall6. It possesses hypothetical advantages of preserving the natural shape of bifurcation (unlike V-stenting) and minimum stent overlapping in the main vessel (MV) (unlike culotte technique). However, its efficacy is hampered by limited success of the final kissing balloon inflation (FKB), which is an important factor for attaining good long-term results7,8. The sleeve technique is a modified version of crush technique9, and has been shown to achieve 100% FKB over a wide range of lesions10,11. This study sought to report the 9-month angiographic follow-up and 1-year clinical outcomes of treatment of non-left-main coronary bifurcation lesions with DES using sleeve technique.
Materials and methods
Patients
From August 2005 to March 2007, consecutive symptomatic patients with MEDINA classification 1,1,0 and 1,1,1 coronary bifurcation lesions12 which had a diameter stenosis ≥50% were treated with 2-stent strategy using DES and sleeve technique9. All those MEDINA classification 1,1,0 bifurcation lesions had significant proximal SB disease (not ostial disease) which necessitated SB stenting. The vessel size must be ≥2.25 mm in MV and ≥2.0 mm in SB by visual estimation in coronary angiography. Patients who had left main coronary artery bifurcation stenoses, in-stent restenotic lesions10, left ventricular ejection fraction < 30%, heavily calcified lesions, contraindications to prolonged use of anti-platelet agents, and life expectancy < 2 years were excluded. Informed, written consent has been obtained from all patients.
Preparation and intervention procedure
All patients were pre-treated with aspirin ≥80 mg daily for ≥1 week; clopidogrel 300 mg oral loading dose, followed by 75 mg daily was prescribed at least 24 hours prior to intervention procedure. During intervention, an intra-arterial bolus of unfractionated heparin was administered at a dosage of 70 U/kg, additional bolus of heparin might be required to titrate the activated clotting time >250 seconds. Intravenous glycoprotein IIb / IIIa inhibitors were strongly encouraged and given at the discretion of operator and 7 Fr guide catheters were used in all procedures. The detail of the sleeve technique has been described elsewhere9,10. In brief, the bifurcation was double-wired; lesion preparation was performed by balloon pre-dilatation either in the MV, SB or both. A stent was positioned in SB with its proximal 2-4 mm segment protruding into the MV; a balloon of a length long enough to cover the protruding stent segment was concurrently positioned in the MV. The SB stent was deployed (Figure 1A), followed by removal of the SB stent-balloon and wire. The MV balloon was then inflated to crush the protruding SB stent segment against the MV wall (Figure 1B). The SB ostium was rewired through its own stent strut and dilated with a balloon (Figure 1C); the bifurcation was then kissed with two balloons (Figure 1D). Afterwards, a stent was deployed in the MV (Figure 1E). The SB ostium was rewired the second time through the MV stent strut and dilated with a balloon (Figure 1F), followed by FKB (Figure 1G). Cine-angiograms were taken in at least two orthogonal views following intracoronary administration of 200 µg of nitroglycerine before and after intervention. Patients were subsequently monitored overnight in coronary care unit; cardiac enzymes (creatinine kinase, CK-MB) were checked every eight hours for two consecutive days.
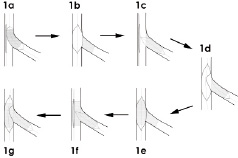
Figure 1. Schematic diagram showing the outline of the sleeve technique in the treatment of coronary bifurcation lesions.
Follow-up visits and clinical definitions
Patients were regularly assessed in out-patient clinic at four weeks, 12 weeks, six months and 12 months. Follow-up angiography was arranged at 8-12 months. All patients received life-long treatment of aspirin. Clopidogrel was dispensed for a mandatory period of 12 months; thereafter, patients were encouraged to purchase their own drugs for another 12 months. Post-procedure myocardial infarction was defined as troponin-I or CK-MB ≥3 times the upper limit of normal13. Stent thrombosis was defined and classified according to the recommendation proposed by the Academic Research Consortium14. Target vessel revascularisation (TVR) was defined as clinically driven percutaneous revascularisation or bypass of the target lesion or any segment of the epicardial coronary artery containing the target lesion. Major adverse cardiac event (MACE) was defined as any death, myocardial infarction or TVR. Angiographic success was defined as a final residual stenosis of <20% with Thrombolysis In Myocardial Infarction flow grade 3. Procedure success was referred to the achievement of angiographic success without in-hospital MACE.
Quantitative coronary angiographic analysis
Quantitative coronary angiographic analysis was performed offline using a validated automated edge detection system (CAAS II QCA V1.0, Pie Medical Imaging, Maastricht, The Netherlands) with contrast-filled catheters as calibration standard by an experienced investigator blinded to the clinical results. The reference diameter, minimal lumen diameter (MLD), and % diameter stenosis were measured at baseline, post-procedure and restudy. Acute gain was calculated from the difference of MLD between the post-procedure and baseline; whereas late loss was the reductions of MLD at restudy compared with post-procedure. Angiographic restenosis was defined as stenosis of ≥50% of the luminal diameter in the target lesion.
Results
There were 45 patients with 45 coronary bifurcation lesions included for analysis. The mean age was 65±12 years with predominance of male (73%). The demography and clinical characteristics were listed in Table 1.
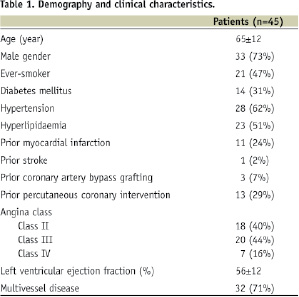
Diabetes mellitus was found in 14 patients (31%); 60% of patients had class III-IV angina on presentation. The lesion and procedure characteristics were summarised in Table 2.
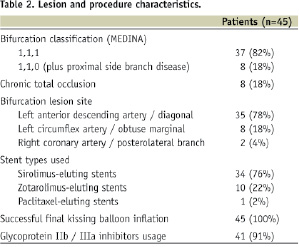
The majority of the stenoses were located at left anterior descending artery / diagonal branch bifurcations (78%). Sirolimus-eluting stents were the most commonly used stent (76%). FKB was successfully performed in all patients.
The stent implantation data were shown in Table 3. Follow-up angiography was performed on 41 (91%) patients at a mean of 9.0±1.3 months. The results of quantitative coronary angiography analysis were shown in Table 4.
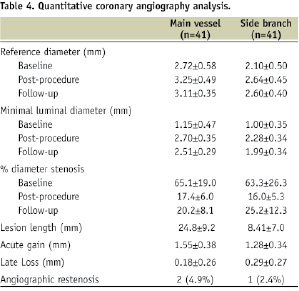
Late loss in the MV and SB was 0.18±0.26 mm and 0.29±0.27 mm, respectively. Angiographic restenosis in the MV and SB were 4.9% and 2.4%, respectively.
There were four patients (9%) who developed post-procedure myocardial infarction post-procedure, including one case of subacute stent thrombosis at day 3. Of the stent thrombosis case, angiography showed that the occlusion site was 10 mm distal to the bifurcation point. Intravascular ultrasound study revealed that stent thrombosis was caused by incomplete stent expansion at the stent outlet where there was a patch of calcium deposition. The resultant in-hospital MACE was 9%. At 1-year follow-up, two deaths were observed: one died of stroke at three months and the other suffered from chest infection at six months (non-cardiac death). There was no myocardial infarction or suspicious case of stent thrombosis. Three patients (7%) had TVR which was angiographically driven (Table 5).
Discussion
This is an angiographic follow-up study of the crush technique with 100% FKB, achieved through technical modifications (the sleeve technique). The overall (MV+SB) angiographic restenosis is 7.3%, with a very low SB restenosis (2.4%). These figures compare very favourably with historical controls using other stenting techniques4,7,8,16-19.
Post-procedure myocardial infarction is caused either by stent thrombosis, side-branch loss, or plaque embolisation and clogging of microcirculation. Apart from one case of definite stent thrombosis, the latest mechanism is the likely cause in this study owing to repeated balloon dilatations of the bifurcation lesions. Moreover, the use of a lower clopidogrel loading dose of 300 mg, instead of 600 mg, may also contribute to the higher ischaemic event15.
Classical crush technique has the major limitation that FKB is potentially difficult because wire and balloon have to cross double layers of stents; this problem may be aggravated when the bifurcation angle increases. The importance of FKB is easily appreciated from the results of the crush technique series7,8,19. SB restenosis rate ranges from 19-25% which corresponds to a FKB rate between 51-64%7,8,19. If only those with successful FKB were selectively analysed, the figure becomes 9-11%. The sleeve technique is a technical modification of the crush technique specifically devised to increase the success rate of FKB9. It splits the FKB step into two so that the wire and balloon have to cross only one layer of stent each time, but FKB has to be performed twice (Figure 1). Preliminary studies revealed that 100% FKB can be achieved in different lesion types and sites, with reasonable fluoroscopy time and a good safety profile10,11. One attractive theoretical advantage of the sleeve technique is that the multiple, stepwise dilatations of SB ostium is likely to allow even better stent expansion and apposition than classical crush technique. The entire procedure involves separate SB ostium dilatation twice (Figure 1C, 1F) and FKB twice (Figure 1D, 1G) (a total of four balloon dilatations). This may translate into extra long-term clinical benefits. In our study, the extremely low SB restenosis rate (2.4%) is very impressive. This concept has been supported by Chen et al, who found that SB restenosis is significantly lower in DK Crush (identical to the sleeve technique) than classical crush20. A larger scale, randomised intravascular ultrasound study is required to prove this hypothesis.
After the crush or sleeve technique, a small arc within a short segment of proximal MV wall above the bifurcation point contains three layers of stents; this raises the doubt of predisposition to late thrombotic complications. All our patients had mandatory dual antiplatelet therapy for at least one year. The 1-year result did not show any myocardial infarction or acute coronary event. The long-term safety of this technique has been echoed by Chen et al20. The duration of clopidogrel use has been shown to be closely related to the occurrence of death and myocardial infarction at follow-up21. A prolonged course of dual antiplatelet therapy is thus advisable for this complex lesions subset. The optimal duration remains to be determined.
This is a single-centre, single-arm, non-randomised registry which was subjected to selection and operator bias. The relatively small number of patients and the fact that about one-fifth of patients had non-ostial SB disease are major limitations of this study. Moreover, the assessment of late loss is not accurate enough without intravascular ultrasound measurement.
Conclusions
The clinical use of the sleeve technique and DES to treat non-left-main coronary bifurcation lesions is associated with a very low angiographic restenosis, particularly at SB ostium, as well as long-term safety.
Online data supplement
Video 1. Pre-intervention angiogram
Video 2. Positioning of side branch stent; main vessel balloon in
position
Video 3. Deployment of side branch stent
Video 4. Inflation of main vessel balloon to crush the protruding
segment of side branch stent
Video 5. Side branch is rewired and ballooned; main vessel balloon
in position
Video 6. First kissing balloon inflation
Video 7. Deployment of main vessel stent
Video 8. Side branch is rewired the second time and ballooned;
main vessel balloon in position
Video 9. Final kissing balloon inflation
Video 10. Final result

