Abstract
Aims: This study was performed to assess the incidence, patient characteristics and predictors of aborted myocardial infarction (MI) in patients with ST-segment elevation MI (STEMI) undergoing primary percutaneous coronary intervention (PPCI).
Methods and results: We enrolled 179 consecutive patients with STEMI within a fixed protocol for PPCI (Leiden MISSION! project); 90 patients received abciximab bolus in the hospital (in-hospital group) and 89 patients received abciximab bolus in the ambulance (pre-hospital group). Thirty-two patients (18%) fulfilled the criteria for an aborted MI. The incidence of aborted MI was four times higher in the pre-hospital abciximab group compared to the in-hospital group (OR=4.2, 95%CI=1.7-10.3). The median time between symptoms onset and abciximab bolus administration was significantly shorter in the aborted MI compared to established MI patients (70 vs 115 min, p=0.005). Multivariable analysis identified pre-hospital abciximab administration as the main predictor of aborted MI (OR=2.86, 95%CI=1.1–7.5).
Conclusions: In patients with STEMI treated with PPCI, the incidence of aborted MI was 18%. Pre-hospital abciximab administration was the main predictor of aborted MI, and this effect was related to the initiation of treatment within the first two hours after symptoms onset and to the higher infarct related artery patency at presentation.
Introduction
Myocardial necrosis can be recognised by the appearance in the blood of several proteins released by the damaged myocytes.1 The ultimate objective of reperfusion therapy for ST-segment elevation myocardial infarction (STEMI), is early and effective treatment that limits or even prevents clinically detectable myocardial necrosis2, resulting in aborted myocardial infarction (MI), a term first used by Weaver et al when reporting the pre-hospital MITI trial.3 Over 10% of patients treated with reperfusion therapy did not develop a rise of cardiac markers in plasma, but did exhibit transient ECG changes consistent with aborted MI.2,4 Coronary reperfusion with primary percutaneous coronary intervention (PPCI) has been established as the treatment of choice in the majority of cases with STEMI.5 The PPCI associated rate of aborted MI is still unknown; even a standardised definition of aborted MI after PPCI is lacking.
The purpose of the present study was to assess the incidence, patient’s characteristics and predictors of aborted MI in patients with STEMI undergoing PPCI.
Methods
Study design
This is an observational prospective study. All patients were treated according to the institutional STEMI protocol (MISSION!) implemented at Leiden University Medical Center (LUMC),6 which included standardised pre-hospital, in-hospital and outpatient clinical framework for decision making and treatment. Our hospital provides around-the-clock service of PPCI with six trained PCI physicians and dedicated nurses.
Patients selection
Main results of MISSION! Study are published elsewhere.6 For this study, patients were eligible if STEMI symptoms started <9 hours before the procedure, the electrocardiogram (ECG) demonstrated STEMI (ST-segment elevation ≥0.2 mV in ≥2 contiguous leads in V1 through V3 or ≥0.1 mV in other leads), and received abciximab prior to PPCI. Exclusion criteria were left bundle branch block, recent surgery, recent stroke, recent spinal trauma, haemorrhagic diathesis, severe liver or kidney failure and known contraindications for therapy with abciximab, aspirin, clopidogrel or heparin.
Study groups
Halfway during the study (December 2006), a new strategy for early abciximab administration starting in the ambulance was adopted within the MISSION! protocol (Figure 1).
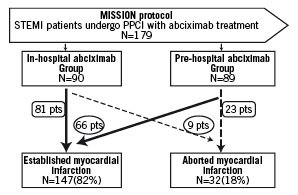
Figure 1. Flow chart for study design. STEMI: ST-segment elevation myocardial infarction; PPCI: primary percutaneous coronary intervention; pts: patients.
We enrolled 179 consecutive patients, who fulfilled the inclusion and exclusion criteria for this sub-study: 90 patients (in-hospital group); in whom abciximab was initiated in the coronary care unit or catheterisation laboratory before the intervention, then 89 patients (pre-hospital group); in whom abciximab bolus was given in the ambulance before transport to the catheterisation laboratory. The study complies with the Declaration of Helsinki. The MISSION! Protocol has been approved by the local ethics committee.
Electrocardiographic data collection
All patients had a high quality 12-lead ECG recorded at presentation as well as within 90 min after PPCI. ECGs were recorded at the patient’s home by trained paramedics with Lifepak-12 Defibrillator/Monitor Series (Medtronic Physio-Control, Redmond, WA, USA). If the ECG fulfiled the positive identification criteria of the pre-hospital MISSION! standard order form, the ECG was transmitted directly as a fax to the computer network of our hospital (Lifenet RS system; Medtronic Physio-Control, Redmond, WA, USA) and assessed by the attending cardiologist who determined the patient’s eligibility for PPCI, based on predefined criteria.6
Electrocardiographic data analysis
ST segment elevation was measured manually 20 ms after the end of the QRS complex (the J point) using a hand-held calliper. The sum of ST-segment elevation in leads V1 to V6, I, and aVL was added to the sum of ST-segment depression in leads II, III, and aVF for anterior MI. For inferior MI, the sum of ST-segment elevation in leads II, III, and aVF (and I, aVL, V5, and V6; if present) were added to the sum of ST-segment depression in leads V1 to V4.7 All ECGs were collected and analysed by an investigator blinded to the assigned treatment. Total ST-segment deviation at inclusion was compared to that taken within 90 minutes after PPCI. ST-segment resolution ≥50% of the initial ST-segment deviation was calculated.
Abciximab and additional medication
All patients received abciximab (Centocor, Leiden, The Netherlands) as a bolus injection of 0.25 mg/kg bodyweight, followed by 0.125 µg/kg/min with a maximum of 10 µg/min as a continuous infusion for 12 hours. All patients received an equivalent of 300 mg of acetylsalicylic acid, 600 mg clopidogrel as a loading dose, and heparin given as a bolus of 5000 IU at the start of the PCI procedure. After the procedure, all patients received aspirin (75 mg/day) indefinitely and clopidogrel (75 mg/day) for one year. Other medications were systematically prescribed according to MISSION! Protocol.6
Laboratory data
Creatine kinase (CK) activity (Roche Hitachi Modular P800, Roche Diagnostics, Basel, Switzerland; upper limit of normal [ULN]=200 U/L) and cardiac troponin-T (TnT) concentration (3rd generation Elecsys 2010 analyser, Roche Diagnostics, Basel, Switzerland); The detection limit of the assay is 0.01 μg/l. The decision limit used for diagnosis of MI is 0.03 µg/l, with an imprecision of <10%) in plasma were determined at admission and every six hours in the first 48 hours after PPCI. Subsequently these levels were determined every day up to discharge, unless clinical events suggested repeat measurements. The cumulative release of CK in the first 48 hours was calculated as a measure of infarct size in each patient by an investigator blinded to the assigned treatment.8
Invasive procedure and angiographic evaluation
Coronary angiography was performed by the femoral approach. All patients underwent PPCI and stenting of the Infarction Related Artery (IRA) according to standard techniques. Stent implantation was successfully completed in all patients. Procedural success was defined as residual stenosis <20% and TIMI flow grade 3. Initial and post procedural TIMI flow grade of the IRA9 were assessed off-line by two experienced interventionalists blinded to the assigned treatment.
Diagnosis of aborted MI
As this is the first study to evaluate the incidence of aborted MI in the PPCI era, we propose a (new) definition of aborted MI: In a well equipped centre for PPCI, aborted MI can be defined as a combination of the following: 1) typical chest pain >30 min with initial ST-segment elevation (indicative of transmural myocardial ischaemia), 2) ST-segment deviation resolution of ≥ 50% within 90 min post-PPCI, 3) peak CK release less than three times ULN within the first 48 hours post-PPCI, and 4) presence of a significant coronary artery stenosis at the territory of suspected ischaemia.
Statistical analysis
Categorical variables were presented as counts and proportions (percentages) and compared by Pearson chi-square analysis or Fisher exact test. Normal distribution of continuous data was tested using a Kolmogorov-Smirnov test. Continuous and normally distributed data are presented as mean ±1 SD and were compared by unpaired t test. Not-normally distributed data are expressed as median with interquartile range (IQR), and the Mann-Whitney U test was used to compare differences between two groups.
Univariable and multivariable logistic regression analyses were performed to characterise predictors of aborted MI. Categorical variables included pre- or in-hospital abciximab group, time to abciximab treatment (≤ 2 hours and > 2 hours), prior myocardial infarction, gender, hypertension, diabetes, hypercholesterolaemia and site of myocardial infarction, smoking habit, Killip class above I and age > 75y. Continuous variables included age, time from abciximab to balloon and sum of ST-segment elevation on admission ECG. Forward stepwise multivariable regression was performed using only variables with a probability value <0.05 at univariable regression analysis.
Receiver operator characteristic (ROC) curve was constructed to examine the relationship between peak TnT concentration and aborted MI. The ability of TnT to assign STEMI patients accurately into the two groups (aborted and established MI) was determined by calculating the area under the ROC curve. According to the Swets scheme for interpreting the area under the ROC curve,10 values of 0.5–0.7 indicate low diagnostic accuracy, values of 0.7–0.9 suggest limited clinical utility, and values >0.9 indicate high global diagnostic accuracy. The sensitivity and the specificity, at the best decision value were also calculated.
All p-values are two-tailed, and statistical significance was defined if p <0.05. All analyses were performed with SPSS version 14.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
The study population consists of 179 consecutive patients who underwent PPCI and were treated with abciximab according to the MISSION! protocol (Figure 1).
Patient characteristics
Baseline characteristics of the per- and in-hospital groups are summarised in Tables 1 and 2.
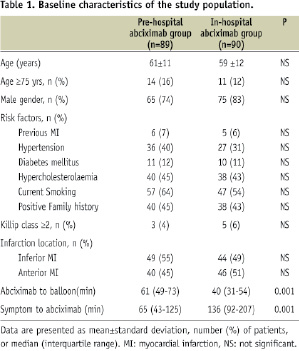
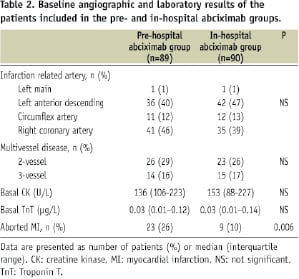
The two groups were well comparable, with no significant differences in baseline characteristics. As expected by protocol, the median time between symptoms onset and abciximab bolus administration was significantly shorter in the pre-hospital group (65 min, IQR 43-125 min) than in the in-hospital group (136 min, IQR 92-207 min). Table 2 reveals no significant differences between groups with regard to baseline angiographic and laboratory results.
Thirty-two patients (18%) fulfilled the criteria of aborted MI in the whole study population (Figure 1), 23 (26%) in the pre-hospital abciximab group and nine (10%) in the in-hospital group (p=0.006).
Characteristics of patients with aborted MI
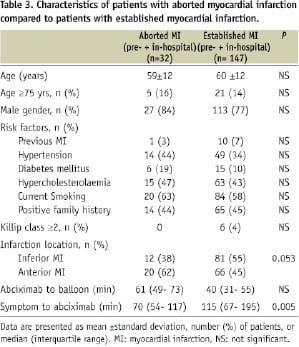
Table 3 compares patients with aborted MI (from both pre- and in-hospital groups) to those with established MI.
The two groups show no significant differences in baseline characteristics, although there was a trend toward increased incidence of aborted MI in patients with anterior MI compared to those with inferior MI (62% vs. 38%, p=0.053).
Time to treatment
The median time between symptoms onset and abciximab bolus administration was significantly shorter in the aborted MI (70 min, IQR 54-117 min) than in the established MI group (115 min, IQR 67-195 min). The occurrence of aborted MI categorised according to time from symptoms onset to abciximab treatment is shown in Figure 2, where aborted MI was most frequent within the first hour (28%) and deceased thereafter (p=0.02).
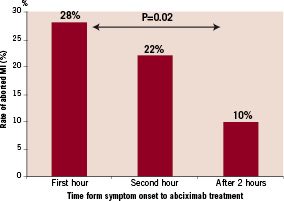
Figure 2. Rate of aborted myocardial infarction according to time from symptoms onset to abciximab treatment. MI: myocardial infarction. Time-dependency of rate of aborted MI is significant (p=0.02)
Furthermore, 79% of the patients in the aborted MI group received abciximab treatment within the first two hours after onset of symptoms compared to 57% in the established MI group (p=0.02) (Figure 3).
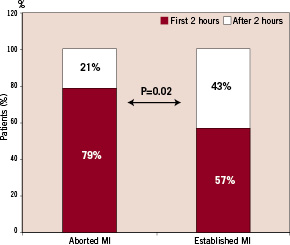
Figure 3. Incidence of aborted myocardial infarction and established myocardial infarction during and after first 2 hours from symptoms onset. MI: myocardial infarction.
The incidence of aborted MI in patients presented during the first two hours after symptoms onset was three times higher than in the established MI group (OR=2.94, 95% CI=1.1-7.7).
Angiographic results
Initial angiographic evaluations showed no significant differences between aborted and established MI groups regarding the infarction related artery and number of diseased vessels prior to PPCI (Table 4).
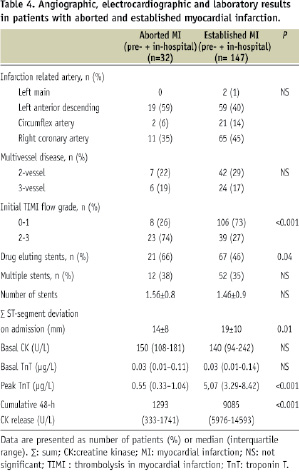
At initial angiography the aborted MI group showed higher early reperfusion rate of the IRA (TIMI 2-3 flow) compared to the group with established MI (74% vs. 27%; p < 0.001). The number of stents used did not differ between the aborted and established MI groups, although the use of drug eluting stents was higher in the aborted MI group (Table 4).
ECG and Laboratory results
Aborted MI patients had a significantly lower sum of ST-segment deviation on their ECG at time of admission compared to patients with established MI (p=0.01) (Table 4).
The baseline levels of serum CK and TnT did not differ between the aborted and established MI groups. Analysis of the peak values of TnT revealed significantly lower levels in the aborted MI group compared to the established MI group (Table 4). The cumulative 48 hour CK release was significantly lower in the aborted MI group than in the established MI group (Table 4).
When we assess the peak TnT for diagnosis of aborted MI in our patient population, TnT peak value <1.5 µg/L diagnose aborted MI with a sensitivity of 97.3 % and a specificity of 96.9%. ROC curve analysis produced an area under the curve of 0.99 (95%CI=0.98- 1.00, Figure 4).
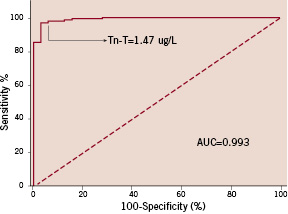
Figure 4. Receiver operator characteristic (ROC) curve analysis for peak troponin-T as a diagnostic test of aborted MI. AUC: Area under the ROC curve. Best decision threshold is shown (sensitivity is 97.3% and specificity is 96.9%).
Prediction of aborted MI
Time-from-symptom onset to abciximab treatment and ST-segment elevation at admission ECG were positively related to incidence of aborted MI (Table 5).
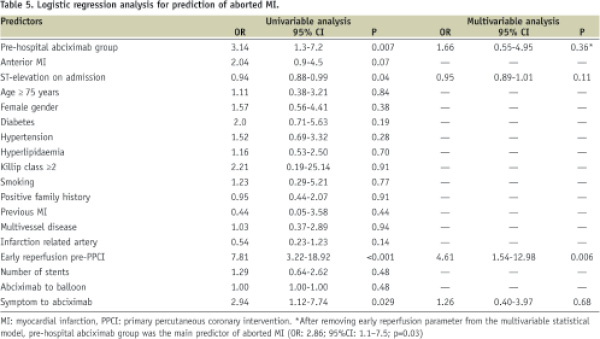
Pre-hospital abciximab administration was significantly related to incidence of aborted MI (OR=3.14, 95% CI=1.3-7.2). Anterior MI was not significantly related to aborted MI.
IRA patency (TIMI 2-3) pre-PPCI was the strongest univariable predictor (OR=7.81, 95% CI=3.2-18.9) and the only significant multivariable predictor of aborted MI (Table 5). The incidence of aborted MI was four times higher in patients with TIMI 2-3 flow at presentation (OR= 4.61, 95% CI=1.5-13.5). According to temporal sequence of events, initial IRA patency comes after abciximab administration, so after removing IRA patency from the multivariable analysis model, we identified only pre-hospital abciximab administration as an independent predictor of aborted MI (OR=2.86, 95% CI=1.1–7.5, p=0.03). Further analysis of the relation between these predictors, revealed significant correlation between the time to abciximab (r=-0.4, p<0.001) and initial IRA patency (r=0.36, p<0.001) with the group effect, so it is reasonable to assume that the per-hospital abciximab administration effect on incidence of aborted MI can be related to the initiation of treatment within the first two hours after symptoms onset and to the early reperfusion of the IRA.
Discussion
The key findings of this study are: 1) this is the first prospective study reporting an 18% incidence of aborted MI after PPCI using a novel and practical definition, 2) pre-hospital abciximab administration is associated with four times higher incidence of aborted MI as compared to in-hospital abciximab administration, 3) aborted MI occurs three times more often in patients presented during the first two hours after symptoms onset, 4) the main predictor of aborted MI is pre-hospital abciximab administration, and we assume that this effect is related to the initiation of treatment within the first two hours after symptoms onset and to the early reperfusion of the IRA.
There is no current standardised definition of aborted MI. The recent consensus document on universal definition of myocardial infarction11 did not contain a definition for aborted MI. The commonly used definition is peak CK ≤2 times ULN with dynamic ECG changes.2,3,7,12 However these definitions were formulated in the thrombolytic era, none of the previous definitions were proposed in the current era where PPCI is the recommended treatment of choice for patients with STEMI.13
Why not apply the previously suggested definition?
The use of coronary intervention for treatment of STEMI provides a unique opportunity to avoid any false positive diagnosis of aborted MI which is the main problem of the previous definitions. Masquerading MI or unjustified thrombolysis (chest pain with persistent ST-segment elevation and without significant CK enzyme rise) occur in around 2% of patients with suspected STEMI.7 The use of the new definition reduces this risk for false positive to zero.
Why 3 times and not 2 times ULN of CK?
According to the recent consensus document for the universal myocardial infarction definition, balloon inflation during PCI almost always results in ischaemia with or without ST-T changes. The procedure related cell necrosis can be detected by cardiac biomarkers measured before, immediately after the procedure, and again at 6-12 hours and 18-24 hours.11 However, there is currently no solid basis for defining a biomarker threshold for the diagnosis of periprocedural myocardial infarction in the PPCI era.11 So two times ULN of the cardiac marker can be applied in the thrombolytic era, but not in the PPCI era. Therefore, we increased the cut-off point to three times ULN of CK.
Why not assess troponin instead of CK?
It is uncertain whether the use of the troponin as a more sensitive marker of myocardial necrosis may change the definition of aborted infarction. The studies on aborted infarction originate from a time period when troponin measurements were not included in the trial designs.2 Moreover, even in the present era, troponin levels are not routinely used as a risk stratifier in ST-segment elevation acute coronary syndromes, as they are in non-ST-segment elevation coronary syndromes.2 No studies are available about the precise value of troponin to diagnose aborted MI. Therefore, we suggested a cut-off point of 1.5 µg/L of troponin-T to diagnose aborted MI, in future studies with a high diagnostic accuracy.
Incidence of aborted MI
Aborted infarction has been observed in 13–17% of patients after fibrinolysis.7,12,14 This incidence rises to 25% of patients treated within one hour after symptoms onset.7 In our study, aborted MI is observed in 18% of patients after PPCI. To our knowledge, this is the first prospective study that reports the rate of aborted MI after PPCI.
Time-to-treatment
In our study, aborted infarction is strongly related to shorter time to abciximab treatment in concordance with prior studies, in which aborted infarction was strongly related to a shorter time to fibrinolytic.7,12 Lamfers et al14 have reported that time-to-treatment was shorter in patients with aborted MI compared to those with established MI (86 vs. 123 min, p=0.05). In the present study we report similar results with somewhat shorter time to abciximab administration (70 vs. 115 minutes, p=0.005) which can be attributed to differences in study design. Taher et al7 have reported that aborted MI was most frequent in the first hour (25%), and decreased thereafter (10% by 3 hours), while in our study 28% of aborted MI occurred within the first hour.
Lamfers et al14 have reported that aborted MI occurred four times more frequently in patients treated with pre-hospital thrombolysis than in patients treated with in-hospital thrombolysis. These results are in conjunction with our results showing that, pre-hospital abciximab administration is associated with four times higher incidence of aborted MI than in-hospital administration.
Predictors and pathophysiology of aborted MI
Abortion of MI is thought to follow rapid early reperfusion of a thrombotic occlusion of an epicardial coronary artery such that myocardial necrosis cannot be detected by classical plasma biomarkers.2 Lamfers et al14 have reported that short time-to-treatment, low ST elevation at presentation, and pre-infarction angina were independent predictors of aborted MI. In our study early reperfusion of the IRA pre-PPCI is the only multivariable predictor of aborted MI. However, by further analysis we assume that the pre-hospital abciximab administration is the main predictor of aborted MI, and this effect can be related to the initiation of treatment within the first two hours after symptoms onset and to the higher IRA patency (TIMI 2-3) at presentation.
A recent report by Tarantini et al15, who studied magnetic resonance images of aborted MI after PPCI, suggested that myocardial oedema in the absence of late enhancement seems to be the magnetic resonance marker of aborted MI.
On the other hand, aborted MI may also occur in the absence of reperfusion therapy as a spontaneous variant of ‘stuttering’ infarction.2,7,12 It has been postulated that in a subset of patients with suspected ST-segment elevation acute coronary syndromes, there is a subtle balance between coronary thrombosis and endogenous fibrinolysis, sometimes modulated by vasoconstriction, resulting in intermittent occlusion and spontaneous reperfusion.
Study limitations
Our study is an observational prospective, single-centre study. Time of abciximab administration was not randomly assigned for the study groups. However, throughout the study period, a rigorously standardised protocol (MISSION!) concerning pre-, peri- and post-PPCI treatment was applied. So it seems unlikely that procedural changes over time other than the timing of abciximab administration have influenced the incidence of aborted MI.
Conclusions
In patients with STEMI treated with PPCI, the incidence of aborted MI was 18%. Pre-hospital abciximab administration was the main predictor of aborted MI, and this effect was related to the initiation of treatment within the first two hours after symptoms onset and to the higher IRA patency at presentation.
Acknowledgements
Funding for this work was provided by Leiden University Medical Center.

