Abstract
The proposed 2020 Core Curriculum for Percutaneous Cardiovascular Interventions aims to provide an updated European consensus that defines the level of experience and knowledge in the field of percutaneous cardiovascular intervention (PCI). It promotes homogenous education and training programmes among countries, and is the cornerstone of the new EAPCI certification, designed to support the recognition of competencies at the European level and the free movement of certified specialists in the European Community. It is based on a thorough review of the ESC guidelines and of the EAPCI textbook on percutaneous interventional cardiovascular medicine. The structure of the current core curriculum evolved from previous EAPCI core curricula and from the “2013 core curriculum of the general cardiologist” to follow the current ESC recommendations for core curricula. In most subject areas, there was a wide - if not unanimous - consensus among the task force members on the training required for the interventional cardiologist of the future. The document recommends that acquisition of competence in interventional cardiology requires at least two years of postgraduate training, in addition to four years devoted to cardiology. The first part of the curriculum covers general aspects of training and is followed by a comprehensive description of the specific components in 54 chapters. Each of the chapters includes statements of the objectives, and is further subdivided into the required knowledge, skills, behaviours, and attitudes.
Introduction
The present version of the Core Curriculum for Percutaneous Cardiovascular Interventions was organised and developed by the Education and Training Committee (ETC) of the European Association of Percutaneous Coronary Interventions (EAPCI), under the leadership of EAPCI Presidents Michael Haude and Andreas Baumbach.
In most countries, the prevalence of coronary artery disease (CAD), valvular heart disease (VHD), peripheral vascular disease (PVD) and heart failure (HF) is increasing. This relates both to the progressive ageing of the population and to a better identification of these diseases. To date, cardiovascular disease remains the leading cause of death worldwide. In Europe, ischaemic heart disease now accounts for almost 1.8 million annual deaths while VHD is becoming a pressing clinical issue1,2.
The main areas of the percutaneous cardiovascular interventional field, as covered by the interventional cardiologist (IC), are percutaneous coronary interventions (PCI), transcatheter valvular interventions, percutaneous interventions for PVD (including those for ischaemic stroke), and percutaneous interventions for HF (including those for cardiogenic shock).
The broad use of these interventions is supported by overriding scientific evidence and has been associated with durable benefits for both individuals and populations3,4,5,6,7,8,9,10,11,12. In this context, ensuring quality of patient care, and clinical excellence in percutaneous cardiovascular interventions are of the utmost importance. The completion of a dedicated curriculum provides the IC with the knowledge, skills, behaviours and attitudes to act as an expert in the invasive physiological and anatomic assessment, diagnosis, and management of coronary and structural heart diseases as well as in the invasive management of HF and PVD.
The first and only “Curriculum and syllabus for Interventional Cardiology subspecialty training in Europe” was published in 2006 by di Mario et al on behalf of the “Working Group 10 of the ESC” (which later became the EAPCI) and a panel of experts in education including the chairmen of the national interventional societies, coordinated by the European Board for the Specialty of Cardiology (EBSC)13. This document was very ambitious and addressed the need for a certified, uniform, training programme, before cardiologists engage in interventional procedures that carry a potential risk. It was divided into several parts: rationale and aims of the curriculum, structure of the training programme, assessment methods, organisation of the training and, importantly, a syllabus-specific programme content with several chapters (basic science, pharmacology, imaging, indication for treatment and patient selection, procedural techniques, management of complications of percutaneous intervention and miscellaneous). Some procedures were not considered to be part of the core curriculum but rather an “optional” part of the training.
The 2006 visionary document set the European standards although these were not broadly adopted. The present approach intends to overcome the main limitations identified in the previous document, namely its endorsement and promotion by the interventional and general cardiology societies. The proposed core curriculum aims to support the educational requirements and to fill the gap of an updated European consensus that defines the level of competences in the field of percutaneous cardiovascular intervention. It promotes homogenous education and training programmes in interventional cardiology among countries, and is the cornerstone of the new EAPCI certification, designed to support the recognition of knowledge, skills, behaviours and attitudes of newly trained interventional cardiologists.
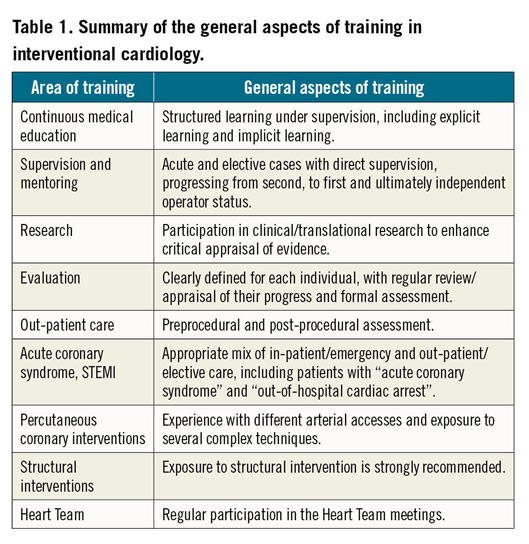
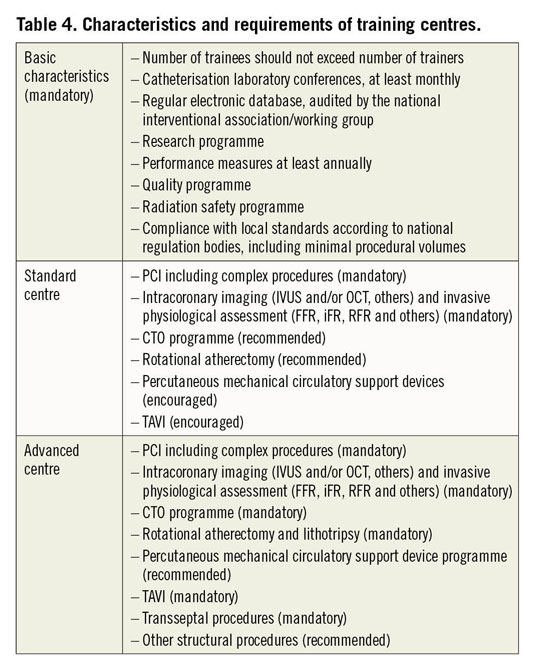
Considering the distinct realities among European and other countries and because numbers are not sufficient per se to describe the proficiency of an IC, the present document is not recommending minimal procedural volume for trainees or for training centres. It is rather providing guidance on the “achievements” and on the “levels of competence” which have to be acquired by the trainees (Table 1-Table 3). We also provide detailed information on how a training centre will have to be organised, including the need to involve at least two ICs with more than five years’ experience dedicated to the percutaneous cardiovascular interventional field (Table 4).
The EAPCI has designed a new two-part certification process: part A (theoretical) and part B (practical). Part A is a multiple choice question (MCQ) exam held twice a year, based on the present core curriculum, as well as the EAPCI Textbook of Interventional Cardiology, the ESC General Cardiology Core Curriculum and the content of the Fellows Course of the EAPCI. The exam was successfully launched at EuroPCR 2018 in Paris. Part B, which is currently under final development, is based on the recognition of acquisition of the competencies listed in Table 4 of the present document. To prevent duplication, and simplify the process, it will preferably be conducted through a very strong interaction with national certification programmes when such programmes exist (i.e., mutual recognition process) and/or a direct interaction with training centres. The model of the present EAPCI certification, in which full certification requires acquiring the two parts, is very similar to those developed by the other subspecialty associations of the European Society of Cardiology (ESC).
The EAPCI ETC Committee launched the project under the auspices of Professors Michael Haude and Andreas Baumbach. A total of 10 groups, consisting of two to three interventional cardiologists each, developed, circulated and improved the document under the direction of the successive Chair and Co-Chair of the ETC, Professors Dariusz Dudek and Eric Van Belle and Doctor Rui Campante Teles. The document was revised by the Chair and Co-Chair of the ETC, Professor Eric Van Belle and Doctor Rui Campante Teles, as well as the current EAPCI President, Professor Andreas Baumbach, and President Elect, Professor Dariusz Dudek.
The 2020 Core Curriculum underwent a thorough review process based on the template of the review of the ESC guidelines and of the EAPCI textbook on percutaneous interventional cardiovascular medicine. The document does not include minimum or optimal numbers of procedures to be undertaken, and does not address periodic evaluation or revalidation. It defines the clinical, patient-oriented, training of the IC. The structure of the current core curriculum has been drastically modified as compared to the previous version and has evolved from the “2013 Core Curriculum of the general cardiologist” to follow the current ESC recommendations for core curriculums. In most subject areas, there was a wide if not unanimous consensus among the task force members on the training required for the IC of the future. The document recommends that acquisition of competence requires at least two years of training in interventional cardiology, in addition to four years devoted to cardiology.
The first part of the curriculum covers general aspects of training and is followed by a comprehensive description of the specific components in 54 chapters. Each of the chapters includes statements of the objectives, and is further subdivided into the required knowledge, skills, behaviours, and attitudes.
The core curriculum for the interventional cardiologist
THE CLINICAL FIELD OF INTERVENTIONAL CARDIOLOGY
The clinical specialty of interventional cardiology aims to deliver expert interventional care for patients presenting with disorders of the heart, the systemic, and the pulmonary circulations. This core curriculum provides the standards for training in interventional cardiology, as well as a template for the maintenance of competence for qualified cardiologists.
The IC is the subspecialist who performs percutaneous interventional cardiovascular procedures. He/she is primarily a medical specialist with a thorough basic training in internal medicine who has completed an approved cardiology fellowship programme incorporating the knowledge demanded by the ESC Core Curriculum for the general cardiologist14. Interventional cardiologists perform general cardiac investigation and management of patients with suspected or established cardiovascular disease using non-invasive methods and are involved in the comprehensive management of the patient and treatment of the underlying disease, not only focused on procedural considerations. They have the ability to consider and apply interventional techniques to the global care of patients. They are team workers who interact closely with other cardiologists and other medical specialties, nurses, paramedics and other healthcare professionals.
In order to master the invasive techniques, there are skills in several general fields which are important for the IC and require special differentiation that complement basic general cardiology skills. It is recommended that an operator be able to interpret the most advanced cardiology imaging techniques required for periprocedural assessment, especially echocardiography, computed tomography and endovascular studies. A high level of cardiac intensive care experience is requested, with a special emphasis on acute heart failure and arrhythmia management14.
As simulators have shown benefit in the progress of novice operators, they are progressively being incorporated into training programmes and courses15,16. While the exact role of these simulators in most advanced technical skills still needs to be clarified, with their progressive sophistication their use in the training of ICs will continue to increase.
A key role of the IC is to perform emergency procedures for reperfusion of acute myocardial infarction in 24/7 PCI-capable centres. Regarding PCI, any operator is expected to be fully competent regarding the entire spectrum of patient evaluation, information, techniques and follow-up, including all advanced techniques such as imaging, physiology, adverse clinical presentations and anatomies and adverse lesion scenarios, incorporating calcification, degenerated grafts, simple chronic total occlusions (CTOs) and bifurcations in general. An IC is expected to be fully skilled in the management of any procedural complications.
Concerning the increasing importance of transcatheter aortic valve implantation (TAVI), any operator should be prepared to conduct complete preprocedural evaluation of TAVI candidates and collaborate with a valvular Heart Team to select the most suitable treatment.
Concomitantly, these fields are continuously expanding and, in certain cases, a very specific training to master a procedure or technique is required. Help from a proctor is recognised as advantageous or an appropriate referral to a more skilled centre might be advisable, especially in certain areas that, depending on the individual and the centre, require a particular expertise, namely complex coronary interventions, stroke, PVD, grown-up congenital heart (GUCH) disease, mitral or tricuspid valve disease, left atrial appendage occlusion (LAAO), etc.
The spectrum of expertise is broad and, in addition to the procedures, includes a comprehensive patient risk assessment that is fundamental for patient information and integrates medical decision making. A multidisciplinary management strategy is essential including a heart failure specialist, imaging specialist, surgeons, geriatrician, anaesthetist and cardiac rhythm specialists17.
Because these interventions are applied to a very large population of patients, their economic impact has become significant. The IC must be conscious of this economic burden and responsible for the appropriate utilisation of devices and therapies.
The process for medical decision making and patient information is guided by the “four principles” approach to healthcare ethics - autonomy, beneficence, non-maleficence and justice. The IC represents the patient’s best interest and therefore the medical decision process must be independent and be performed according to the best available evidence, in order to deliver optimal patient-centred care. Moreover, because this is a very technological and continuously demanding evolving medical area, it requires lifelong learning and continuous updating of his/her knowledge. The IC is expected to be engaged in structured clinical investigation programmes and to collaborate actively in patient follow-up.
GENERAL ASPECTS OF TRAINING IN THE SPECIALTY
Candidates for interventional training should be physicians licensed to practise in the country of training. The trainee must have the necessary linguistic ability to communicate with patients and colleagues in the country of training and later in the country of practice. The trainee should have completed a minimum of four years of full-time training in general cardiology.
The recommended minimum duration of dedicated subspeciality training should be two years of full-time and exclusive training in interventional cardiology.
To gain sufficient experience, the trainee should gain exposure to all aspects of interventional cardiology, with an appropriate mix of in-patient/out-patient and emergency/elective care, including the elements described below and summarised in Table 1:
– Participation in the clinical management of in-patients, with an emphasis on patients presenting acutely to the coronary care unit (CCU) and acute medical unit (AMU) with acute coronary syndromes (ACS).
– Regular on-call commitment providing a primary PCI service for patients presenting with ST-elevation myocardial infarction (STEMI) and/or out-of-hospital cardiac arrest (OHCA).
– Regular attendance and/or coordination of Heart Team meetings.
– Bedside patient care, including preprocedural and post-procedural assessment.
– Structured learning, under the direct supervision of educational supervisors/nominated trainers, which may include (a minimum of two hours/day is suggested):
– explicit learning: journal club, postgraduate teaching, exercises in evidence-based medicine, discussion of guidelines for clinical practice, national/international symposia/congress attendance.
– implicit learning: ward rounds, case-based discussions, supervised acquisition of diagnostic and interventional skills.
– Interventional training should include a mix of acute and elective cases with direct supervision, progressing from second, to first and ultimately independent operator status by the end of the training period.
– Interventional training should guarantee experience with arterial access (femoral and radial), and with the most frequent of the complex techniques, including bifurcation strategies, treatment of calcified vessels, intravascular imaging, and functional assessment of coronary stenoses (FFR, iFR, etc.).
– Exposure to chronic total occlusion (CTO) strategies, with both antegrade and retrograde approach, atherectomy techniques including rotablation, haemodynamic support/mechanical circulatory support, is required.
– Exposure to structural intervention including TAVI, mitral and tricuspid valve treatment, atrial septal defect/patent foramen ovale/left atrial appendage closure, and paravalvular leak/ventricular septal defect closure is strongly recommended.
– The training programme should be clearly defined for each individual, with regular review/appraisal of their progress and formal assessment of their knowledge and procedural competencies.
– Participation in clinical/translational research in interventional cardiology is recommended to enhance critical appraisal of evidence.
Learning objectives should be clearly defined and are preferred to recommendations based solely on the time spent in a particular department or on the number of procedures performed. The objectives should include knowledge, and specific and generic skills including communication and appropriate behaviours, competencies and attitudes that will be further reinforced during ongoing training.
LEARNING OBJECTIVES
These are specific aims which demonstrate skills acquired by the trainee at the end of the course. They are based on the trainee’s capabilities in certain tasks. Specific objectives are classified according to knowledge, skills, and behaviours and attitudes.
– Knowledge: describes requirements for trainees. The subject matter is defined by the EAPCI Core Curriculum chapters. This knowledge includes pathology of diseases as the rational basis for long-term learning.
– Skills: a practical application of knowledge acquired from experience and training to solve practical problems, make clinical decisions and perform specific procedures.
– Behaviours and attitudes: refer to those attitudes and behaviours that lead to optimal clinical performance.
CATEGORIES AND LEVELS OF COMPETENCE
First-hand exposure and practical experience are crucial in the learning of techniques. However, the number of procedures performed by trainees is not considered an exclusive measure of performance. The authors acknowledge the variability of the learning curve among individuals and the impact of the training centre volumes on the learning process. Thus, this document focuses on the acquisition of competencies rather than on procedural volume.
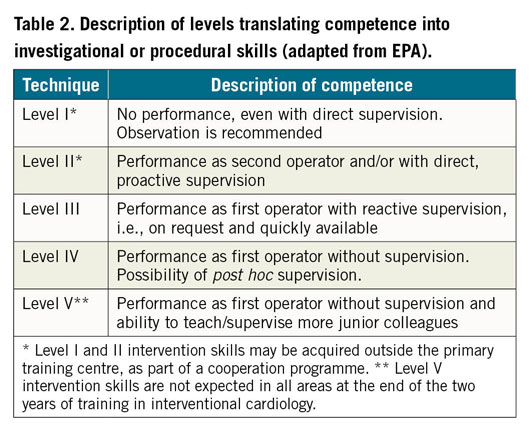
This section describes the levels to translate competencies into investigational or procedural skills. Their ascending order is defined as follows and summarised in Table 2. It has been adapted from the description of Entrustable Professional Activities (EPA)18:
– Levels I and II. The trainee must have acquired experience in selecting an appropriate diagnosis or therapy and in interpreting results or choosing an appropriate treatment for a referred patient.
– Level I does not require any procedural skills, yet participation in related procedures during training may be valuable.
– Level II of competency indicates acquisition of some procedural skills as operator, usually as assistant/second operator, obtained in the primary or external training centres.
– Level III. The trainee must be able to interpret clinical data, recognise treatment indications, and perform the technique or procedure and manage related complications, as first operator, but still requires to work under the direct supervision of a senior IC operator.
– Level IV. The trainee must be independent in the ability to interpret clinical data, recognise treatment indications, perform the technique or procedure and manage related complications, as first operator without the direct supervision of a senior IC operator. Post hoc supervision including case review with more senior colleagues is possible.
– Level V. Same as level IV. In addition, it includes the ability to teach and supervise the technique or procedure to more junior colleagues.
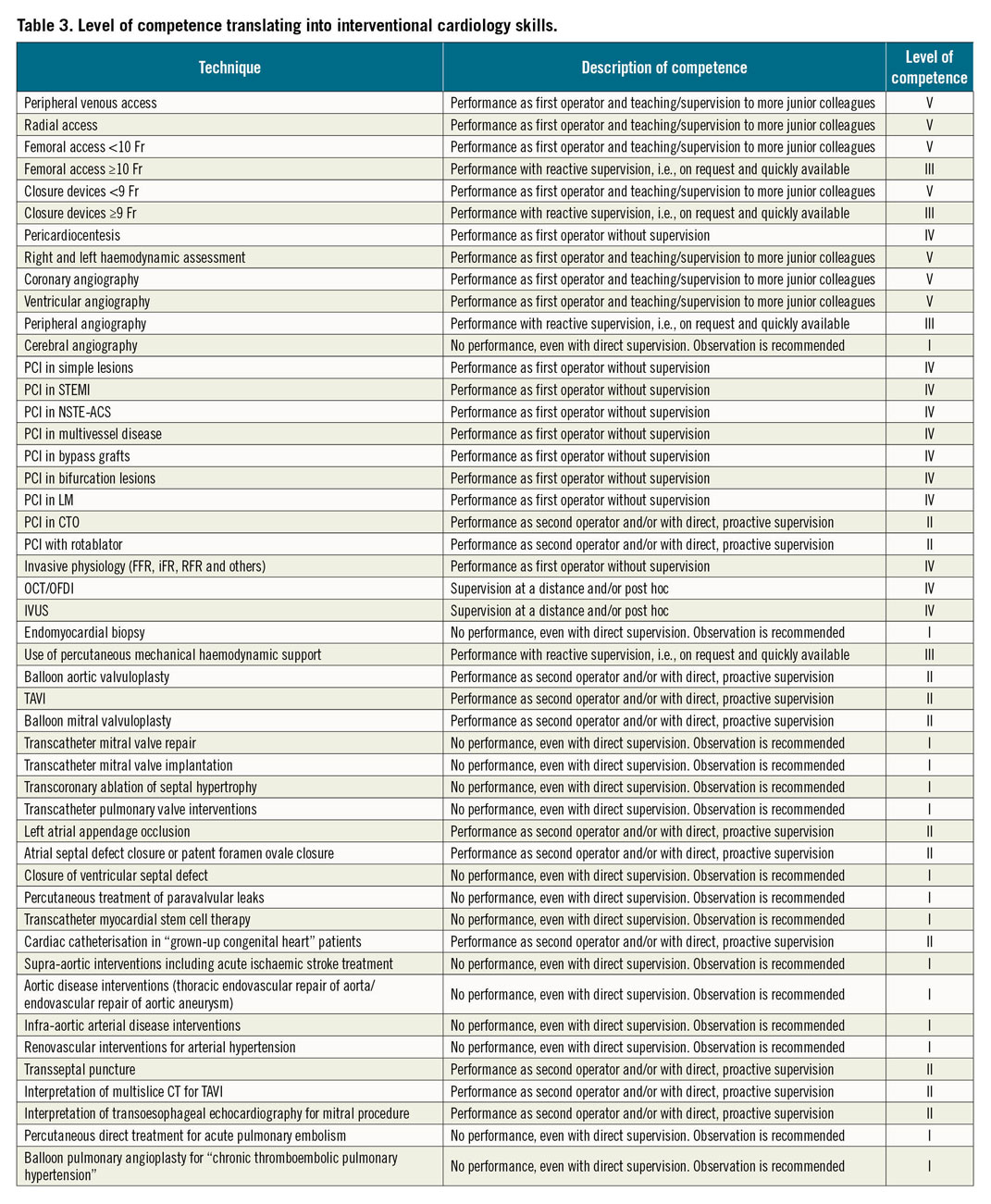
Table 3 summarises the level of competence translating into interventional cardiology skills that the EAPCI considers desirable for a trainee in interventional cardiology to achieve at the end of his/her two years of training19,20,21,22,23,24. Although organisation of cardiac services and resources for training are not uniform across Europe and ESC member countries, the core curriculum aspires to an optimal, rather than a minimal standard. In countries or centres that are currently unable to deliver training in all aspects required, the core curriculum should be used as a benchmark to promote policies for improvement. Also, rotation of trainees between different centres may provide an adequate solution.
REQUIREMENTS FOR TRAINING INSTITUTIONS AND TRAINERS
REQUIREMENTS FOR TRAINING INSTITUTIONS
General aspects
We believe that training institution profile and performance are as important as trainers’ profile and expertise in order to provide objective and quality interventional training. In order to comply with EAPCI standards, the institutions must be standardised using procedural volume reports and performance measures.
A training institution/centre for interventional cardiology should include a cardiac catheterisation laboratory with on-call 24-hour PCI availability and a dedicated cardiology unit, department or ward, in order to manage patients throughout hospitalisation. The trainee should be able to be educated to manage patients from their admission, through the invasive procedure, to discharge from the ward. Institutional workflow allowing the interventional cardiology programme attendees to follow the patient throughout their hospitalisation is mandatory.
The training centre should have an independent interventional cardiology unit, allowing the trainee to follow the patient from the beginning to the completion of interventional treatment. Units not integrated into a cardiology department (run as a service without dedicated beds) can exceptionally be considered if they demonstrate a well-developed structured co-operation with cardiology wards where the patients are admitted, allowing the interventional cardiology programme attendees to follow the patient throughout their hospitalisation.
Training centres should be encouraged to incorporate on-site interventional cardiology simulators or to provide simulation sessions during the IC training, especially during the early phases of training of the trainee and/or the techniques15,16.
Training centres should have the following basic characteristics (summarised in Table 4):
1) Active clinical research programme and/or involvement in clinical trials is mandatory for both types of centre.
2) Number of trainees per institution should not exceed the number of faculty members/trainers.
3) Heart Team meetings, including participation by clinical cardiologists, interventional operators, and cardiothoracic surgeons should be planned regularly (i.e., weekly or bimonthly).
4) Regular database - electronic database of diagnostic and interventional procedures regularly audited by the national interventional society is recommended to ensure centre quality.
5) Performance measures report of the institution (periodic, at least annual): in-hospital mortality in acute, elective PCI and diagnostic catheterisation.
6) Regular “quality assessment and quality improvement” (QA/QI) programme including radiation safety programme.
We further define two types of training centre: standard and advanced training centre (Table 4).
– Standard centre: must have a (mandatory) programme of 24 hours a day availability of PCI on call for STEMI/NSTEMI patients and a working hours regular programme for all kinds of patients. Availability of IVUS and/or OCT and assessment of intracoronary pressure-based physiology indices such as FFR/iFR is mandatory. It is strongly recommended that these centres are involved in complex PCI, including left main and multivessel disease. Availability of left ventricular assist devices such as IABP/Impella® (Abiomed, Danvers, MA, USA) is desirable but not mandatory as well as a CTO programme, rotational atherectomy and similar procedures. Institutional coronary and structural Heart Teams are also encouraged, even if the centre does not perform TAVI.
– Advanced centres: these have similar requirements to standard centres and should have a structural heart programme including at least TAVI according to national regulation, transseptal procedures and a structured CTO programme. Other structural procedures (stroke, carotid, peripheral, GUCH, septal ablation, left atrial appendage occlusion, paravalvular leak closure, etc.) are recommended. The presence of a Heart Team is mandatory.
– A centre may develop other programmes for peripheral interventions (stroke, carotid stenting, aorta, peripheral limb), treatment of adult congenital heart disease, performance of septal ablation for hypertrophic cardiomyopathy, etc.
Procedural volumes and public metric reporting
It has been established that the procedural volumes of centres have a significant impact on the availability of training opportunities and on performance measures and intervention outcomes, but numbers are insufficient to define the quality of a centre and their ability to train interventional fellows. Public reporting of centre training programmes, procedural volumes and clinical outcomes is advisable to guide trainee choice of the training centre. While the present document does not make recommendations on specific procedural volumes, training centres should comply with local standards according to national regulation bodies, including minimal procedural volumes.
REQUIREMENTS FOR TRAINERS
General aspects and levels of competence
Trainers should be graded as trainers in standard institutions (standard trainers) and trainers in advanced institutions (advanced trainers). Trainers should be experts for levels of competence III, IV and V (Table 2, Table 3). It is not required that every trainer be expert in those techniques for which a level of competence I or II (Table 2, Table 3) is required, provided trainees can rotate to train with an IC (in the same or different institution) with the necessary expertise.
Ideally, the number of trainers (full-time equivalent) should match or exceed the number of trainees. Delivery of the curriculum may be facilitated by a structure that includes a director of training (national/regional), a cath lab director (or supervisor), a training mentor (or educational mentor), and multiple clinical trainers (or clinical mentors).
The training mentor (or someone else involved in the organisation of training) should be responsible for organising the training programme in interventional cardiology, coordinating external rotations to referral centres, attendance at courses and congresses, and organising structured learning. It is necessary that both trainee and training mentors be subject to periodic assessment.
Number of trainers and their expertise
At least two trainers (supervisors) must be available, with more than five years’ experience dedicated to interventional cardiology as their main clinical activity. These trainers should be members of the permanent staff and should be able to deliver the procedural skills associated with levels of competence III, IV and V in the learning objectives (Table 2, Table 3).
In advanced centres, trainers should have experience of more than five years performing advanced heart interventions.
Trainers without personal expertise in these additional skills described in the learning objective (levels of competence I and II, Table 2, Table 3) should make them available to trainees through a cooperation programme with other trainers (or other institutions) who will deliver the formal training on these techniques. A similar five years of experience is required for the trainers delivering training on each one of those additional procedural skills.
The cath lab director must be responsible for the interventional unit and should ensure that the trainee fulfils his/her learning objectives. The training mentor must also ensure that the trainee attends the formal training courses and is involved in the research and educational activities of the department.
Conflict of interest statement
A. Baumbach received institutional research support from Abbott Vascular, consultation and speaker fees from AstraZeneca, Sinomed, MicroPort, Abbott Vascular, Cardinal Health, KSH, and Medtronic. R. Estevez-Loureiro reports grants and personal fees from Abbott Vascular and personal fees from Boston Scientific, outside the submitted work. A. Geppert reports lecture fees from Medtronic, Abbott and Abiomed, consulting fees from Abbott and Abiomed, congress grants from Asahi and Terumo, outside the submitted work. J. Kefer reports proctorship and speaker fees from Medtronic and Abbott, and speaker fees from Servier. D. Milasinovic reports personal fees from Abbot, Biosensors, Terumo, AstraZeneca and Sanofi, outside the submitted work. D. Muir is a proctor and advisory board member for Abbott Vascular, and received proctor, advisory board and speaker fees from Edwards Lifesciences. A.S. Petronio received proctor and advisory board fees from Abbott Vascular, and received proctor, advisory board and speaker fees from Edwards Lifesciences. G. Pires-Morais received speaker fees from Abbott Vascular. S. Pyxaras received consultancy fees from Abiomed and Boston Scientific and proctor fees from Boston Scientific. R. Parma received speaker fees from Boston Scientific, Edwards Lifesciences and Medtronic. F. Saia reports personal fees from Abbott Vascular, Boston Scientific, Edwards, Medtronic, Biotronik, Amgen, AstraZeneca, Daiichi Sankyo, Bayer and Boehringer-Ingelheim, outside the submitted work. N. Van Mieghem reports advisor fees from PulseCath BV and Abiomed. S. Windecker reports grants from Abbott, Amgen, BMS, Bayer, Boston Scientific, Biotronik, Cardinal Health, CSL Behring, Daiichi Sankyo, Edwards Lifesciences, Johnson and Johnson, Medtronic, Quebert, Polares, Sanofi and Terumo, outside the submitted work. E. Van Belle reports personal fees from HeartFlow and Philips, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.