Abstract
Aims: A tentative evaluation of doses received by patients undergoing international cardiolfgy (IC) procedures was carried out in France in June 2006 by the GACI. A pilot survey was performed aiming at: a) demonstrating the feasibility of the adopted approach towards estimating patient exposure; b) getting a first estimate of national diagnostic reference level (DRL) values; c) gathering experience on data collection in view of nationwide future studies.
Methods and results: Nineteen catheterisation laboratories provided data on 813 IC procedures (496 coronarography (CA) and 317 PTCA) performed by 60 cardiologists on 29 different installations.
Data gathered for each procedure were: patient characteristics, dosimetry indicators (DosexArea Product, fluoroscopy time, number of frames) and examination details (number of severe lesions, number of stents, etc.).
In spite of their overall compliance with international DRL values, dosimetric indicators showed large variations. Maximum to minimum ratios ranged from 60 to 160 for the DAP, from 80 to 60 for the fluoroscopy time and from 25 to 30 for the number of images for CA and PTCA respectively.
Conclusion: Findings highlighted key aspects of IC practice which should be improved from the radiation protection point of view: training of cardiologists, awareness of equipment performance and optimisation of procedures.
Introduction
Assessing patient exposure due to complex interventional procedures is one of the most important requirements of the Council Directive 97/43/Euratom1 on health protection of individuals against the dangers of ionising radiations in relation to medical exposure.
Ensuring that such exposures comply with the optimisation principle of radiation protection while avoiding any patient’s skin injury2 represents an ideal goal toward which the interventional cardiology community should be converging through the implementation of modern and appropriate radiation protection options.
Within this general framework, and in the absence of any previous information on patient exposure, the Groupe Athérome coronaire et Cardiologie Interventionnelle (GACI), a subgroup of the French Society of Cardiology, launched an initiative in June 2006 aimed at assessing the so-called “diagnostic reference levels” (DRL) for both coronary angiography and PTCA currently performed in catheterisation laboratories (CL) in France.
A tentative evaluation of doses received by patients undergoing diagnostic as well as therapeutic cardiology procedures was therefore carried out through a pilot survey performed in nineteen interventional cardiology centres.
The objectives of the survey were threefold:
a) to demonstrate the feasibility of the adopted approach towards estimating patient exposure;
b) to get a first estimate of DRLs in France and make the provisional results usable as a tool to promote the optimisation of patient radiation protection at the level of each interventional cardiology centre;
c) to gather experience on data collection in view of nationwide future works on this subject.
Method
The survey dealt with CL where at least one cardiologist, a member of GACI, had previously participated in a training course on both staff and patient radiation protection.
Originally 55 CLs were asked to participate to the survey, provided they complied with a minimal set of conditions: equipment available with a dose-area product measuring device and ability to return recorded data by means of either local software or a detailed questionnaire sent to them in advance.
Thirty-five CLs out of 55 answered favourably, but due to default of adequate dosimeter device availability or other local restrictions, only 19 were finally included in the survey. The radiological equipment involved in the survey comprised 29 installations (50% of which were fully digital with a flat panel detector) representing seven models from three different manufacturers.
Considering the limited scope of the survey, neither preliminary quality control checks of equipment, nor dedicated calibration of dose area product measuring devices were carried out before the survey. Knowing that, in general, most DAP meters are not calibrated on a regular basis, this would result in an uncertainty of DAP values of ±30%3-5.
In order to analyse the results of the survey, a central data management was set-up at the Centre d’Assurance de qualité des Applications Technologiques dans le domaine de la Santé (CAATS) which coordinated the survey and sent out the questionnaires to the different participating centres.
Each CL was required to provide CAATS with at least twenty consecutive procedures (diagnostic and/or therapeutic). The survey addressed both categories of cardiologists: those having followed the training course on radiation protection previously mentioned, and others who did not participate in that course.
For each procedure, the following data were gathered: patient characteristics (sex, age, height and weight, main risk factors: smoking, diabetes, etc), relevant dosimetry indicators (DAP-value, fluoroscopy time, number of runs, number of frames) and examination details (ID code for the practitioner, number of severe lesions, number of stents and balloons used). Patient identity was preserved according to current ethical regulations.
Between mid-June and mid-July of 2006, data on both diagnostic and interventional coronary procedures were collected from 12 CLs through questionnaires and from 7 CLs through their own software (CARDIOREPORT & ANGIOQUERY software respectively).
All CDroms containing the images (anonymous copy in DICOM format) recorded for each patient were centrally collected for further evaluation.
In order to assess the DRL of the survey, a two-step procedure was followed: a) each dosimetry related parameter was averaged over the total number of patients examined in a given CL, thus providing a mean value for the considered interventional cardiology centre; b) the third quartile value of the distribution of the mean values of different centres was assessed, thus providing the DRL.
Finally, as commonly adopted by other authors dealing with DRL evaluation, both ad hoc and PTCA procedures alone were put together into the same category hereafter named as PTCA.
In the following, due to asymmetrical distribution of variables, summary statistics are expressed preferably in terms of median, quartiles, interquartile range values (3rd minus 1st quartile), as illustrated in Figure 1; comparisons between groups are made using Mann-Whitney U-Test for rejecting the null hypothesis that there is no significant difference.
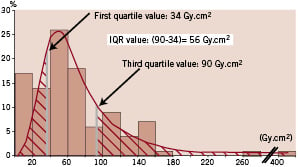
Figure 1. Example of DAP value distribution for PTCA.
Results
Among the 813 procedures gathered through the survey, 496 procedures were coronarography and 317 were PTCA, the latter including 122 PTCA alone and 195 ad hoc procedures respectively. All examinations were performed by 60 cardiologists with a wide degree of contributions: 14 physicians performed at least 20 and 41 of them performed less than 10 procedures. Consequently the number of examinations by centre varied from 15 (four centres under 20) to 95.
Three-fourths (74%) of the patients were male, their mean age was 65 years (female 26%, mean age 70 years); 55% of them showed at least one significant lesion, with more than 50% of arterial stenosis, multivessel diseases were diagnosed in 34.7% of patients.
Vascular access varied between centres, radial access ranging from 0 to 94% of all procedures in one given centre, with an overall mean value of 51%. No systematic difference was observed between values for CA or PTCA (radial access in 52% and 50% of procedures respectively). A ventriculography was associated to a CA procedure in 34% of the cases.
Table 1 shows DRL values obtained for the two categories of procedures considered, and for the three dosimetric indicators: DAP, fluoroscopy time and number of frames.
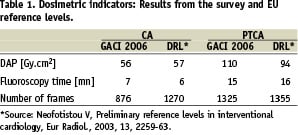
The provisional European DRL reference values are given in the same table.
Table 2 provides, for each examination category, statistics describing the dispersion of values gathered from the survey.
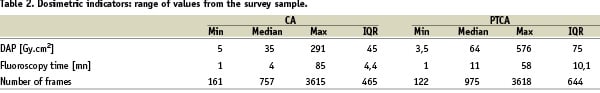
Four indices are given for each dosimetric indicator: the minimum, the median, the maximum values and the interquartile range (IQR).
From the radiation protection point-of-view, one may first notice the high values of DAP for PTCA, peaking at 576 Gy.cm2: six DAP values from four centres were found to exceed the 300 Gy.cm2 value, a trigger level that is commonly considered6,7 as likely to lead to possible skin damage.
However, these differences have to be cautiously regarded considering the inherent uncertainty in DAP values from this multicentre survey, although variations in one given centre are not affected by this precaution.
More generally, all indicators exhibit broad ranges of variation, particularly in therapeutic versus diagnostic procedures: maximum to minimum ratios range from 60 to 160 for the DAP, from 60 to 80 for the fluoroscopy time and from 25 to 30 for the number of images for CA and PTCA respectively. Looking at the IQR values obtained, the number of images show a lower degree of dispersion comparatively to the other two dosimetric indicators – the IQR value being significantly lower than the corresponding median value. Conversely the IQR values associated with the DAP and fluoroscopy time are of the same order, or even greater than the assessed median values.
An illustration of such a dispersion is given in the following graphs where data are grouped according to the corresponding interventional cardiology centre.
In each related parameter graph, all the centres are ranked in ascending order as a function of their mean value. Only 18 CL, instead of 19, are represented in the PTCA graphs since one specific CL included in the survey did not provide any PTCA procedures.
Each horizontal bar shows minimum, mean and maximum values and allows a comparison with the DRL value to be made. An anonymous inter-centre comparison is also made possible by the graphs through an arrow pointing to the position of a given centre called “your centre” among the others.
One can notice that the rank of “your centre” is changing according to the parameter considered and illustrates how difficult it can be to achieve the “optimum” rank order for all dosimetric indicators at once.
The six graphs above (Figure 2) show broad differences between centres: mean values of each parameter are in a ratio of 1 to 3 (number of images), 1 to 4 (fluoroscopy time), 1 to 5 or more (DAP), going from the lowest to the highest mean values.
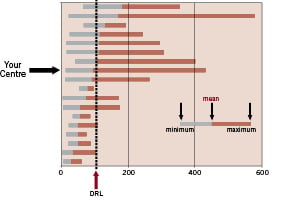
Figure 2(a). Distribution of DAP [Gy.cm2] (PTCA) (GACI Survey 2006)
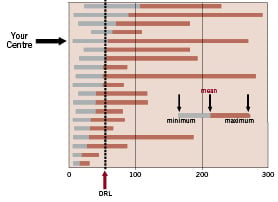
Figure 2(b). Distribution of DAP [Gy.cm2] (CA) (GACI Survey 2006)
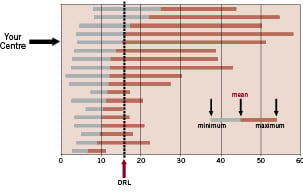
Figure 2(c). Distribution of fluoroscopy time [mn] (PTCA) (GACI Survey 2006)
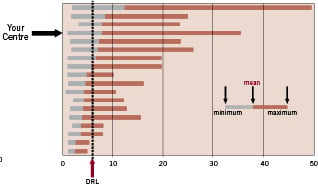
Figure 2(d). Distribution of fluoroscopy time [mn] (CA) (GACI Survey 2006)
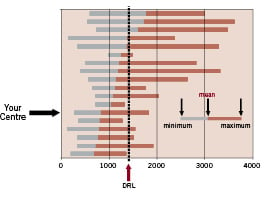
Figure 2(e). Distribution of the number of frames (PTCA) (GACI Survey 2006)
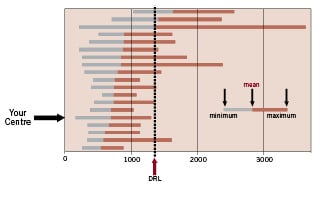
Figure 2(f). Distribution of the number of frames (CA) (GACI Survey 2006)
Furthermore, regardless of the type of parameter and procedure, the number of centres exceeding the DRL value markedly vary: from two (number of frames for CA), to seven (the DAP value for CA) thus evoking, from the radiation protection point-of-view, a clear need for further investigations of the corresponding interventional cardiology practices.
Although not in the scope of this survey, a further analysis of the relationship between a few “patient variables” and dosimetric parameters was tempted to correlate the latter with the severity of lesions (Table 3) in diagnostic as well as in PTCA procedures.
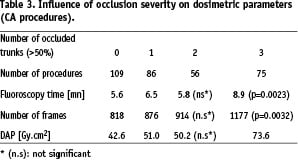
Table 3 clearly illustrates a consistent increase of the dosimetric parameters in CA procedures along with the severity of diagnosed lesions as expressed by the number of trunks with at least 50% of stenosis: the higher the number of lesions, the more important the dosimetric indicator value (p=0.0023 and p=0,0032 for the fluoroscopy time and the frame number from 1 to 3 occluded trunks respectively).
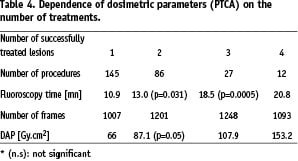
As for PTCA procedures, Table 4 shows the same general trend: the higher the number of treated lesions, the more important the dosimetric parameters value (p=0.031 and p=0.0005 for the fluoroscopy time from one to two and three treated lesions respectively; p=0.05 for DAP from one to two lesions treated).
Discussion
The results of the three dosimetric indicators (DAP, fluoroscopy time and number of frames) appear to reasonably comply with the reference levels first assessed in the EU7, with even better results as regards the number of frames (Table 1). A plausible cause of the latter finding may be the fact that a non negligible fraction (30%) of CA were carried out without ventriculography, together with the generalised use of lower frame rates (12.5 frames/s for cine run and 7 pulses/s combined with high X-ray beam filtration for fluoroscopy) made available in up-to-date equipment.
In spite of their overall compliance with international DRL values, all dosimetric indicators show larger variations, especially for PTCA comparatively to CA.
These wide ranges of variations demonstrate that global results do not entirely reflect the extreme values that may be correlated with high patient exposures.
In fact, three major factors which are always interacting in every interventional cardiac procedure must be considered:
– patient characteristics (weight, vascular access anatomy, habitus and status of coronary lesions),
– equipment settings (particular layout and availability of dose reduction options, e.g. low frame rate, adaptive dose rate filters or low dose fluoroscopy, ergonomy of equipment),
– operator practice or “profile” (absence of standardised protocols to follow, openness to adopt dose reduction options, together with his (or her) experience, level of training in intervention cardiology, as well as in the field of radiation protection).
As shown on the six graphs in the Figure 2, observed variations were due to combined influences of these three factors.
a) Influence of patient
When looking at the patient volume alone and considering the mechanisms that the automatic brightness control system should be doing to provide the user with a consistent level of image quality, several physical parameters (kV, mA, beam filtration, wedge filter) automatically and concomitantly interfere, leading to significant modifications of dose-rate from the X-ray tube, hence the expected larger dosimetric indicator values.
Although often mentioned as a patient dose related factor the Body Mass Index (BMI) of the population studied in this survey did not show any statistical significant correlation with the dosimetric indicators considered18.
Furthermore, if one adds to that, the complexity of therapeutic procedures (tortuosity of vessels, presence of calcification, bifurcation, occluded arteries) that cardiologists may be facing, dosimetric indicators can show a wide range of variations: complex situations such as PTCA may thus require prolonged fluoroscopy times without necessarily involving a proportionate increase of acquired images, hence the lower spread of values than in the case of CA (see Figures 2a to 2f).
As illustrated in Tables 3 and 4, the complexity of procedures, even at the diagnostic level, induces a higher degree of exposure through a rather systematic increase of dosimetric indicator values, the fluoroscopy time being the most sensitive parameter in the case of PTCA (increasing factor of 2.5 between one to three lesions to be treated).
Longer fluoroscopy times were also registered for CA using the radial access route compared to femoral access route 7.9 minutes against 6.3 minutes respectively. Although frequently mentioned8 as a meaningful factor influencing patient dose, the observed differences were not found as statistically significant in this survey (p=0,147 according to Mann-Whitney U-Test).
b) Influence of equipment
Equipment-related factors continually evolve according to equipment design and include equipment features and selectable operational modes that provide control over X-ray dose rates. Ideally, the operating physician must know the location and function of these controls and employ them as needed to assure minimal patient and personnel exposure. However intrinsic differences in terms of dose rates have been reported among different equipment models due to service engineers settings sometimes customised to the particular preferences of interventionists, thus suggesting unexpected increasing of dose levels according to the evolution of the technology (flat panel detector versus Image Intensifier system)9-12. However, when comparing these imaging detection technologies in terms of dose by keeping everything equal (field size, patient thickness, acquisition modality, radiographic projection), the reported resulting variations are within a range of 20 to 50%, a much smaller factor than that found in the survey in terms of interventional cardiology practices. As a very rough assertion, and taking into account that the evaluation of equipment performances was not the aim of the survey, the major factor to be explored seems therefore the way of the equipment is used rather than its intrinsic way of functioning.
c) Influence of operator
Knowing that variations among catheterisation laboratories, and more specifically between individual operators, have often been reported in the literature13,14, a tentative analysis of “operator effect” was made according to the following assumption: both fluoroscopy time and number of images reflect essentially/primarily the decisions of the practitioner faced with a given patient, whereas the DAP can be viewed as a translation by the equipment of the combined characteristics of patient (habitus, case complexity, etc) and operator behaviour.
Within this framework, two categories of cardiologists who participated in the survey were considered separately: those who previously had been trained in radiation protection and those who did not follow such a training course. They will be hereafter called “trained” and “untrained” operators.
In order to minimise the “patient effect”, only those operators who had performed at least 10 procedures of a given type were considered for the analysis. This led to include 310 CA out of 496, and 104 PTCA out of 317 respectively. The corresponding patient BMI mean values were 27 and 28 thus indicating the absence of any particular bias in such a reduction of the patient sample size.
The two following scatter diagrams (Figure 3) show the difference between the examinations carried out by the two categories of operators in terms of number images and fluoroscopy time for the CA and PTCA respectively.
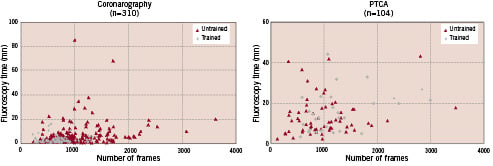
Figure 3. Comparison of dose related parameters between trained and untrained practitioners.
As shown, there are clearly two differently scattered distributions of values depending on the procedure type considered. As for the CA, the differentiation among the operators namely “trained” and “untrained” is distinctly identifiable: almost all the examinations performed by the “trained” operators are grouped together and close to the origin of the axis, thus representing rather “optimised” CA characterised by shorter fluoroscopy time and lower number of images (trained operators mean values: 3.3 minutes and 675 images – untrained operators mean values: 7.3 minutes and 979 images). Conversely, the CA performed by the “untrained” operators are scattered all around the graph.
Concerning the PTCA graph, one cannot, as in the previous case, clearly separate the two groups of examinations; “trained” or “untrained” operators being undifferentiated (trained operators mean values: 5.5 minutes and 799 images – untrained operators mean values: 7.6 minutes and 724 images).
Operator behaviour combined with training in radiation protection seems to have more impact on the two influencing patient dose parameters (fluoroscopy time and number of images) when solely looking at diagnostic procedures rather than at PTCA (Figure 3).
Indeed, as currently found, DAP values in coronarography are predominantly due to cine runs rather than fluoroscopy, therefore significantly reducing the number of images and limiting the use of fluoroscopy, as advised during the training, would tangibly result in an optimised procedure without any impairment of the final outcome.
In the case of PTCA, the relative contribution of fluoroscopy to the total DAP value is generally higher and consequently a cardiologist must carefully take into account the basic radiation protection rules: beam collimation, use of low dose rate modality (2 or 3 fluoroscopy modes are often available), limited use of magnification. Furthermore, it should be remembered that during such procedures the use of radiation protection devices is made more difficult since the operator is manipulating wires and/or balloon catheters while fluoroscopically viewing the patient. To be able to achieve an optimised procedure would therefore result in a benefit for both patient and cardiologist at the same time.
Conclusion
The dosimetric survey carried out by the GACI, allows us to estimate, for the first time in France, DRL values in interventional cardiology. Although provisional, since it is based on a small sample of interventional cardiology centres, these DRLs compared rather well with those already published in this field, with the exception of the DAP value for PTCA procedures. The maximum DAP values found in few cardiology centres exceeded the “critical” reference value of 300 Gy.cm2 thus evoking a potential risk of severe skin injury for the patients who underwent those procedures. It should be remembered as well that such maximum values are somehow related to an increase of the stochastic risk for the same patients expressed in terms of lethal cancer attributable to the ionising radiation exposure.
In order to practically implement the basic radiation protection principles (justification and optimisation for the patient on one hand, justification, limitation and optimisation for the staff on the other) a specific training for cardiologists is needed. According to a French government decree16 currently in force (published in the official journal of the French Republic, May 2004), all interventional cardiologists working in France are required to follow a training course on patient radiation protection by the end of 2009. This course will provide them with the essential notions of ionising radiation physics and patient dosimetry knowing that dosimetric results obtained so far tend to demonstrate that radiation protection training has already had an impact on the reduction of the highest dose values monitored during the survey.
Associated with such training there must be an evaluation of the equipment performance as well as an improvement of the radiation protection options.
As a general rule, cardiologists are not aware of dose levels and their relative variations occurring while carrying out fluroscopically guided procedures or acquiring radiographic images. Two components may be considered as contributing to this situation: a) the absence of relevant dosimetric indicators (DAP, fluoroscopy time, etc.) clearly displayed online at the level of each angiographic installation, b) a permanent quality control of the equipment providing baseline values against which actual DRL might be checked. A recent regulation put in place by the French government17 as a means of complying with European recommendations will help improve the current radiation protection practices, helping us respond in a consistent fashion to the ALARA requirement by continuous audits of equipment performance throughout the country.
Finally, regardless of the type of interventional cardiology procedure, strong variations in dose observed among the participating centres reflected the absence of harmonisation of technical protocols used thus clearly pointing out a need for promoting educative initiatives in relation to patient radiation protection.
Acknowledgements
The authors would like to express their gratitude to all physicians, radiographers and nurses of the following cardiology centres who actively participated in this survey.
Clinique Lafourcade, Bayonne; Nouvelles Cliniques Nantaises (NCN), Nantes; Polyclinique les Fleurs, Ollioules; Polyclinique Saint-Laurent, Rennes; Polyclinique de Courlancy, Reims; CHU Rangueil, Toulouse; CMC Parly 2, Le Chesnay; Hôpital Privé Antony, Antony; CHU Saint-Etienne, Saint-Etienne; Hôpital Henri-Duffaut, Avignon; CH Versailles, Hôpital André-Mignot, Le Chesnay; CH Haguenau, Haguenau; CHU Pitié Salpêtrière, Paris; CH Périgueux, Périgueux; Clinique Claude-Bernard, Metz; Institut Hospitalier Jacques-Cartier, Massy; Clinique Saint-Vincent, Besançon; CH Ambroise-Paré, Boulogne-Billancourt; Clinique Saint-Gatien, Tours