Abstract
Aims: Optical coherence tomography (OCT) is increasingly being applied to the coronary arteries. However, the risks associated with the imaging procedure are not yet well defined. The purpose of the present multicentre registry was to assess the acute complications associated with the clinical use of intra-coronary OCT in a large number of patients.
Methods and results: Consecutive patients from six centres who had OCT examination were retrospectively included. All adverse events and complications, even if transient, were noted. Risks were categorised into: 1) self-limiting 2) major complications including major adverse cardiac events (MACE) and 3) mechanical device failure. A total of 468 patients underwent OCT examination for evaluation of: plaque (40.0%), percutaneous coronary intervention (28.2%) or follow-up stent tissue coverage (31.8%). OCT was performed using a non-occlusive flush technique in 45.3% with a mean contrast volume of 36.6±9.4ml. Transient chest pain and QRS widening/ST-depression/elevation were observed in 47.6% and 45.5% respectively. Major complications included five (1.1%) cases of ventricular fibrillation due to balloon occlusion and/or deep guide catheter intubation, 3 (0.6%) cases of air embolism and one case of vessel dissection (0.2%). There were no cases of coronary spasm or MACE during or within the 24 hour period following OCT examination.
Conclusions: OCT is a specialised technique with a relatively steep learning curve. Major complications are uncommon and can be minimised with careful procedural planning and having an awareness of the potential contributory risks, especially deep guide catheter intubation during contrast flushing. Upcoming developments will make OCT more practical and less procedurally demanding, also potentially conserving contrast volume considerably.
Introduction
Optical coherence tomography (OCT) is an intracoronary imaging technique using near infrared light with a much higher spatial resolution than intravascular ultrasound (IVUS). The 15 micron resolution permits detailed characterisation of the vessel wall giving new insights into the in vivo characterisation of atherosclerotic plaque and tissue responses following stent implantation. Unlike IVUS however, the technique requires flushing of the coronary artery to allow light transmission with the first generation OCT system also mandating proximal vessel balloon occlusion. Whilst the imaging resolution benefits of OCT are clear, the need for a flush system increases the complexity of the technique, and the risks associated with this have not been evaluated. The purpose of the present multicentre registry was, for the first time, to assess the acute complications associated with the clinical use of intracoronary OCT in a large number of patients.
Methods
Study population and OCT procedure
We conducted a multicentre registry to evaluate the safety of OCT. Data from patients undergoing OCT examination in six centres were reviewed. Consecutive patients who had OCT examination performed before January 31, 2008 were retrospectively included. Weight adjusted heparin was administered as standard prior to OCT imaging. All OCT examinations were carried out using a dedicated optical wire (ImageWire, LightLab Imaging Inc., Westford, MA, USA) connected to either the M2 or M3 OCT console (LightLab Imaging Inc., Westford, MA, USA). All participating centres completed the demographic, clinical and procedural case information using a uniform data sheet that was centrally analysed. The indications to perform OCT were categorised into evaluation of: A), lesion/plaque; B), percutaneous coronary intervention PCI) (stent apposition); or C), stent tissue coverage at follow-up. The number of vessels imaged, together with the OCT flushing strategy (with or without proximal vessel balloon occlusion, see below) were recorded. OCT exclusion criteria applied by operators/centres included impaired left ventricular ejection fraction (<30%), renal impairment (serum creatinine >1.5 mg/dL), single remaining or tortuous vessel. When the non-occlusive technique was used, the additional contrast load required to permit imaging in a blood-free environment was documented.
Flush strategy
Infra-red light is unable to penetrate blood, thus imaging must be accompanied by transient clearance of the field of view from blood. In clinical intracoronary OCT, two methods have been established: 1), using a proximal occlusion balloon with flushing of crystalloid solution through the end hole of the balloon catheter using a power injector or 2), a non-occlusive approach with contrast flush injection via the guiding catheter.1
Balloon occlusion method
A low-pressure, short over-the-wire balloon (Helios, Goodman Inc, Nagoya, Japan) with large inner lumen is advanced over a conventional guidewire distal to the region of interest. The guidewire is then replaced with the dedicated OCT imaging wire and the balloon catheter is positioned in the proximal part of the vessel. Inflation of the balloon is performed using a dedicated indeflator to 0.5-0.7 atm during which coronary blood flow is replaced by continuous infusion of Ringer’s lactate or physiological saline at a rate of 0.5-1.2 ml/sec using a power injector (e.g. Mark-V ProVis, Medrad, Inc. Indianola, PA, USA).1-3 A motorised pullback of the image wire is then commenced at a rate of 1.0 mm/sec to acquire images.
Non-occlusive technique
As the handling of the OCT image wire is limited by the fact that it contains an optical fibre and is not comparable to a standard guidewire with respect to steerability, pushability and torqueability, its safe passage distal to the region of interest can be facilitated by use of an over-the-wire catheter (e.g., the single lumen Transit, Cordis, Johnson & Johnson, Miami, FL, USA or the double lumen 0.023” TwinPass, Vascular Solutions Inc, Minneapolis, Minnesota, USA). The automated pullback (at 3.0 mm/sec) is then commenced during simultaneous flushing of viscous iso-osmolar contrast (e.g. Iodixanol 320, Visipaque™, GE Health Care, Cork, Ireland) through the guiding catheter. This can be achieved either manually or by use of an automated power injector (e.g. Mark-V ProVis, Medrad, Inc. Indianola, PA, USA).1-3
OCT risks
Any complication judged by the operators to have occurred during or within the immediate 24-hour period following OCT examination was included, even if transient and with no clinical sequelae.
Risks were categorised into:
1) Self-limiting events
2) Major complications (arrhythmia, embolisation, coronary dissection or spasm) including major adverse cardiac events (defined as MI, emergency revascularisation – including percutaneous or surgical – and death).
3) Mechanical device failure
Furthermore, all risks were classified based on their eventual outcome as: A), Immediate correction with no specific action required; B), transient, but requiring specific treatment with resolution before the patient left the catheterisation laboratory; or C), required treatment/surveillance following discharge from the catheterisation laboratory (including lengthening patient’s hospitalisation).
Study centres
The six participating centres were located in the Netherlands (one centre), United Kingdom (two centres), Italy (one centre), Germany (two centres). The number of OCT studies contributed by each centre was: Thoraxcenter (Rotterdam, the Netherlands n= 162, 34.6%); Royal Brompton Hospital (London, United Kingdom, n=91 19.4%); St. Giovanni Hospital (Italy, n=85, 18.2%); Helios Heart Centre (Siegburg, Germany, n=64, 13.7%). Medizinische Poliklinik, University of Munich (Munich, Germany, n=36, 7.7%) and Harefield Hospital (Middlesex, United Kingdom, n=30, 6.4%).
Statistical analysis
Descriptive analyses were used. Results are quoted as percentages for categorical data or as mean ± standard deviation for continuous variables. Continuous and categorical variables were compared with the t-test and the chi-square/Fisher’s exact test as appropriate. A p value of <0.05 was considered significant.
Results
Baseline clinical and procedural characteristics
A total number of 468 OCT examinations were recorded between June 2004–November 2007. Table 1 shows the baseline clinical and procedural characteristics.
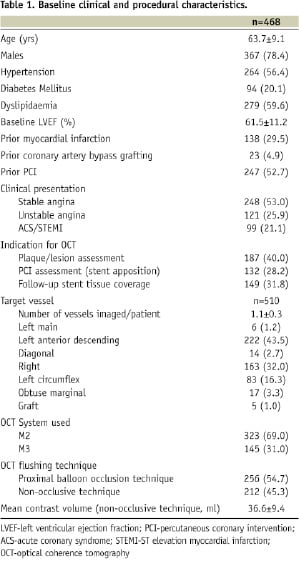
OCT was performed for plaque/lesion evaluation in 187 (40.0%), PCI evaluation in 132 (28.2%) and for the assessment of stent tissue coverage at follow-up in 149 (31.8%) of patients. A total of 510 vessels were imaged (1.1±0.3/patient). The LAD and RCA were the most frequently imaged vessels. A small proportion of patients had OCT imaging of the left main coronary artery (1.2%) and a bypass graft (1.0%).
Of the 468 patients, 256 (54.7%) had images acquired during proximal balloon occlusion while the remaining 212 (45.3%) had OCT using a non-occlusive technique. In these patients, the additional mean contrast load used for flushing during OCT imaging was 36.6±9.4ml.
Risks of OCT
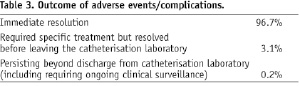
All observed complications are summarised in Table 2. The eventual outcome of the adverse events and complications encountered is depicted in Table 3.

1) Self-limiting events
As expected, the most frequent observation was transient chest pain during OCT image acquisition (47.6%). In all cases this settled following cessation of imaging and was significantly more frequent in patients imaged using the occlusive compared to non-occlusive technique (69.9% vs. 20.8%, p<0.001). In association, transient electrocardiographic changes were also observed with widening of the QRS complex or ST-segment depression in 41.0% and ST-elevation in 4.5%, almost exclusively in those imaged using proximal vessel balloon occlusion. Sinus brady and tachycardia was infrequently observed and settled promptly following cessation of imaging. There were two (0.4%) cases of transient atrioventricular block that spontaneously resolved following deflation of the proximal occlusion balloon and withdrawal of the catheter.
2) Major complications
Ventricular fibrillation
Ventricular fibrillation (VF) occurred in five (1.1%) patients. In all cases, sinus rhythm was promptly restored following cessation of OCT imaging and external defibrillation. Three of the five cases occurred during proximal balloon occlusion. The two cases seen with the non-occlusive technique were in the context of deep guide catheter intubation of the left coronary artery during simultaneous contrast injection.
Air embolism
There were three (0.6%) cases of air embolisation. In one case, this occurred early on in the procedure, when introducing the guiding catheter specifically with the intention to perform OCT. Two other cases occurred during flushing of the crystalloid solution with air inadvertently introduced during connection of the flush lines. All cases responded promptly to air aspiration, treatment with nitrates and in one case, nitroprusside administration.
Coronary dissection
A minor type-A coronary dissection was observed in one (0.4%) patient as a result of the imaging wire. Coronary blood flow was not impaired and further treatment was not indicated.
Coronary spasm
There were no cases of coronary spasm observed during OCT imaging.
MACE
There were no MACE observed during or in the 24 hour period following OCT imaging. In one patient, stenosis was observed at the site of previous balloon occlusion four months following OCT evaluation of the LCx. Due to the presence of multivessel coronary disease with angina, the patient was referred for CABG.
3) Mechanical device failure
Although there was no adverse clinical outcome observed, in one (0.2%) patient having OCT nine months following stent implantation, the imaging wire became entrapped amongst stent struts in the LAD with subsequent fracture at the distal tip. In this case, an over-the-wire catheter was initially used to advance the wire distally however, once positioned, was found to be too proximal and within the stent. Attempts to advance the wire forward resulted in wire entrapment. Four month follow-up was uneventful with control angiography showing patent vessel without flow abnormalities.
Discussion
This is the first registry to demonstrate the acute risks related to OCT imaging in a large number of patients. The high-resolution, together with advantages over other imaging modalities such as IVUS, have made OCT very popular for the detailed assessment of atherosclerotic plaque and coronary stents. As a result, this study provides essential safety information that will see OCT performed in a more informed manner, both for operators and patients alike.
Several groups have reported their clinical experience with OCT over the last few years.2-11 Nevertheless, only limited information about acute complications of this procedure is available. Recently, Yamaguchi et al12 examined the feasibility of OCT and IVUS imaging in 76 patients. Although transient chest pain and electrocardiographic changes caused by imaging were not considered as part of their study, there were no adverse events reported following both IVUS and OCT, with the latter being performed exclusively using the occlusive method. In contrast, the present study included a large number of consecutive patients undergoing OCT examination, and recorded all potential adverse events, even if transient and benign. We believe this permits a more informed assessment and is therefore representative of the ‘real world’ application and safety of OCT imaging.
The present study also assessed patients having OCT imaging using the non-occlusive technique that will, because of its simpler procedural requirements, become the mainstay method for OCT image acquisition, eliminating the cumbersome proximal balloon occlusion requirements. Such developments will be realised in the not too distant future, with the introduction into clinical practice of faster image acquisition speeds thanks to optical frequency-domain technologies.13 Therefore, the expected rise in OCT use is another reason why comprehensively reporting the safety profile of the technique remains of paramount clinical importance.
The spectrum of adverse events observed in relation to OCT imaging in our study was broad. The majority of events recorded were minor and transient, with chest pain being the most frequent. This is not surprising as, in a significant proportion of patients (54.7%), images were obtained during proximal balloon vessel occlusion. In all cases, the chest pain resolved following cessation of imaging or deflation of the occlusion balloon. The mechanisms purporting to link balloon coronary occlusion and chest pain are complex and include the triggering of several neural responses stimulating coronary mechanoceptors and vagal/sympathetic cardiac afferent fibres.14,15
Electrocardiographic changes were observed in almost half the patients. Such changes are also frequently observed during angioplasty and stent implantation and are likely reflective of underlying ischaemia. In addition to ST-segment changes, transient prolongation of the QRS interval was seen. Although this study was not designed to measure the QRS interval, prolongation was judged visually during OCT imaging. This remains a highly sensitive marker of ischaemia during percutaneous coronary intervention (PCI), even more so than ST-segment changes and chest pain which is highly subjective.16 Furthermore, coronary occlusion, particularly of proximal or middle artery segments is directly linked to observations of QRS prolongation.16 The knowledge that almost half of all patients are likely to experience some level of chest discomfort and/or electrocardiographic changes of ischaemia during OCT imaging should serve to inform patients prior to the procedure and, where indicated, encourage the use of pre-medication, such as short acting analgesics.
The frequency of arrhythmias observed, particularly life-threatening VF that occurred in five (1.1%) of patients, warrants further analysis. Several studies have shown the incidence of VF during coronary angioplasty is about 1.5%,17,18 with the rate dropping down to around 0.6% for diagnostic procedures.19,20 In addition to ischaemia, other mechanisms have also been identified including reperfusion, electrolyte imbalances, coronary instrumentation, osmolarity and electrolyte composition of contrast agents and intra-coronary thrombus.21-27
Iodixanol (Visipaque™, GE Health Care, Cork, Ireland) is the contrast agent that is preferentially used for flushing during the non-occlusive method. The advantage lies in its higher viscosity relative to other agents, which permits optimal blood clearance for OCT imaging at the given flush volumes through the guiding catheter. This agent has also been shown to have a lower propensity to cause VF given its lower osmolality, higher viscosity and higher concentration of sodium and calcium chloride molecules compared to other non-ionic media.28-31
In the two cases in which VF occurred during contrast flush, the operators reported deeply intubating the guide into the left coronary artery in an attempt to optimally deliver the contrast flush. In hindsight, this is thought to potentiate the risk of VF with prior reports showing that the combination of a wedged catheter and contrast flush is a high-risk situation for inducing VF.25,32,33 Given that VF also occurred in the patients during the occlusive technique with flush of crystalloid solution and, therefore no contrast, it is obvious that other mechanisms are at play, with ischaemia still a major contributor. Nevertheless, reporting of such events encourages further work in developing alternative, non-contrast based flushing solutions that are bio-compatible while eliminating the potential unwanted effects of contrast agents.
In our experience, the additional contrast volume used for flushing does not translate into adverse nephrotoxic events. However, patients with renal impairment are not subjected to OCT imaging. In such patients, an occlusive technique could be used however acknowledging its inherent limitations such as an inability to visualise ostial or very proximal coronary segments. Refinements in OCT technology with optical frequency domain imaging (OFDI) permit pullback speeds up to 20 mm/sec hence, a single pullback could be accomplished within a matter of a few seconds thereby dramatically reducing the contrast volume needed.13
Other complications, such as dissection and air embolisation are not specific to OCT and can be observed at any stage of an invasive procedure. Recently Kim et al34 reported a single case of thrombus formation during elective OCT interrogation of LAD stents at seven months follow-up. Although this is a potential complication with any arterial instrumentation, we did not observe any such cases in our cohort of patients, all treated with weight adjusted heparin prior to OCT assessment.
Compared to IVUS, the present study did not identify cases of vessel spasm with dissection seen in one patient and device related failure in one patient. Prior IVUS studies found an incidence of 3% of coronary spasm, in some, also resulting in abrupt vessel occlusion.35 This was irrespective of the size of the IVUS catheter used.35 Technical failure of the IVUS system was observed in 0.4% including guide wire winding or breakage of the catheter.35 Such complications are fortunately uncommon, but are inherent with invasive procedures requiring intracoronary catheter manipulation and instrumentation.
The incidence of complications encountered in relation to the OCT procedure is consistent with safety data from coronary angioscopy. Similarly, angioscopy requires balloon occlusion during image acquisition although balloon-related vessel injury has not been shown to be a problem six months following angioscopic examination.36 The general trend for OCT image acquisition is to eliminate this aspect, thereby simplifying the procedure considerably.
Angioscopic technology has also remained rather stagnant over the years, causing it to be used only by a select few specialised centres worldwide. In contrast, OCT has rapidly evolved from the initial use of angioplasty balloons and catheters to dedicated, low profile materials, all contributing to a safer procedure. Further, OCT permits the accurate quantification of both plaque and tissue strut coverage and is also compatible with 6 Fr guiding catheters.
Limitations
This study was a retrospective analysis, however included a large number of consecutive patients undergoing OCT at different centres. Also, as OCT is a relative ‘new comer’ to the field of intravascular imaging, cases from the early phase of OCT technology development were included in this study meaning that complication rates were also inclusive of this early experience and might reflect to a certain degree the learning curve of the technique. Nevertheless, to allow an informed assessment about the safety profile, all potential adverse events were included, even if transient and benign.
Conclusions
OCT technology has moved at a rapid pace with greater refinements in materials and technique already contributing to increased clinical uptake. Future developments such as optical frequency domain imaging will see OCT use simplified and therefore become conducive to more centres and operators worldwide. Nevertheless, OCT is a specialised technique with a relatively steep learning curve and therefore, requires adequate proctorship. Major complications are uncommon and can be minimised with careful procedural planning and being aware of the potential contributory risks, especially deep guide catheter intubation during contrast flushing and minimising the duration of image acquisition in preference for more frequent but shorter imaging runs. Developments will also make OCT more practical and less procedurally demanding, also potentially conserving contrast volume considerably. The benefits in relation to a greater understanding of coronary artery disease and responses following stent implantation are enormous, meaning that light-based imaging will continue to develop well beyond the Acknowledgements Jurgen Lighthart, Francesca Del Furia, and Philip Moore who provided valuable assistance with data collection. The study was supported in part by Siemens Healthcare.

