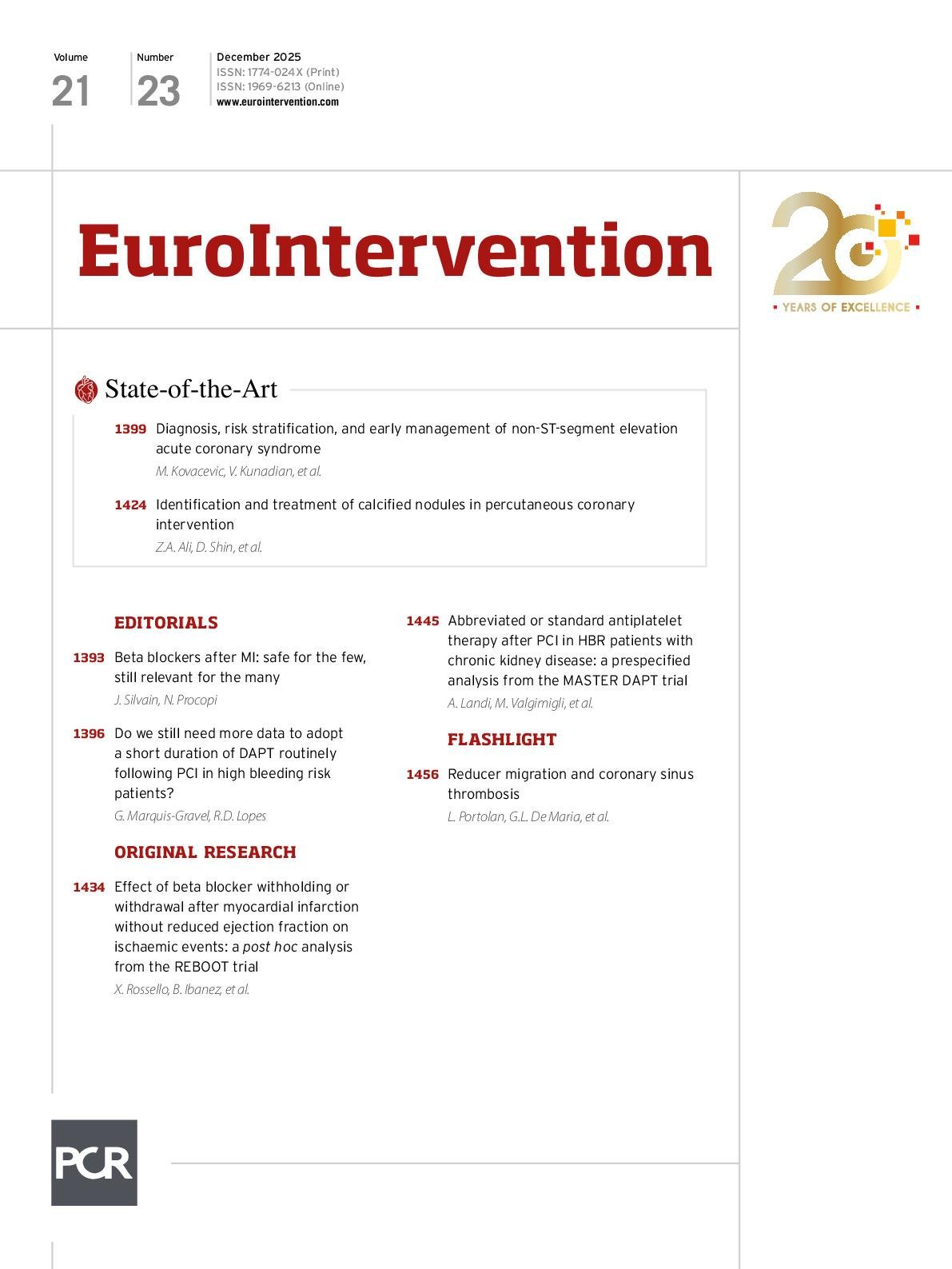
As we arrive near the end of 2025, we offer you the chance to update your knowledge with not one, but two state-of-the-art reviews, as well as the latest research in beta blockers and dual antiplatelet therapy.
Management of NSTE-ACS
Mila Kovacevic, Vijay Kunadian and colleagues present a comprehensive state-of-the-art review of current evidence-based strategies for managing patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). The authors discuss recent advances in diagnostic tools, risk stratification, and the timing and choice of treatment strategies and then delve into the management of specific subsets of patients, including those with multivessel disease, the elderly, and females.
Calcified nodules and PCI
The challenge of treating calcified nodules (CNs) with percutaneous coronary intervention (PCI) is the subject of our second state-of-the-art. Ziad A. Ali, Doosup Shin and colleagues discuss the identification and classification of CNs and their distinct subtypes, as well as the treatment strategies that are currently available to the interventional cardiologist.
Beta blockers after MI
In a post hoc analysis of the REBOOT trial, Xavier Rossello, Borja Ibáñez and colleagues evaluate the short-term ischaemic safety of withdrawing or withholding beta blockers after discharge in patients with myocardial infarction (MI) and a left ventricular ejection fraction >40%. Their finding – that neither withdrawal nor withholding beta blockers increased the incidence of short-term or recurrent ischaemic events in this patient population – has contributed to the recent lively discussion on beta blockers. Johanne Silvain and Niki Procopi contribute an accompanying editorial.
Abbreviated antiplatelet therapy in HBR patients with CKD
Antonio Landi, Marco Valgimigli and colleagues compare the efficacy of 1-month to ≥3-month dual antiplatelet therapy (DAPT) in high bleeding risk (HBR) patients with chronic kidney disease (CKD) undergoing PCI. In this prespecified analysis of the MASTER DAPT trial, the abbreviated DAPT duration was associated with similar rates of net adverse clinical events and major adverse cardiac or cerebral events and reduced bleeding – regardless of renal function. Guillaume Marquis-Gravel and Renato D. Lopes discuss the results in an accompanying editorial.