In the European Council Directive 97/43 EURATOM on health protection of individual against the dangers of ionising radiation in relation to medical exposure1 interventional procedures are considered as a “special practice” involving high radiation doses to patients and requiring quality assurance programmes including patient dose evaluations. Practitioners performing such procedures shall obtain appropriate training in radiation protection (RP) under the responsibility of the Member States of the European Union (EU). The Directive mentions that the use of diagnostic reference levels (DRL) shall be promoted, and that Member States shall ensure that appropriate local reviews are undertaken whenever DRLs are consistently exceeded and that corrective actions are taken where appropriate.
Staff working with ionising radiation are under the jurisdiction of specific national regulations coming out of the Council Directive 96/29/EURATOM2, requiring strict annual limits of doses, which do not apply to patients.
The medical purpose of the procedure is considered a priority, and practitioners are expected to have enough knowledge of RP to avoid giving unnecessary radiation doses to the patients.
DRLs are values that represent the state of practice and are only applicable to a sample of patients. In practice, the values are selected on the basis of a percentile point based on the observed distribution of doses to patients. The International Commission on Radiological Protection (ICRP) has introduced this concept in 1996 to help with the optimisation of medical exposures. In medical imaging, these values help indicate whether, in routine conditions, the levels of a patient’s dose are unusually high or low for a specified imaging procedure. If so, a local review should be initiated to determine whether protection has been adequately optimised or whether corrective action is required. The values should be selected by professional medical bodies in conjunction with national health and radiological protection authorities and reviewed at intervals that represent a compromise between the necessary stability and the long-term changes in the observed dose distributions3.
In the beginning, DRL were only used for simple diagnostic examinations, but a significant effort has been made over the last years to extend this concept to interventional procedures and especially to cardiology. In 2003, a research consortium, supported by the European Commission, published a set of provisional DRL values for cardiology4. At the same time, the International Atomic Energy Agency (IAEA) launched an ambitious programme of RP in cardiology, including the preparation of a significant amount of training material5 and several research programmes dealing with the evaluation of patient doses as part of its International Action Plan on the radiological protection of patients. As a result, a pilot study involving hospitals from Europe, South America and United States, produced a second set of DRLs6 compatible with the previous European ones. Table 1 summarises the results obtained by the EU and the IAEA studies.
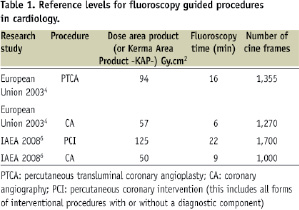
In both studies, the complexity of the procedures (that can be affected by the patient’s anatomy, and the location and severity of the treated pathology)7 could be considered “moderate” and it is suggested6 that an increase in the median values of patient doses up to a factor of 2 due to complexity could be acceptable. Appropriate scaling of reference levels by complexity provides an additional tool for refining a facility’s quality assurance and optimisation processes.
Thus, the tool to compare median dose values for a sample of cardiac procedures with DRL already exists on an international level and could be used to confirm the appropriate setting of the x-ray systems and the operational procedures if local values are consistently higher than the DRL.
The paper published by O. Bar, C. Maccia and co-workers in this issue of EuroIntervention is specially relevant, as it represents one of the first national surveys in Europe on this topic including a set of reference levels for France, confirming that the radiological risk for interventional cardiology in this country is similar to that evidenced in other international studies already published.
It should be highlighted that all the centres involved in the French survey have at least one cardiologist trained in RP. A similar study with medical specialists not trained in RP would probably give worse results. What the French experience demonstrates moreover is the possibility of using the results of these surveys to improve clinical practice while identifying the centres with high patient doses and suggesting corrective actions.
France along with some other European countries (but yet not all the members of the EU), has already started a programme to train (and certify) interventional cardiologists in RP as required by the European Directive1 and the corresponding European guidelines9. These guidelines, published after a consulting process with the member states of the EU and most of the European scientific societies suggests 20 to 30 hours of RP training for interventional cardiologists.
Finally, one must not forget to mention the relatively high level of exposure for staff working in interventional cardiology laboratories. Interventional cardiologists have an exposure per-head per year two to three times higher than radiologists. It appears quite feasible to reduce by a factor of ten these occupational doses simply by an intensive training program. Professional guidelines as well as European law stress the responsibility all physicians have to minimise the radiation injury hazard to their patients, to their professional staff and to themselves10.
Increasing cancer risk and undesirable side effects on staff should be taken into account to support training and optimisation programmes.
Lens doses may exceed the threshold for opacities or cataracts after several years of work, if RP tools are not properly used. The ICRP, in its last 2007 recommendations3 stated that new data are expected concerning the radio sensitivity of the eye and the ensuing visual impairment due to the likelihood of inherent risk, a particular emphasis on optimisation in situations of exposure of the eyes should thus be acknowledged.
The main source of staff exposure is the scatter radiation from the patient. Thus, if cardiologists are doing good management of their patient doses they will also improve their own occupational protection. The study published by O. Bar, C. Maccia and co-workers8 will help towards this goal: the good management of radiation doses in cardiology reducing unnecessary risks for patients and staff.