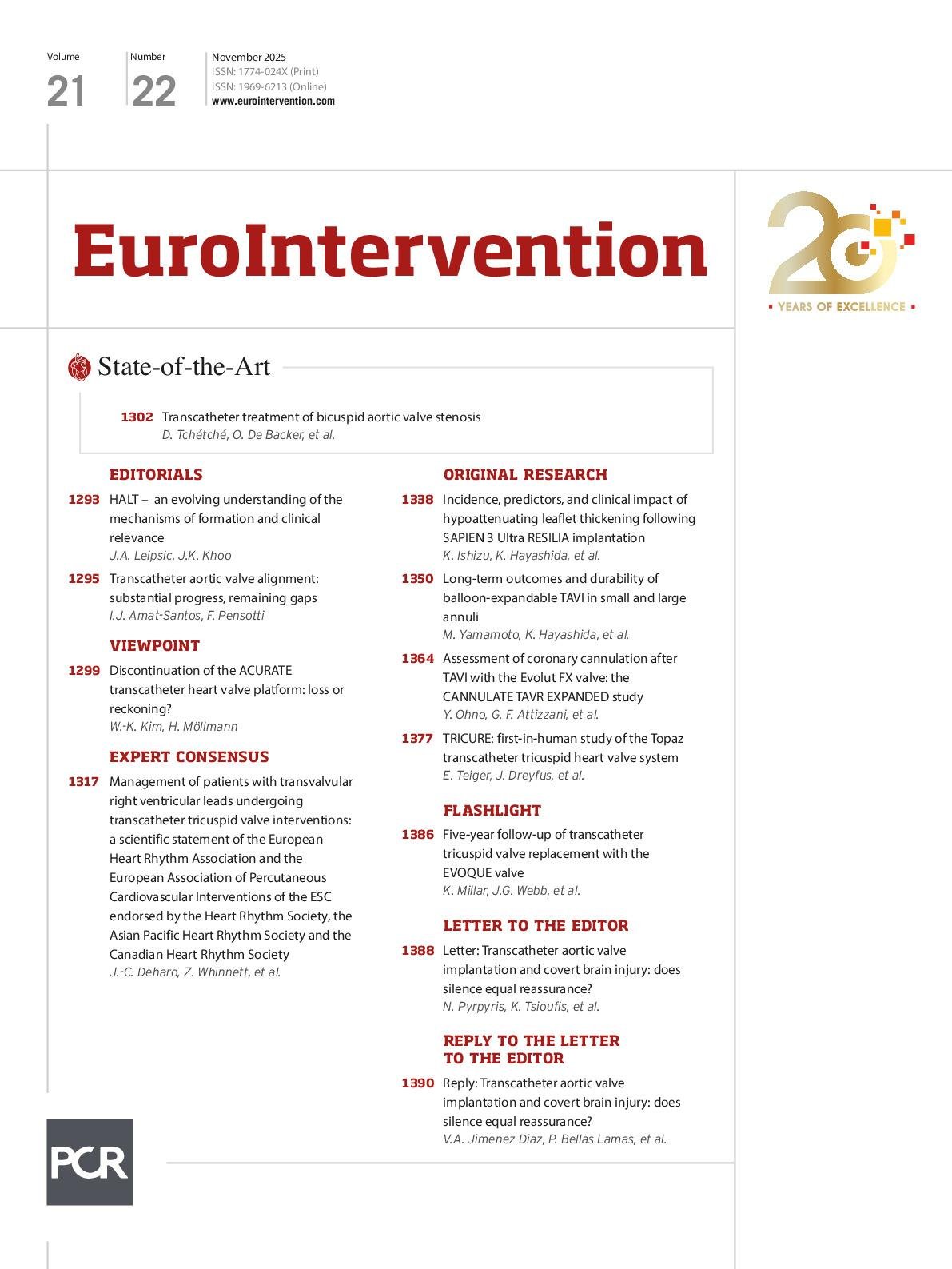
And here we are again in November, opening a new issue full of articles on interventions for valvular heart disease, coinciding with another sparkling edition of PCR London Valves. This issue is special for us, and the fact that it is one of only four printed issues is the clearest proof. Perhaps we are a bit romantic – and in the digital era our kind is probably becoming extinct – but seeing conference attendees holding the printed copy, as a gift, is a real satisfaction. I remember that, years ago, assembling this special issue was more complex. Given the nature of the conference, one would expect it to be full of articles on transcatheter aortic valve implantation (TAVI), mitral transcatheter edge-to-edge repair, and similar topics â and indeed, it always has been. However, filling an entire issue was not simple, especially in 2020, when most submissions were predominantly coronary-focused. At that time, we had to be resourceful, inviting renowned authors to contribute editorials, viewpoints, and reviews. Now, the challenge is the opposite: we are fortunate to receive an abundance of high-quality submissions – likely reflecting the Journal’s growth and rising impact factor. The task is no longer simply filling the issue, but selecting the most relevant articles, arranging them to ensure a coherent flow, and refining the production process to maximise both clarity and visual impact. Our aim is to attract trials, multicentre studies, and leading authors, always striving for excellence, even when the standard is already high. In keeping with this commitment, and to celebrate the Journal’s 20th anniversary, we are establishing a new tradition. For the first time, a prominent member of our cardiology community will receive the “Alain Cribier EuroIntervention” award. With the family Cribier’s endorsement, the award will be presented in a plenary session by Hélène Eltchaninoff, honouring the academic and clinical contributions of a man whose invention, talent, and charisma have reshaped the management of valvular heart disease. It is in this spirit of excellence and innovation that we present the current issue. Here, you will find a carefully curated selection of articles on TAVI and other interventions, each chosen to provide a comprehensive overview of the latest evidence, clinical insights, and emerging techniques. We hope this issue both informs and inspires, reflecting the dynamic progress in valvular heart disease management. Let’s turn to the articles: We begin this issue with a state-of-the-art review on the transcatheter treatment of bicuspid aortic valve (BAV) stenosis from Didier Tchétché, Ole De Backer and colleagues. TAVI has expanded to include selected patients with BAV anatomies, but challenges, both technical and procedural, remain. The authors review the classifications of BAV disease and the current procedural techniques; they discuss what research has been done to date and what knowledge gaps remain to be filled. In an expert consensus commissioned by the European Heart Rhythm Association and the European Association of Percutaneous Cardiovascular Interventions of the European Society of Cardiology, Jean-Claude Deharo, Zachary Whinnett and colleagues focus on the management of patients with transvalvular right ventricular leads undergoing transcatheter tricuspid valve interventions. Nearly one-third of patients referred for transcatheter tricuspid valve interventions have a pacemaker or implantable cardioverter-defibrillator lead, making communication between interventional cardiologists and electrophysiologists essential. This document relays the current scientific evidence available and is intended as a resource for Heart Teams in their decision-making and patient management. The timing and impact of the ACURATE neo2/Prime transcatheter heart valve’s (THV) discontinuation merit a nuanced discussion, according to Won-Keun Kim and Helge Möllmann. In this viewpoint, the authors discuss whether the platform’s discontinuation really is the scientific reckoning that some claim, or whether other elements, such as registry design, device sizing and use, led to an underestimation of the device’s potential. To begin our original reseach section, Kenichi Ishizu, Kentaro Hayashida and colleagues examine the 30-day clinical incidence, predictors, and impact of hypoattenuated leaflet thickening (HALT) after TAVI with the latest-generation SAPIEN 3 Ultra RESILIA. The overall rates of HALT were found to be comparable with the previous-generation devices and the device’s revised commissural leaflet suspension method that is specific to the smaller-sized valves was not found to be associated with an increased risk of HALT. However, the prosthesis deformation index and asymmetric leaflet expansion were independently associated with an increased risk of HALT, regardless of THV size. Jonathon A. Leipsic and John K. Khoo comment in an accompanying editorial. Our next original research articles asks whether a patient’s baseline aortic annulus size is a predictor of long-term outcomes after TAVI with a balloon-expandable THV. Masanori Yamamoto, Kentaro Hayashida and colleagues tackle this question by dividing a large cohort of patients who underwent TAVI up to 7 years earlier by annular size in order to evaluate primary endpoints of all-cause mortality and stages of bioprosthetic valve failure. As annular size was not found to be associated with a long-term prognosis or valve durability, the authors suggest that other indicators need to be explored. Then, we turn to whether optimal commissural and coronary alignment can be achieved using a tall-frame, supra-annular THV. Yohei Ohno, Guilherme F. Attizzani and colleagues evaluate the feasibility and timing of coronary cannulation post-TAVI with the new-generation Evolut FX device. The CANNULATE TAVR EXPANDED study had a 100% success rate in coronary cannulation of the left coronary artery and a 96.7% success rate for the right coronary artery. Misalignment was identified as a strong predictor for suboptimal coronary cannulation of both the left and right coronary arteries. In an accompanying editorial, Ignacio J. Amat-Santos and Filippo Pensotti discuss how these findings can help direct future research. In this issue’s final original research paper, Emmanuel Teiger, Julien Dreyfus and colleagues present the first-in-human TRICURE study which evaluated the safety and efficacy of the novel Topaz transcatheter tricuspid valve replacement system for the treatment of tricuspid regurgitation (TR). This dual-stent device, specifically designed for the tricuspid valve anatomy, was tested in 20 patients with outcomes including short procedure times, low complication rates, and substantial and sustained reduction of TR at 30 days. The authors include a case study of one patient at 6 months as well as a discussion about operator learning curves and screening criteria, in the hopes of paving the path for future studies. And now, to the articles themselves.
Intro editorial
DOI:
A State-of-the-Art on TAVI in biscuspid aortic stenosis; an expert consensus on transcatheter tricuspid valve interventions in patients with transvalvular right ventricular leads; the ACURATE platform discontinuation; coronary cannulation after transfemoral TAVI with the Evolut FX; HALT after TAVI with the SAPIEN Ultra RESILIA; impact of aortic annular size on long-term outcomes and valve durability; the TRICURE first-in-human study; 5-year follow-up of EVOQUE TTVR; and more
You need to subscribe to download this file
×
If you are not yet a subscriber, please subscribe to download this file.
Download citations
×
Select a format