Introduction
Optimal revascularization strategy in patients with coronary artery disease remains a subject of debate between interventional cardiologists and surgeons. Numerous large scale randomized trials addressed this issue comparing coronary artery bypass grafting (CABG) with percutaneous coronary intervention (PCI) in patients with multivessel disease (MVD). Initially these trials compared multivessel balloon angioplasty with CABG1-6 and in a later period multivessel stenting with CABG7-11. These studies clearly demonstrated that there was no difference between the two therapeutic modalities regarding mortality and non fatal myocardial infarction but patients treated with balloon angioplasty or stenting required more often repeat revascularization procedures related to restenosis12,13.
Clearly stenting reduced the gap in the event free survival rate between the two revascularization strategies from 32% in CABRI trial (91% versus 59% in favour of CABG) to 14% in ARTS I trial (89% versus 75%) but still surgery remained the gold standard for patients with MVD with an event free survival rate around 90%14.
Recently the drug eluting stents were introduced and proven to be very effective in reducing restenosis and the incidence of repeat revascularisation15-18. In the recently conducted ARTS II trial the sirolimus eluting stents were compared with historical CABG data from the ARTS I trial in patients with MVD. The incidence of major adverse cardiac events was comparable in both approaches, even though the number of vessels and lesions treated were higher than in the previous trials19. However, it has been argued that despite the fact that patients with two or three vessel disease have been included in the aforementioned trials, in the «real world» both interventional cardiologists and surgeons are often confronted with more complex anatomy. Numerous exclusion criteria and disagreement between the surgeons and the interventional cardiologists allowed only 2%-12% of the patients screened to be randomized13.
Another characteristic of these trials was the heterogeneity in the complexity of coronary artery disease of the patients enrolled13. For example, a patient with distal a left-main stem trifurcation lesion in combination with an occluded right coronary artery is pooled together with a patient with three focal lesions in the mid portions of the three coronary arteries. Both are characterised as routinely named “3-vessel disease”, despite the fact that the first patient represents a greater therapeutic challenge for the interventional cardiologist and has completely different prognosis compared to the second patient regardless of the revascularization strategy; percutaneous or surgical. The absence of grading of the severity of coronary artery disease and the lack of comparison of lesion complexity based on pre-treatment angiographic criteria between various groups severely limits the interpretation of the results of these trials.
Thus, for the selection of the optimal revascularization strategy for patients with three vessel and/or left main stem disease there are three major requirements:
1. The conductance of an “all comer” (no exclusion criteria) study in such patients.
2. Consensus between the interventional cardiologist and the cardiothoracic surgeon for the treatment plan.
3. The quantification of the complexity of coronary artery disease, taking into account not only the number of significant lesions and their location, but also the complexity of each lesion independently.
The SYNTAX (SYNergy between PCI with TAXUS™ and Cardiac Surgery) study was organized as an all comer study for patients with significant lesions in the left main stem and/or the three epicardial coronary arteries. It will be comprised of a randomized arm and two registries for patients that are not suitable for one of the two revascularization strategies. Patients who have a preference for one of the treatment strategies or patients in whom medical treatment is suggested they will be included in the screening log.
The SYNTAX score has been developed for this study to prospectively characterise the coronary vasculature with respect to the number of lesions and their functional impact, location, and complexity. Higher SYNTAX scores, indicative of more complex disease are hypothesized to represent a bigger therapeutic challenge and to have potentially worse prognosis.
Pre-existing classifications
The SYNTAX score has been developed based on the following:
1. The AHA classification of the coronary tree segments modified for the ARTS study
2. The Leaman score
3. The ACC/AHA lesions classification system
4. The total occlusion classification system
5. The Duke and ICPS classification systems for bifurcation lesions
6. Consultation of experts
Each of these classifications has been focusing on specific functional and anatomical parameters of the lesions. Thus, the development of a global classification system that would take into account all the variables was necessary.
Definition of the coronary tree segments
The definition of the coronary tree segments is based on the classification proposed by the AHA20 and modified for the ARTS I and II trials21. By this system the arterial tree is divided in 16 segments (Figure 1) and as such has been adopted in the SYNTAX score.
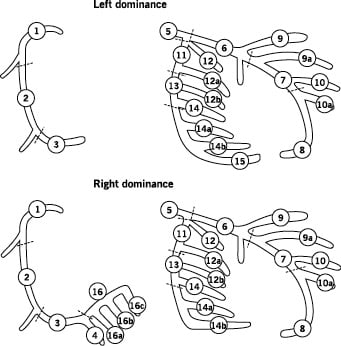
Figure 1. Definition of the coronary tree segments
1. RCA proximal: From the ostium to one half the distance to the acute margin of the heart.
2. RCA mid: From the end of first segment to acute margin of heart.
3. RCA distal: From the acute margin of the heart to the origin of the posterior descending artery.
4. Posterior descending artery: Running in the posterior interventricular groove.
16. Posterolateral branch from RCA: Posterolateral branch originating from the distal coronary artery distal to the crux.
16a. Posterolateral branch from RCA: First posterolateral branch from segment 16.
16b. Posterolateral branch from RCA: Second posterolateral branch from segment 16.
16c. Posterolateral branch from RCA: Third posterolateral branch from segment 16.
5. Left main: From the ostium of the LCA through bifurcation into left anterior descending and left circumflex branches.
6. LAD proximal: Proximal to and including first major septal branch.
7. LAD mid: LAD immediately distal to origin of first septal branch and extending to the point where LAD forms an angle (RAO view). If this angle is not identifiable this segment ends at one half the distance from the first septal to the apex of the heart.
8. LAD apical: Terminal portion of LAD, beginning at the end of previous segment and extending to or beyond the apex.
9. First diagonal: The first diagonal originating from segment 6 or 7.
9a. First diagonal a: Additional first diagonal originating from segment 6 or 7, before segment 8.
10. Second diagonal: Originating from segment 8 or the transition between segment 7 and 8.
10a. Second diagonal a: Additional second diagonal originating from segment 8.
11. Proximal circumflex artery: Main stem of circumflex from its origin of left main and including origin of first obtuse marginal branch.
12. Intermediate/anterolateral artery: Branch from trifurcating left main other than proximal LAD or LCX. It belongs to the circumflex territory.
12a. Obtuse marginal a: First side branch of circumflex running in general to the area of obtuse margin of the heart.
12b. Obtuse marginal b: Second additional branch of circumflex running in the same direction as 12.
13. Distal circumflex artery: The stem of the circumflex distal to the origin of the most distal obtuse marginal branch, and running along the posterior left atrioventricular groove. Caliber may be small or artery absent.
14. Left posterolateral: Running to the posterolateral surface of the left ventricle. May be absent or a division of obtuse marginal branch.
14a. Left posterolateral a: Distal from 14 and running in the same direction.
14b. Left posterolateral b: Distal from 14 and 14 a and running in the same direction.
15. Posterior descending: Most distal part of dominant left circumflex when present. It gives origin to septal branches. When this artery is present, segment 4 is usually absent.
Leaman score22
The ‘Leaman score’ is based on the severity of luminal diameter narrowing and weighed according to the usual blood flow to the left ventricle in each vessel or vessel segment. In a right dominant system, the right coronary artery (RCA) supplies approximately 16% and the left coronary artery (LCA) 84% of the flow to the left ventricle (LV). This 84% is normally directed for 66% to the left anterior descending artery (LAD), and for 33% into the left circumflex coronary artery (LCX). Thus, the Left Main (LM) supplies approximately 5 times, the LAD approximately 3,5 times (84/16 x 0.66) and the circumflex 1,5 times as much blood as the RCA to the left ventricle.
In a left dominant system the RCA does not contribute to the blood supply of the ventricle. Thus the LM supplies 100% of the flow to the LV. The RCA contribution of blood flow to the LV is now supplied by the LCX. Hence the LAD provides 58% (weighing factor 3.5) and the LCX 42% (weighing factor 2.5) of the total flow to the LV. Using the same principle of relative blood supply to the LV all coronary segments has been given a weighing factor factor, Table 1.
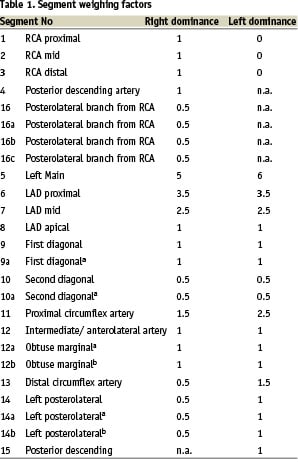
The contribution of each coronary segment to the blood flow to the LV is used as a multiplication factor for the calculation of the Leaman score and as such has been transferred to the SYNTAX score.
A lesion is defined as significant when it causes (50% reduction in luminal diameter by visual assessment in vessels (1.5mm. Less severe lesions should not be included in the SYNTAX score. The percent diameter stenosis is not considered in the algorithm. Distinction has been made only between occlusive (100% diameter stenosis) and non occlusive (50-99% diameter stenosis) disease. A multiplication factor of 2 is used for non-occlusive lesions and 5 for occlusive lesions reflecting the difficulty of the percutaneous treatment, Table 1. Importantly, all other adverse lesion characteristics considered in the SYNTAX score have an additive value, Table 2.
Multiple-tandem lesions
If multiple lesions are less than 3 vessel reference diameters apart (tandem lesion), these lesions are scored as one lesion. However, lesions at a greater distance from each other (more than 3 vessel reference diameters), are considered as separate lesions.
ACC/AHA lesion classification system23
This lesion classification system is based on parameters, such as length, eccentricity, angulation, calcification, involvement of side branches, thrombus and severity of stenosis. Lesions are classified as Type A, (high success and low risk), Type B (moderate success and moderate risk) or Type C (low success and high risk).
The majority of these individual parameters have been incorporated in the SYNTAX score (Table 2). Although the ACC/AHA system takes into account the total occlusions and the bifurcation lesions classifying them as a high-risk, it is not considered as detailed enough to adequately quantify their complexity.
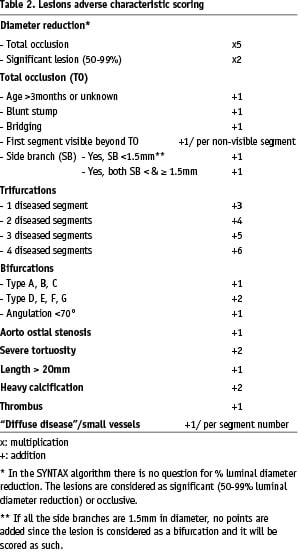
Total occlusion classification system24
A lesion is characterized as a total occlusion when no antegrade flow is visible distal to the obstruction. Segments distal to the occlusion may be filled by bridging, ipsilateral or contra-lateral collaterals.
Parameters suggested in this system such as age of the occlusion more than three months, presence of side-branch at the site of the occlusion and their size, a blunt stump, presence of bridging collaterals and occlusion length have been incorporated into the SYNTAX score, Table 2.
The length of the obstructed segment is calculated by measuring the distance between the stump of the occlusion and the first segment beyond the occlusion, visualized by ante-grade or retrograde collateral flow, Figure 2. The age of the total occlusion is scored based on history of previous infarct, worsening symptoms, previous angiographic or electrocardiographic data. In case that this information is absent the age of total occlusion is scored as unknown.
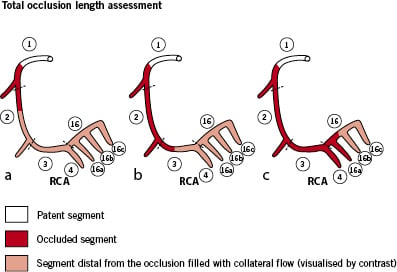
Figure 2. Total occlusion length assessment
a) Total occlusion involving segments 1 and 2. Segments 2,3,4,16,16a,16b,16c are filled by antegrade or retrograde collateral flow (visualised by contrast).
b) Total occlusion involving segments 1, 2 and 3. Segments 3,4,16,16a,16b,16c are filled by antegrade or retrograde collateral flow (visualised by contrast).
c) Total occlusion involving segments 1, 2, 3, 4, 16 and 16a Segments 16,16b,16c are visualized by antegrade or retrograde collateral flow (visualised by contrast).
Duke and ICPS bifurcation lesion classification systems
Bifurcation is defined as a junction of a main vessel and a side branch (with a minimal diameter of 1.5mm). A lesion is scored as a bifurcation, if the main vessel and/or the side branch have a narrowing. Bifurcation lesions not involving the ostium of the side branch are classified as type A if the lesion in the main vessel is proximal, type B distal and type C both proximal and distal to the side branch. Bifurcation lesions involving the ostium of the side branch are classified as type F if the lesion in the main branch is proximal, type G distal and type D both proximal and distal to the side branch. As plaque shift can occur even when only the ostium of a side branch is narrowed, such a lesion is also considered as a bifurcation (type E) (Figure 3). Bifurcations are only considered for the following segment junctions: 5/6/11, 6/7/9, 7/8/10, 11/13/12a, 13/14/14a and 3/4/16 and 13/14/15 in case of left dominance. The above mentioned classification is a combination of the Duke25 and the ICPS26 classification bifurcation systems, each proposing 6 types of bifurcations. Type G was missing from the former while type D from the latter. The combination of both constitutes the SYNTAX classification with 7 types.
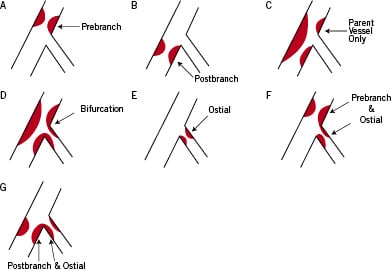
Figure 3. Bifurcation classification (modified from Duke and ICPS classifications systems)
Type A: Pre-branch stenosis not involving the ostium of the side branch.
Type B: Post side branch stenosis of the main vessel not involving the origin of the side branch.
Type C: Stenosis encompassing the side branch but not involving its ostium.
Type D: Stenosis involving the main vessel and ostium of the side branch.
Type E: Stenosis involving only the ostium of the side branch
Type F: Stenosis directly involving the main vessel (pre-side branch) and the ostium of the side branch.
Type G: Stenosis directly involving the main vessel (post-side branch) and the ostium of the side branch.
One lesion characteristic added to the bifurcation lesion classification is the angulation less than 70 degrees of the side branch with the distal main vessel. Despite the fact that this represents a less technical challenge, it is regarded as an adverse lesion characteristic due to the fact that the smaller this angle is the more difficult it will be to cover the ostium of the side branch when stenting is necessary, Figure 4.
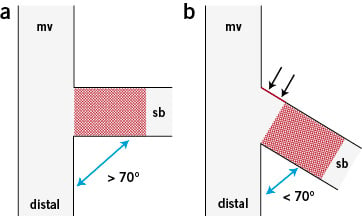
Figure 4.
a) An example of a bifurcation lesion with a wide angle (>70 degrees) between the side branch and the distal main vessel. Although technical challenging sometimes, the stent can fully cover both the proximal and distal rims of the side branch ostium. b) An example of a bifurcation with a steep angle (<70 degrees) between the side branch and the distal main vessel. Side branch stenting might be technically less challenging compared to the previous anatomy but when the stent is placed to cover the distal rim of the ostium the proximal rim will remain uncovered (red line with arrows). If the stent is placed to cover the proximal rim it will protrude into the main vessel distally.
mv denotes main vessel, sb denotes side branch.
Trifurcation lesions
Trifurcation is a junction of three branches, one main vessel and two side branches (with a minimal diameter of 1.5mm). In a trifurcation, one, two, three or four of the involved segments can be diseased. The most common example of a trifurcation is at the division of LM into the LAD, LCX, and an intermediate branch. Trifurcations are only scored for the following segment junctions: 3/4/16/16a, 5/6/11/12, 11/12a/12b/13, 6/7/9/9a and 7/8/10/10a, Table 2.
Aorto-ostial lesions
A lesion is classified as aorto-ostial when it is located immediately at the origin of the coronary arteries from the aorta. It applies only to segments 1 and 5. In case of absence of a LM (double ostium of the Left Coronary Artery), the segments 6 of the LAD and 11 of the LCX originate directly from the aorta and consequently may also involve aorto-ostial lesions. Aorto-ostial location is regarded as an adverse characteristic since the treatment of such lesions is technically more challenging.
Diffuse disease/Small vessels
Present when at least 75% of the length of the segment distal to the lesion has a vessel diameter of <2mm, irrespective of the presence or absence of disease at that distal segment. It is a parameter introduced to reflect the more challenging creation of a surgical anastomosis in small or diseased vessels.
The SYNTAX score algorithm (Table 3)
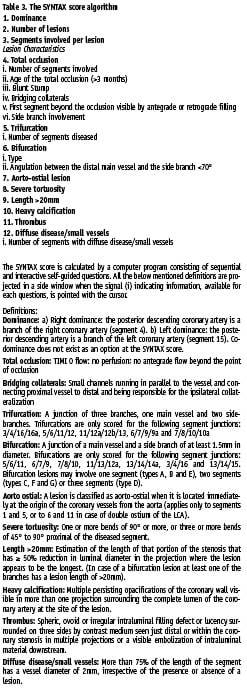
The SYNTAX score is calculated by a computer program consisting of sequential and interactive self-guided questions. The algorithm consists of twelve main questions. They can be divided in two groups:
The first three determine the dominance, the total number of lesions and the vessel segments involved per lesion and they appear once. The maximum number of lesions allowed is twelve and each lesion is characterized by a number, 1 to 12. The lesions will be scored in the numerical order inserted in question 3. Each lesion can involve one or more segments. In this case each vessel segment involved contributes to the lesion scoring. There is no limit in the number of segments involved per lesion.
The last nine questions refer to adverse lesion characteristics and are repeated for each lesion.
The question referring to a total occlusion is the first one. If a total occlusion is scored, answers must be given to detailed sub-questions. The last of these sub-questions refers to the presence or absence of side branches and their size. If there are no side branches or if their diameter is <1.5 mm then the questions related to the trifurcation and bifurcation lesions will be automatically skipped since vessels <1.5 mm are not considered large enough for treatment either with PCI or CABG. If side branches with diameter 1.5 mm are involved then the lesion is considered as both total occlusion and bifurcation lesion and the algorithm will continue with all the questions. The same is the case for non-occlusive lesions.
With the exception of the selection of the type in case of a bifurcation or a trifurcation lesion all the other questions of the algorithm can be answered by selecting “yes” or “no”.
The last question of the algorithm, diffuse disease/small vessels, is the only one non-lesion-specific since it is related to vessel anatomy beyond the stenosis. In case of positive answer all the coronary segments beyond the one under scoring will appear allowing the selection of these fulfilling the criteria for diffuse disease/small vessels. It is quoted once (the first time selected) per coronary territory (RCA, LM, LAD, LCX). If for example this question is answered during a LM lesion scoring it will not reappear for lesions in the LAD or LCX territory. The same is the case for multiple lesions in the same vessel. Since the lesions are scored in the numerical order inserted in question 3, a scoring in “anatomical order” from proximal to distal is advised for each coronary artery. For example a lesion in segment 2 of the RCA should be scored before a lesion located in more distal segments.
An important characteristic of the SYNTAX score is that it is lesion based. For each lesion a separate score is calculated. The total SYNTAX score is derived from the summation of these individual scorings.
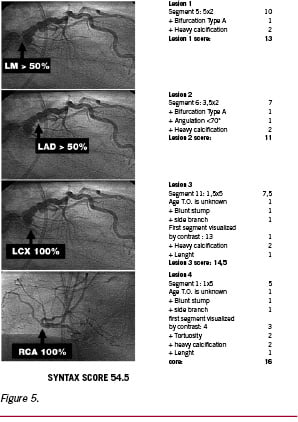
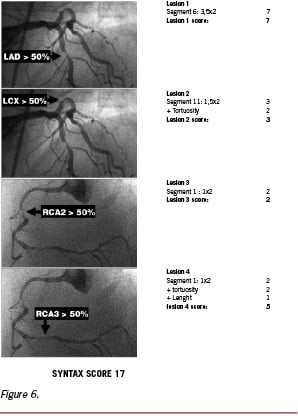
After the completion of the algorithm a report is automatically generated summarizing all the adverse characteristics, and the individual scoring of each lesion as well as the total SYNTAX score. Two examples of the SYNTAX score calculation are presented in Figures 5, 6. Both patients have significant stenosis in all three coronary arteries with four lesions each but the calculated SYNTAX score differs greatly (54.5 versus 17) reflecting the more complex pattern of coronary artery disease in the patient with the higher score.
Validation
The utility of the SYNTAX score for predicting outcomes will be examined at three junctures in the conduct of the trial:
1. In phase I it will be evaluated based on patient allocation into the 3 study arms (randomized, PCI registry and CABG registry).
2. In phase II its utility at predicting early procedural outcomes (30 days) will be assessed and optimised.
3. In phase III it will be evaluated and the scoring will be optimized for predicting 1, 3 and 5 year outcomes.
Summary
The most important characteristic of the SYNTAX score to be emphasized is that it is focusing on anatomy of coronary vasculature and not on treatment plan.
The ultimate goal is to create an angiographic tool grading the complexity of coronary artery disease and obtain evidence based guidelines for selecting the optimal technique of revascularization (CABG or PCI). In addition it will allow comparison of coronary artery disease complexity in individual patients and entire patient cohorts, as well as assessment of adequacy and completeness of revascularisation.
In summary it’s a score under investigation to predict prognosis based on disease complexity in coronary vasculature. It will be retroactively weighted based on clinical outcomes and potentially revised to optimize its prognostic value. Once validated and standardised the SYNTAX score will become available on-line.

